What if I am dual eligible for Medicare and Medicaid?
If you are dual eligible for Medicare and Medicaid, you may be able to apply for a Medicare Supplement (Medigap) plan that’s available where you live. A Medigap plan can help pay for some of your out-of-pocket costs such as deductibles or coinsurance.
Do I have to enroll in Medicare and Medicaid separately?
Individuals must enroll on Medicare and Medicaid separately. All seniors who are eligible for retirement Social Security benefits are entitled to Medicare. In addition, many people who are living with a disability will be able to claim Medicaid. Eligibility for Medicare is set at a federal level, which means the standards are the same nationwide.
How do I qualify for the full dual eligible program?
Qualifying as full dual eligible is based on your assets, which include checking and savings accounts, stocks, real estate (other than your primary residence) and vehicles (if you own more than one).
What percentage of dual-eligible enrollment is dually eligible?
ESRD 0.6% Sources: Dual-Eligible Enrollment Data come from Monthly Enrollment Snapshots: Quarterly Update from September 2020. The Percentage of Medicaid Population that is Dually Eligible by State was calculated by dividing dual-eligible enrollment by total Medicaid enrollment.
When can a patient have both Medicare and Medicaid?
Some people qualify for both Medicare and Medicaid and are called “dual eligibles.” If you have Medicare and full Medicaid coverage, most of your health care costs are likely covered.
What does it mean if a Medicare patient is dual eligible?
Dually eligible beneficiaries are people enrolled in both Medicare and Medicaid who are eligible by virtue of their age or disability and low incomes.
Can you qualify for both Medicare and Medical?
If you qualify for full Medi-Cal (Medi-Cal without a share of cost (SOC)), Medi-Cal will also cover your Medicare Part A and B deductibles and copayments, and pay your monthly Medicare Part B premium. Learn more. If you have both Medicare and Medi-Cal, how you receive your benefits depends on the county you live in.
What do you call an individual who receives both Medicare and Medicaid?
Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (about 12.3 million people). Dual eligibles are categorized based on whether they receive partial or full Medicaid benefits.
What plan provides both Medicare and Medicaid coverage?
UnitedHealthcare Connected® for One Care (Medicare-Medicaid Plan) is a health plan that contracts with both Medicare and MassHealth (Medicaid) to provide benefits of both programs to enrollees.
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
Can you have Medicare and Medicaid?
Medicaid is a state and federal program that provides health coverage if you have a very low income. If you are eligible for both Medicare and Medicaid (dually eligible), you can have both. They will work together to provide you with health coverage and lower your costs.
Who qualifies for Medi Medi?
Medi-Cal covers a wide variety of people, including people who are under 65, living with a disability, as well as children under 19, parents, or other adults caring for a child, and even adults without dependent children in some locations as long as they demonstrate financial need.
What is the income to qualify for Medi-Cal?
This means that a single adult, in order to qualify for Covered California and the health insurance subsidies, will need to have an income of more than $1,564 per month. The annual amount for a single adult for Covered California will need to be over $18,755 per year.
What is a partial dual eligible?
“Partial dual eligible” is a term used to describe Medicare beneficiaries who receive financial assistance for certain Medicare costs from their state Medicaid program. These individuals don't qualify for full Medicaid benefits from their state, like long-term services and supports or behavioral health services.
When a patient has Medicaid coverage in addition to other third party payer coverage Medicaid is always considered the?
For individuals who have Medicaid in addition to one or more commercial policy, Medicaid is, again, always the secondary payer.
What does a dual eligible patient mean quizlet?
An individual who is covered by both Medicare and Medicaid is called an. Dual Eligible.
What is dual eligible?
Full dual eligible refers to those who receive full Medicaid benefits and are also enrolled in Medicare. People who are full dual eligible typically receive Supplemental Security Income (SSI) benefits, which provide cash assistance for basic food ...
What is partial dual eligibility?
Partial dual eligibility includes those who receive assistance from Medicaid in order to help pay for Medicare costs such as premiums, coinsurance or deductibles. Partial dual eligibles fall into one of four categories of eligibility for Medicare Savings Programs.
What is the Medicare and Medicaid program?
Another Medicare and Medicaid program is PACE, or Programs of All-Inclusive Care for the Elderly. PACE helps older Medicare beneficiaries to seek health care within their community, in their home and at PACE facilities. Some of the things that can be covered by PACE include: Adult day primary care. Dental care.
What is QMB in Medicare?
Qualified Medicare Beneficiary (QMB) Program. This program helps pay for Medicare Part A and Part B premiums, deductibles, coinsurance and copayments. Eligibility requires: Income of no more than $1,061 per month for an individual in 2019, or $1,430 per month for a married couple.
