Most people get Part A for free, but some have to pay a premium for this coverage. To be eligible for premium-free Part A, an individual must be entitled to receive Medicare based on their own earnings or those of a spouse, parent, or child.
What is a Medicare Advantage plan?
Medicare Advantage Plans are another way to get your Medicare Part A and Part B coverage. Medicare Advantage Plans, sometimes called “Part C” or “MA Plans,” are offered by Medicare-approved private companies that must follow rules set by Medicare.
Do Medicare Advantage plans include OTP?
Medicare Advantage (MA) plans must include the OTP benefit as of January 1, 2020 and contract with OTP providers in their service area, or agree to pay an OTP on a non-contract basis. In covering the OTP benefit, MA plans must use only Medicare-enrolled OTP providers. MA Plans & OTP Payment
Do I still have Medicare if I join a Medicare Advantage plan?
If you join a Medicare Advantage Plan, you’ll still have Medicare but you’ll get most of your Part A and Part B coverage from your Medicare Advantage Plan, not Original Medicare.
What is the difference between Original Medicare and Medicare Advantage?
Medicare Advantage (also known as “Part C”) is an “all in one” alternative to Original Medicare. These “bundled” plans include Part A, Part B, and usually Part D. Most plans offer extra benefits Original Medicare doesn’t cover–like vision, hearing, dental, and more.
How are Medicare Advantage plans regulated?
The private health plans are known as Medicare Advantage plans and are regulated and reimbursed by the federal government. MA plans combine Part A and Part B and oftentimes Part D, into one plan so your entire package of benefits comes from a private insurance company.
Can you be denied a Medicare Advantage Plan?
Generally, if you're eligible for Original Medicare (Part A and Part B), you can't be denied enrollment into a Medicare Advantage plan. If a Medicare Advantage plan gave you prior approval for a medical service, it can't deny you coverage later due to lack of medical necessity.
Does CMS regulate Medicare Advantage plans?
The Centers for Medicare & Medicaid Services (CMS) released a regulation that clarifies the payment of compensation to agents and brokers who enroll beneficiaries in Medicare Advantage and Prescription Drug Plans. Copies of the new regulations and related documents can be downloaded from below.
Who decides Medicare coverage?
Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
Do Medicare Advantage plans have underwriting?
Because Advantage plans have no medical underwriting, the insurer must accept you. Many of these plans have extra perks, such as dental, vision or hearing coverage, that original Medicare doesn't provide.
Can I switch from a Medicare Advantage plan back to Original Medicare?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
Who is the largest Medicare Advantage provider?
AARP/UnitedHealthcareAARP/UnitedHealthcare is the most popular Medicare Advantage provider with many enrollees valuing its combination of good ratings, affordable premiums and add-on benefits. For many people, AARP/UnitedHealthcare Medicare Advantage plans fall into the sweet spot for having good benefits at an affordable price.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
How does CMS define a Medicare Advantage Plan?
Medicare Advantage plans are approved by Medicare but are run by private companies. These companies provide Medicare Part A and Part B covered services and may include Medicare drug coverage too. Medicare Advantage plans are sometimes called “Part C” or “MA” plans. MA plans are not supplemental insurance.
What is CMS approval?
CMS approvals are issued at a local level by the Medicare Administrative Contractor (MAC) or are reviewed an approved through a centralized process by CMS. Studies approved through the centralized process are listed here.
What is the difference between Medicare and Medicare Advantage plans?
Medicare Advantage is an “all in one” alternative to Original Medicare. These “bundled” plans include Part A, Part B, and usually Part D. Plans may have lower out-of- pocket costs than Original Medicare. In many cases, you'll need to use doctors who are in the plan's network.
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
When does Medicare Advantage plan include OTP?
Medicare Advantage Plans. Medicare Advantage (MA) plans must include the OTP benefit as of January 1, 2020 and contract with OTP providers in their service area, or agree to pay an OTP on a non-contract basis.
What should an OTP do with a MA plan?
OTPs should contact MA plans and ask for “provider services” to help with questions about payment for OTP services under that MA plan. If you’re not sure if your Medicare patient is enrolled in an MA plan:
Does MA have to use Medicare OTP?
In covering the OTP benefit, MA plans must use only Medicare-enrolled OTP providers. Regardless of whether an OTP is under contract with an MA plan or rendering services on a non-contract basis, the OTP must contact each specific plan with payment questions.
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
Can a provider bill you for PFFS?
The provider shouldn’t provide services to you except in emergencies, and you’ll need to find another provider that will accept the PFFS plan .However, if the provider chooses to treat you, then they can only bill you for plan-allowed cost sharing. They must bill the plan for your covered services. You’re only required to pay the copayment or coinsurance the plan allows for the types of services you get at the time of the service. You may have to pay an additional amount (up to 15% more) if the plan allows providers to “balance bill” (when a provider bills you for the difference between the provider’s charge and the allowed amount).
What is Medicare Advantage?
Most Medicare Advantage Plans offer coverage for things that aren't covered by Original Medicare, like vision, hearing, dental, and wellness programs (like gym memberships). Plans can also cover more extra benefits than they have in the past, including services like transportation to doctor visits, over-the-counter drugs, adult day-care services, ...
What happens if you have a Medicare Advantage Plan?
If you have a Medicare Advantage Plan, you have the right to an organization determination to see if a service, drug, or supply is covered. Contact your plan to get one and follow the instructions to file a timely appeal. You also may get plan directed care.
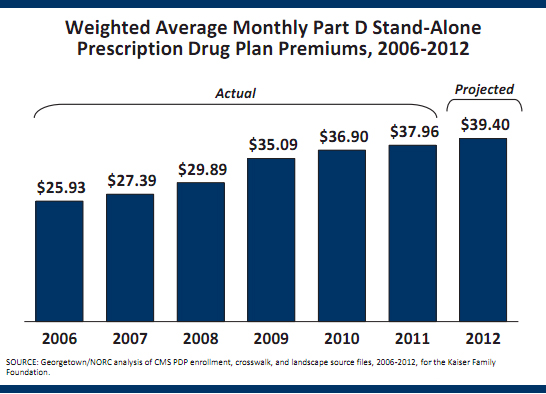
How much is Medicare Advantage 2021?
In addition to your Part B premium, you usually pay a monthly premium for the Medicare Advantage Plan. In 2021, the standard Part B premium amount is $148.50 (or higher depending on your income). If you need a service that the plan says isn't medically necessary, you may have to pay all the costs of the service.
What is Medicare health care?
Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine. under Medicare. If you're not sure whether a service is covered, check with your provider before you get the service.
Is Medicare Advantage covered for emergency care?
In all types of Medicare Advantage Plans, you're always covered for emergency and. Care that you get outside of your Medicare health plan's service area for a sudden illness or injury that needs medical care right away but isn’t life threatening.
Does Medicare cover hospice?
Medicare Advantage Plans must cover all of the services that Original Medicare covers. However, if you’re in a Medicare Advantage Plan, Original Medicare will still cover the cost for hospice care, some new Medicare benefits, and some costs for clinical research studies. In all types of Medicare Advantage Plans, you're always covered for emergency and Urgently needed care.
