Does Medicare Cover My Children?
- Social Security Disability Insurance (SSDI) recipient. ...
- Railroad Retirement Board (RRB) recipient. ...
- Individuals with amyotrophic lateral sclerosis (ALS) Individuals with ALS, also referred to as Lou Gehrig’s disease, can be enrolled in Original Medicare automatically once an individual starts receiving SSDI benefit ...
- People who are 65 or older.
- Certain younger people with disabilities.
- People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What medications are not covered by Medicare?
Some examples of medications that may not be covered by Medicare include: Weight loss or weight gain medications Medications used to treat cold or cough symptoms Fertility medications Vitamins and minerals (with the exception of prenatal vitamins or fluoride preparation products) Medications used ...
What kind of patients are covered under Medicare?
Some of the requirements may include:
- You must be under the care of a doctor, who must have a plan of care for you that she or he regularly reviews.
- The in-home health agency must be Medicare-approved.
- Your doctor must certify that you’re unable to leave your home without some difficulty – for example, you might need transportation and/or help from a cane, a walker, a wheelchair, ...
Which medical services are covered by Medicare?
Medicare Services Medicare Part A and Part B cover a variety of services, including inpatient hospital care, skilled nursing care, preventive services, home health care and ambulance transportation. Additional services such as vision and dental care may be available through a Medicare Advantage plan. Get a Free 2022 Open Enrollment Guide
What items are not covered by Medicaid?
Some of the items and services that Medicaid does not cover include: Services that have been deemed by the peer review organization, DHS, Dental, or Optometric specialist not to be clinically essential. Services that are provided by direct relatives or members of the beneficiary’s home. Home remedies, nutritional supplements, vitamins ...

Who is eligible for coverage under Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
Who would not be covered under Medicare?
Some of the items and services Medicare doesn't cover include:Long-Term Care. ... Most dental care.Eye exams related to prescribing glasses.Dentures.Cosmetic surgery.Acupuncture.Hearing aids and exams for fitting them.Routine foot care.
Do I automatically get Medicare when I turn 65?
You automatically get Medicare when you turn 65 Part A covers inpatient hospital stays, skilled nursing facility care, hospice care, and some home health care. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
What is the difference between Medicare and Medicaid?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
Medicare Advantage (Part C)
You pay for services as you get them. When you get a covered service, Medicare pays part of the cost and you pay your share.
You can add
You join a Medicare-approved plan from a private company that offers an alternative to Original Medicare for your health and drug coverage.
Most plans include
Some extra benefits (that Original Medicare doesn’t cover – like vision, hearing, and dental services)
Medicare drug coverage (Part D)
If you chose Original Medicare and want to add drug coverage, you can join a separate Medicare drug plan. Medicare drug coverage is optional. It’s available to everyone with Medicare.
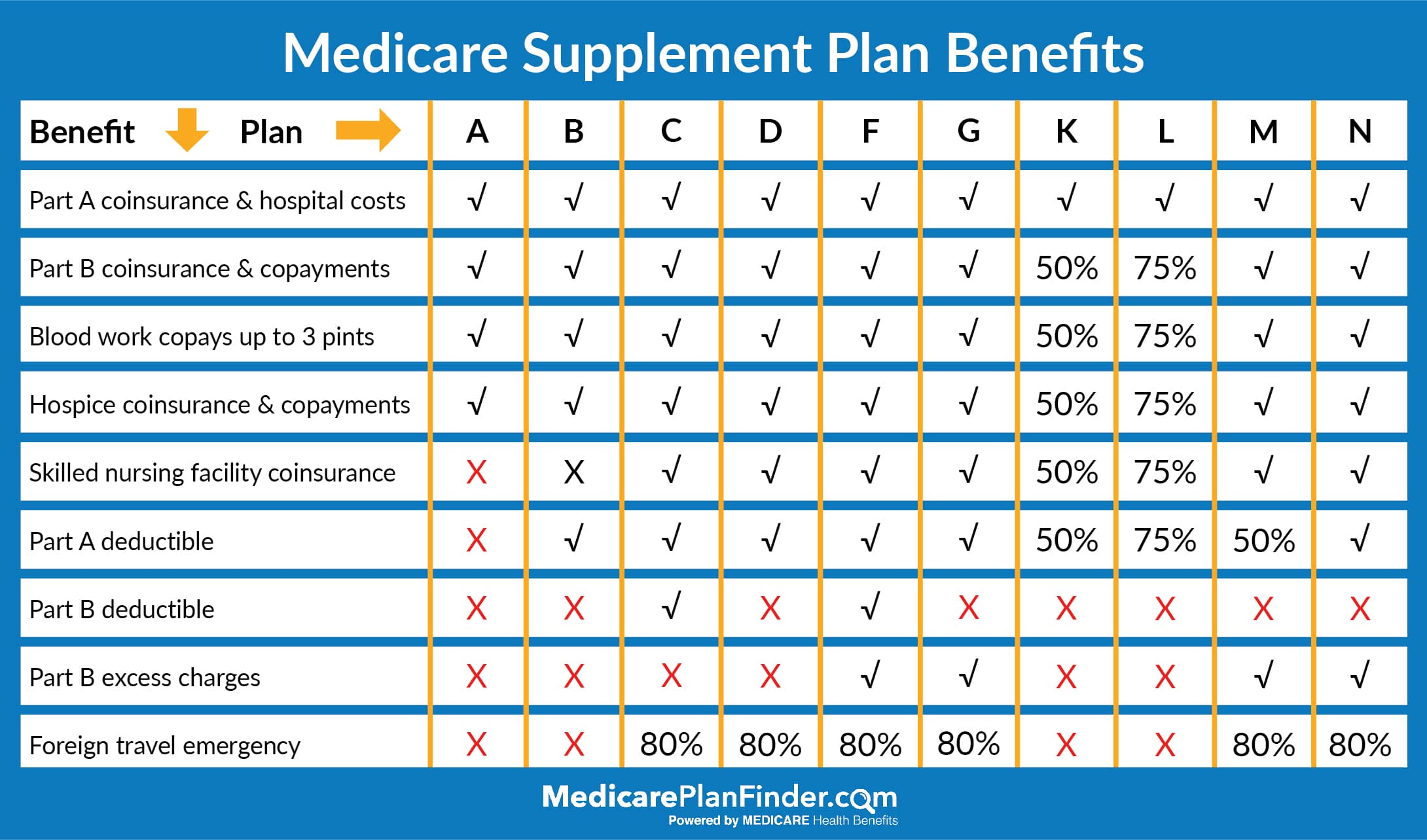
Medicare Supplement Insurance (Medigap)
Medicare Supplement Insurance (Medigap) is extra insurance you can buy from a private company that helps pay your share of costs in Original Medicare.
