Medicaid covers TMS only in Washington state at this time. Meritain Health Tricare. TMS is covered on an outpatient basis. United Healthcare.
Full Answer
Is TMS covered by Medicare?
TMS is covered by Medicare if prescribed and administered by a licensed physician like Dr. Bruno at Mid City TMS who accepts Medicare and is knowledgeable in the use of Transcranial Magnetic Stimulation. TMS is indicated for patients with Major Depressive Disorder who have failed to benefit from initial treatment of their depression.
How much does TMS treatment cost?
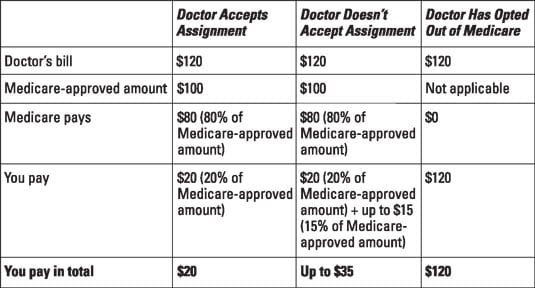
Each TMS session generally costs between $400 and $500. If your treatment is approved, you may be responsible for paying 20 percent of this cost for each session you undergo. Before deciding to pursue TMS treatment, check to see what your specific Medicare plan covers.
Does Medicare cover transcranial magnetic stimulation?
Medicare does in fact cover transcranial magnetic stimulation (TMS) treatments. When treated by licensed, Medicare-approved physicians such as Dr. Bryan Bruno, the Medical Director at Mid City TMS, who are proficient in the administration of TMS, a patient with Medicare is eligible to receive full coverage for the procedures.
Does TMS work for everyone?
Medications do not always work for everyone, and TMS provides an alternative therapy option for individuals seeking relief. TMS can be used as a primary treatment in some cases, but many individuals opt for antidepressant prescriptions initially. TMS treatment is associated with very few side effects.
Does Medicare cover maintenance TMS?
If you're 65 years or older and suffer from depression, you may have wondered, “Does Medicare cover TMS?” Medicare does in fact cover transcranial magnetic stimulation (TMS) treatments.
Does Medicare cover TMS for anxiety?
Is TMS Therapy Covered by Medicare or Medicaid? The short answer is yes, but coverage may vary depending on your specific Medicare or Medicaid plan. If all requirements are met, Medicare may pay for 80% of the treatment cost.
What qualifies you for TMS?
The patient must have a DSM diagnosis of F33. 2 (Recurrent Depressive Disorder, Current Episode Severe Without Psychotic Symptoms) or F32. 2 (Severe Depressive Episode Without Psychotic Symptoms). The severity of depression required, as measured by a clinical rating scale, differs by insurance plan.
Is TMS covered by Medicaid in NY?
Patients frequently contact our office and ask whether their New York state Medicaid plan will cover TMS. Unfortunately, our answer is always “not yet.” As of 2019, Medicaid covers several different treatments for depression – including medication and talk therapy – but TMS is not on the list of treatments covered.
Can TMS make anxiety worse?
Can TMS Make Anxiety Worse? Some studies have shown that when TMS is used to treat depression, anxiety symptoms can increase. However, anxiety is not listed as a side effect of TMS therapy, and there is no evidence to show that TMS makes anxiety worse.
Is electromagnetic therapy covered by insurance?
Unsupervised use of ES or electromagnetic therapy for wound therapy will not be covered, as this use has not been found to be medically reasonable and necessary.
Who is not a candidate for TMS?
Individuals have generally failed 2-4 medication trials before starting TMS. You're not satisfied with the results you get from your medication(s) You cannot tolerate the side effects of your medication(s) You have an illness that limits your ability to take medications for depression.
Who should not get TMS?
Patients less than 18 years of age or older than 68 years of age. Patients with a history of substance abuse. Patients with a psychotic disorder, such as schizophrenic disorder, schizoaffective disorder, bipolar disease, or major depression with psychotic features.
What is the success rate of TMS therapy?
Does TMS work? Approximately 50% to 60% of people with depression who have tried and failed to receive benefit from medications experience a clinically meaningful response with TMS. About one-third of these individuals experience a full remission, meaning that their symptoms go away completely.
What is TMS treatment for depression?
Transcranial magnetic stimulation (TMS) is a noninvasive procedure that uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of depression. TMS is typically used when other depression treatments haven't been effective.
What is transcranial magnetic stimulation (TMS)?
TMS is a fairly new form of therapy, which has shown success in treating patients with depression, OCD, and bipolar disorder. The process involves...