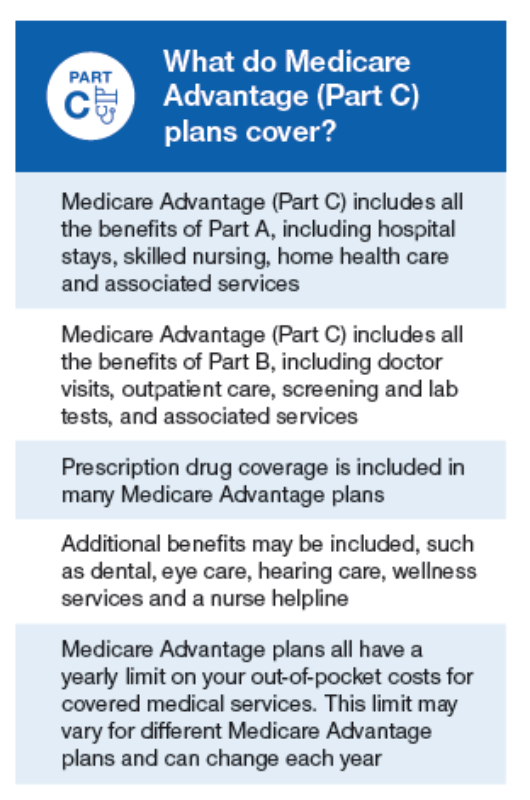
What is a special needs plan?
A Medicare special needs plan is a certain type of Medicare Advantage plan that is designed for people with specific health conditions or circumstances. A D-SNP is built for the specific needs of dual eligibles. All Medicare SNPs (including Medicare D-SNPs) provide prescription drug coverage.
What is a dual SNP?
If you are Medicare dual eligible, you may qualify for a Medicare D-SNP (Dual Special Needs Plan), which is a type of Medicare Advantage plan. 61.9 million Americans are Medicare beneficiaries. 1 In 2019, more than 12 million Americans were dually eligible for Medicare and Medicaid and are enrolled in both programs. 2.
What is an annual special enrollment period?
An annual Special Enrollment Period to enroll in a Part D plan or switch to a new one. Elimination of Part D late enrollment penalties. You automatically qualify for Extra Help if you are enrolled in Medicaid, Supplemental Security Income or a Medicare Savings Program.
Who Is Dual Eligible for Medicare and Medicaid in 2022?
If you meet the required qualifications for Medicare and Medicaid in 2020, you may be dual eligible.
How Do Medicare and Medicaid Work Together?
When a person is eligible for both Medicare and Medicaid benefits, Medicare serves as the primary payer and Medicaid is the secondary payer.
What Are the Benefits of Being Dual Eligible in 2022?
If you are dual eligible, you can benefit from both Medicare and Medicaid. You may also qualify for a Medicare Savings Program (MSP) .
What Is a Medicare Dual Eligible Special Needs Plans (D-SNP)?
Beneficiaries who qualify for both Medicare and Medicaid may also qualify for a Medicare Dual Eligible Special Needs Plan (D-SNP), if one is available where you live.
Medicare Supplement Insurance (Medigap) Can Help Pay for Out-of-Pocket Medicare Costs
If you are dual eligible for Medicare and Medicaid, you may be able to apply for a Medicare Supplement (Medigap) plan that’s available where you live.
What is dual eligible Medicare?
Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (12.1 million people). Dual eligibles are categorized based on whether they receive partial or full Medicaid benefits. Full-benefit dual eligibles have comprehensive Medicaid coverage, ...
What is a dual eligible special needs plan?
If you are dual eligible, you are can enroll in a dual eligible special needs plan (D-SNP) that covers both Medicare and Medicaid benefits. These plans may also pay for expenses that Medicare and Medicaid don’t over individually, including over-the-counter items, hearing aids, and vision or dental care. Beneficiaries who are dual eligible can ...
Do seniors qualify for medicaid?
Many seniors who live in nursing homes are dual eligible: they qualify for Medicare based on their age, and Medicaid because of their financial circumstances.
Does Medicare cover long term care?
But this is not the case for things Medicare doesn’t cover, like long-term care . If Medicaid is covering a beneficiary’s long-term care, Medicare will still be the primary payer for any Medicare-covered services – like skilled nursing care or physical therapy.
Is Medicare the same as Medicaid?
The federal government oversees Medicare eligi bility – meaning it is the same in each state. But states set their own eligibility rules for Medicaid and the MSPs (within federal guidelines) – and income limits for these programs vary widely.
Dual Enrollment Is Available for Low-Income Individuals
Medicare and Medicaid are two separate programs, each with different eligibility requirements. Individuals must enroll on Medicare and Medicaid separately. All seniors who are eligible for retirement Social Security benefits are entitled to Medicare. In addition, many people who are living with a disability will be able to claim Medicaid.
Some Seniors May Qualify for Other Medical-Related Assistance
In addition to Medicaid, many seniors may be eligible for other assistance, depending on the state they reside in. For example, many states offer a Home and Community Based Services waiver that provides support with all or part of the cost of assisted living or other long-term care.
How many people are covered by medicaid?
Medicaid also provides coverage to 4.8 million people with disabilities who are enrolled in Medicare.
Can you be covered by Medicare and Medicaid?
Individuals who are enrolled in both Medicaid and Medicare, by federal statute, can be covered for both optional and mandatory categories.
Can Medicare help with out of pocket medical expenses?
Medicare enrollees who have limited income and resources may get help paying for their premiums and out-of-pocket medical expenses from Medicaid (e.g. MSPs, QMBs, SLBs, and QIs).