What are the requirements for Medicare?
Individuals under the age of 65 can qualify for Medicare under these specific conditions: 1 Social Security Disability Insurance (SSDI) recipient. Individuals receiving SSDI will be automatically enrolled in Original Medicare after 24 months of consecutive benefit payments. 2 Railroad Retirement Board (RRB) recipient. Individuals receiving RRB benefits will be automatically enrolled in Original Medicare after 24 months of consecutive benefit payments. 3 Individuals with amyotrophic lateral sclerosis (ALS). Individuals with ALS, also referred to as Lou Gehrig’s disease, can be enrolled in Original Medicare automatically once an individual starts receiving SSDI benefit payments. 4 Individuals who have end-stage renal disease (ESRD). Individuals sign up for Original Medicare through their local Social Security office.
How old do you have to be to get medicare?
Medicare Recipients Over the Age of 65. Most people become eligible for Medicare when they turn 65 years of age, as long as they are an American citizen or have lived in the U.S. as a legal permanent resident for five consecutive years or more.
How long does it take to get Medicare if you are 65?
Individuals receiving SSDI will be automatically enrolled in Original Medicare after 24 months of consecutive benefit payments. Railroad Retirement Board (RRB) recipient.
Can dependents get Medicare if they lose their health insurance?
If your dependents have lost coverage from your employee health insurance due to your transition to Medicare , they may be eligible for this temporary form of insurance. Private insurance. There are a variety of private health insurance companies with plans that can cover anyone in your household who is not eligible for Medicare benefits. CHIP. ...
Can I get Medicare if I have Lou Gehrig's disease?
Individuals with ALS, also referred to as Lou Gehrig’s disease, can be enrolled in Original Medicare automatically once an individual starts receiving SSDI benefit payments. Individuals who have end-stage renal disease (ESRD).
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What are the factors that determine Medicare coverage?
Medicare coverage is based on 3 main factors 1 Federal and state laws. 2 National coverage decisions made by Medicare about whether something is covered. 3 Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
How long do you have to be disabled to get medicare?
Children over the age of 20 must be disabled and receiving disability benefits for two years before applying for Medicare. They qualify for Medicare due to disability if disabled prior to turning 22 years old.
How long does a child have to work to get medicare?
If your child continues to work after the trial work period ends, Medicare will continue for over seven years. After that, your child will be considered a Medicare enrollee instead ...
How long does it take for a child to get medicare?
Medicare Waiting Period for Children. Often there’s a two-year waiting period for Medicare coverage for kids with disabilities. If your child was born with a disability, you’ll have to wait until the child’s second birthday to receive Medicare. However, children with ESRD or Lou Gehrig’s disease have no waiting period for Medicare.
Can a child be a Medicare beneficiary?
After that, your child will be considered a Medicare enrollee instead of a Medicare beneficiary. This means your child will be required to start paying for continued Medicare coverage.
Can a child with ESRD be on Medicare Advantage?
In certain cases, your child may be able to enroll in a Medicare Advantage Special Needs Plan ( SNP ). Depending on where you live will determine if this program is available to your child with ESRD. Medicare Advantage SNPs have certain conditions that need to be met to qualify for eligibility.
Can a child be eligible for medicaid?
Eligible for Medicaid. If your kid qualifies for Medicare due to a disability, they can join a Medicare Advantage plan.
Can a kid be on Medicare?
Any kid who is eligible for Medicare may join a Medicare prescription drug plan. These plans work paired with Original Medicare or as part of a Medicare Advantage plan.SNPs include coverage for medical treatments and medications necessary to manage a certain condition, like ESRD.
How old do you have to be to get Medicare?
In a case such as this, you must be at least 62 years old.
How long do you have to work to qualify for Medicare?
In the United States, as soon as you turn 65 you are eligible for Medicare benefits if you are citizen or have been a legal resident for five years or more and have worked for at least 40 quarters (10 years) paying federal taxes.
Can you get Medicare at different ages?
If you and your spouse are different ages, you will likely become eligible at different times. Primary Medicare recipients and their non-insured spouses are entitled to the same benefits under Medicare if both have reached the age of 65.
Do you have to enroll in Medicare Part B or D?
If you wish to sign up for Medicare Part B (Medical Insurance), and/or Part D (prescription drug insurance), you must enroll separately during your initial enrollment period, Open Enrollment or during Special Enrollment Period to avoid paying late enrollment penalties.