Does Medicare Cover TMS therapy?
Medicare does not cover TMS therapies, claiming that the technology’s effectiveness has not sufficiently been studied. Note, however, that this ver...
Does Medicare cover alternatives to TMS?
Medicare covers a number of treatments for depression. Medicare Part D plans cover prescription antidepressant medications such as SSRIs. In additi...
What is Transcranial Magnetic Stimulation (TMS)?
TMS is a relatively new treatment for severe major depressive disorder. It uses magnetic fields to stimulate nerve cells in areas of the prefrontal cortex linked to mood regulation.
Does Medicare cover TMS Therapy?
While most major insurance companies cover TMS for depression treatment, Medicare, unfortunately, does not cover TMS therapy at all.
Frequently Asked Questions
TMS is a fairly new form of therapy, which has shown success in treating patients with depression, OCD, and bipolar disorder. The process involves using a wand-like device called a TMS coil to discharge high-intensity magnetic pulses near various areas of the prefrontal cortex—the area associated with mood regulation.
Conclusion
Transcranial Magnetic Stimulation therapy is an exciting treatment choice for major depressive disorder and other severe mental health conditions. Unfortunately, because of how new the technology is, government programs like Medicare do not cover it.
TMS is one of the most effective treatments for depression, especially for patients who have failed to achieve a positive response from antidepressants and therapy
Depression is one of the most prevalent mental health disorders worldwide, affecting over 280 million people around the world. Characterized as a mood disorder, depression is often experienced as having persistent feelings of sadness and disinterest in daily activities.
What is TMS?
Transcranial magnetic stimulation (TMS) is a noninvasive procedure that uses magnetic fields to stimulate nerve cells in the brain in order to improve symptoms of mental disorders like depression.
Does Medicare Cover TMS Treatments?
Yes! Medicare has started offering coverage for TMS treatments due to the treatment’s success rates with patients. In order to be eligible for coverage, the patient must be diagnosed with severe major depressive disorder by a Medicare-approved physician.
I don't have Medicare, will my insurance cover TMS Treatments?
The short answer is yes, although as a rule, insurance companies will not pay for a service or procedure unless they consider it medically necessary or appropriate.
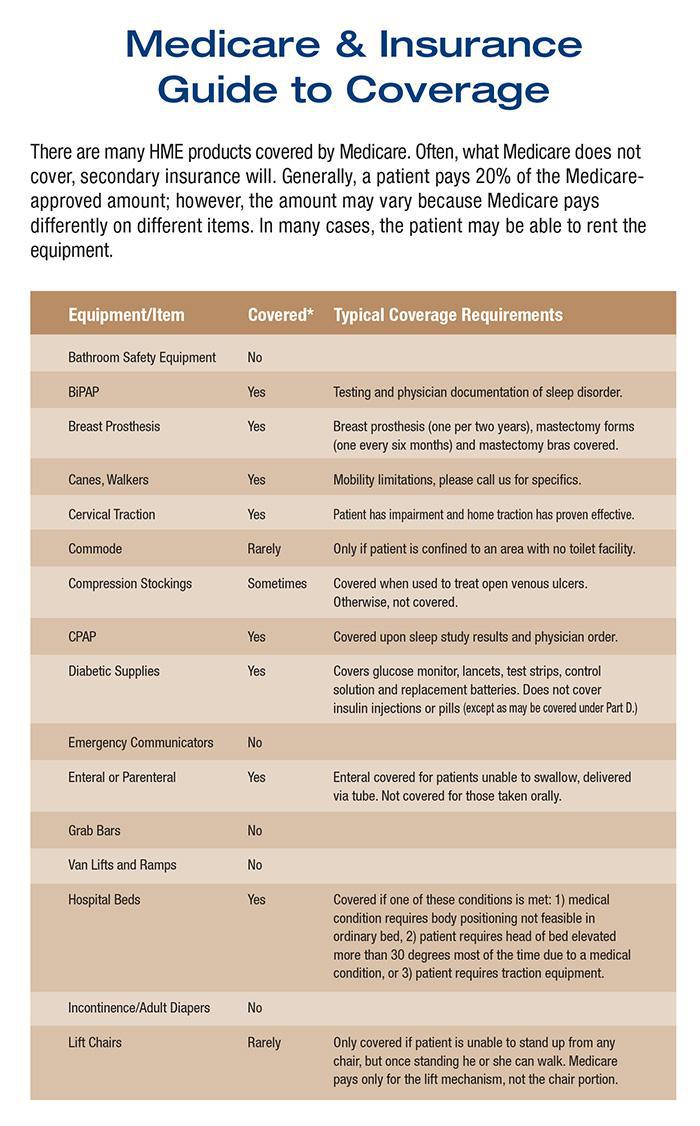
Insurance companies that cover TMS therapy
TMS therapy is covered by most insurance companies. Many insurance companies pay for TMS therapy for depression because it’s effective and FDA-approved for the treatment of major depressive disorder. Image courtesy of bostonscientific.com.
What are the limitations of TMS?
There are certain circumstances that will limit a patient’s ability to receive Medicare coverage for their TMS treatments, including: 1 Psychotic symptoms in the current depressive episode. 2 History of seizures 3 The following Neurological conditions: epilepsy, cerebrovascular disease, dementia, increased intracranial pressure or a history of repetitive or severe head trauma 4 Presence of an implanted magnetic-sensitive items located within 30 centimeters from the TMS magnetic coil
What is TMS in medical terms?
TMS, transcranial magnetic stimulation, is a noninvasive medical procedure that utilizes magnetic fields to generate electric currents in regions of the brain. An electromagnetic coil is strategically positioned against a patient’s scalp near their forehead to target a region of the brain involved with mood.
What are the conditions that can cause neurologic problems?
The following Neurological conditions: epilepsy, cerebrovascular disease, dementia, increased intracranial pressure or a history of repetitive or severe head trauma
How many people have depression in the US?
In 2017, the National Institute of Mental Health (NIMH) estimated that 17.3 million adults in the United States had at least one major depressive episode during a typical year.
Does Medicare cover TMS in NYC?
When patients 65 years or older are prescribed to TMS treatments at Mid City TMS, many of them often ask “Does Medicare cover TMS treatments?” and luckily there is Medicare coverage available for TMS in NYC.
Does TMS require anesthesia?
The TMS procedure doesn’t require anesthesia or analgesia and is typically performed in an outpatient setting. Since the magnetic stimulation is focal and non-systemic, TMS usually has no side effects and doesn’t cause memory loss or seizures like electroconvulsive therapy (ECT).
Who is the medical director of Mid City TMS?
When treated by licensed, Medicare-approved physicians such as Dr. Bryan Bruno , the Medical Director at Mid City TMS, who are proficient in the administration of TMS, a patient with Medicare is eligible to receive full coverage for the procedures.
Get In Touch With Tms Institute Of Americatoday To Get An Exact Understanding Of The Benefits Associated With Your Specific Insurance Plan We Are An In
Most major insurance will cover the cost of TMS therapy every six months providing specific criteria is met. Each insurance has its own set of guidelines, but generally the basic criteria includes:
Tms For Conditions Other Than Depression
TMS is a safe and effective treatment for many However, insurance providers generally do not yet cover the cost of TMS therapy for the following conditions:
What Are The Most Common Side Effects Of Tms
The most common side effects of TMS are scalp discomfort and headache.
What Treatment For Depression Is Available
Depression treatment takes a variety of forms, depending on the cause and severity of the problem. The most common types of treatment for depression include:
Madison Ave Tms & Psychiatry Accepts All Major Insurance Plans That Offer Coverage For Tms
In addition to accepting Medicare, we also accept all major insurance plans that cover costs associated with TMS. See which insurance plans we accept.
Am I Eligible For Tms Therapy
For people with depression who have not benefited from antidepressant medication, TMS therapy can offer hope for long-lasting relief of symptoms. If you agree with two or more of these statements, TMS therapy may be right for you.
Contraindications For Tms Therapy
Some things can prevent you from being a candidate for TMS therapy. There is a strong magnetic field produced with TMS, so you wont be able to have it done if you:
What brain areas are affected by rTMS?
Twenty studies met inclusion criteria with 19 using rTMS and one dTMS. All but one of the rTMS trials are included in the meta-analyses described above. Included brain areas were the dorsolateral prefrontal cortex (DLPFC), supplementary motor area (SMA), orbitofrontal/medial prefrontal cortex (OFC), and anterior cingulate cortex (ACC). Frequency stimulation was low (1 Hz) or high (>/=5 Hz). Treatment duration varied from two to six weeks with follow-up ranging from none to three months. Three tables listed 16 of the studies. Nine had Y-BOCS score reductions with rTMS versus sham; eight showed no significant difference. Summaries of dTMS studies follow. The authors concluded treatment of OCD with neurostimulation shows promise, but it is yet to be determined how best to optimize the approach using rTMS or dTMS to achieve clinically relevant results.
Is DTMS covered by OCD?
Based on a reconsideration request received April 2019 to allow coverage of dTMS for obsessive compulsive disorder (OCD), the following literature has been reviewed and added. In addition, literature to examine the use of rTMS for OCD has also been included.
What does "you" mean when acting on behalf of an organization?
If you are acting on behalf of an organization, you represent that you are authorized to act on behalf of such organization and that your acceptance of the terms of this agreement creates a legally enforceable obligation of the organization. As used herein, “you” and “your” refer to you and any organization on behalf of which you are acting.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Local Coverage Determinations (LCDs). CMS believes that the Internet is an effective method to share LCDs that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
Is rtms FDA approved?
The rTMS treatment is delivered by a device that is FDA-approved or –cleared for the treatment of MDD in a safe and effective manner. rTMS treatment should generally follow the protocol and parameters specified in the manufacturer’s user manual, with modifications only as supported by the published scientific evidence base; and
Is rTMS a less invasive treatment?
History of response to electroconvulsive therapy (ECT) in a previous or current MDD episode, or inability to tolerate ECT, and rTMS is considered a less invasive treatment option; and
What are the conditions that affect the central nervous system?
Neurologic conditions that include epilepsy, cerebrovascular disease, dementia, increased intracranial pressure, having a history of repetitive or severe head trauma, or with primary or secondary tumors in the central nervous system ;
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Articles. CMS believes that the Internet is an effective method to share Articles that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
What is a local coverage article?
Local Coverage Articles are a type of educational document published by the Medicare Administrative Contractors (MACs). Articles often contain coding or other guidelines that are related to a Local Coverage Determination (LCD).
Does CMS have a CDT license?
Organizations who contract with CMS acknowledge that they may have a commercial CDT license with the ADA, and that use of CDT codes as permitted herein for the administration of CMS programs does not extend to any other programs or services the organization may administer and royalties dues for the use of the CDT codes are governed by their commercial license.
What is a bill and coding article?
Billing and Coding articles provide guidance for the related Local Coverage Determination (LCD) and assist providers in submitting correct claims for payment. Billing and Coding articles typically include CPT/HCPCS procedure codes, ICD-10-CM diagnosis codes, as well as Bill Type, Revenue, and CPT/HCPCS Modifier codes. The code lists in the article help explain which services (procedures) the related LCD applies to, the diagnosis codes for which the service is covered, or for which the service is not considered reasonable and necessary and therefore not covered.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
What does "you" mean when acting on behalf of an organization?
If you are acting on behalf of an organization, you represent that you are authorized to act on behalf of such organization and that your acceptance of the terms of this agreement creates a legally enforceable obligation of the organization. As used herein, “you” and “your” refer to you and any organization on behalf of which you are acting.
How to check if my insurance covers TMS?
To check on insurance coverage for TMS, you can either reach out directly to a TMS provider or contact your insurance company. Some insurance providers also have online, searchable directories of in-network medical services. Those receiving Medicare or Medicaid should check to make sure their state provides coverage for TMS specifically. If your state offers no insurance coverage for TMS treatment, don’t be afraid to contact state and local representatives to advocate for mental health coverage options.
What is the TMS treatment?
November 30, 2020. ... Transcranial magnetic stimulation is an alternative psychiatric treatment method that uses electromagnetic pulses delivered through a device coil to target areas of irregular brain activity. TMS is most effective for those with mental disorder symptoms that have proven to be resistant to psychiatric medications.
How to be awake during TMS?
Be energized and awake. It’s essential that a TMS patient remains awake and alert during treatment sessions. The brain must be as alert as possible in order for the TMS device’s pulses to be effective. Be prepared to be up and energized prior to your sessions. Consider talking during treatment.
What is a TMS coil?
The device used to deliver TMS pulses uses a coil to safely and effectively target areas of irregular brain chemistry in the patient. During the average TMS session, the TMS device’s coil is first placed above the seated patient’s head.
What is TMS in psychology?
TMS modifies brain activity to alter communication between neurons, subsequently influencing various brain functions. Mood regulation and other executive functions are typically the targets of TMS pulses. With electromagnetic pulses permeating the skull to reach the brain, TMS is effective in reducing symptom severity in major depression, anxiety disorders, and other mental health conditions.
Why do TMS patients wear earbuds?
It’s best for TMS patients to wear earbuds during each session to reduce the potential discomfort in response to the device’s clicking noises. Following each electromagnetic pulse, neuronal activity and communication is promoted in the brain.
What to do if you don't have insurance for TMS?
If your state offers no insurance coverage for TMS treatment, don’t be afraid to contact state and local representatives to advocate for mental health coverage options. For those struggling to find in-network TMS providers, some insurers may use what’s called a “carve-out plan.”.
