When you buy a Medicare supplement insurance policy, you keep your original Medicare and can go to any doctor who accepts Medicare. Your Medicare supplement insurance works in tandem with your Medicare, so if your doctor accepts Medicare, your supplement insurance is accepted as well.
Full Answer
How does Medicare supplement insurance work with Medicare?
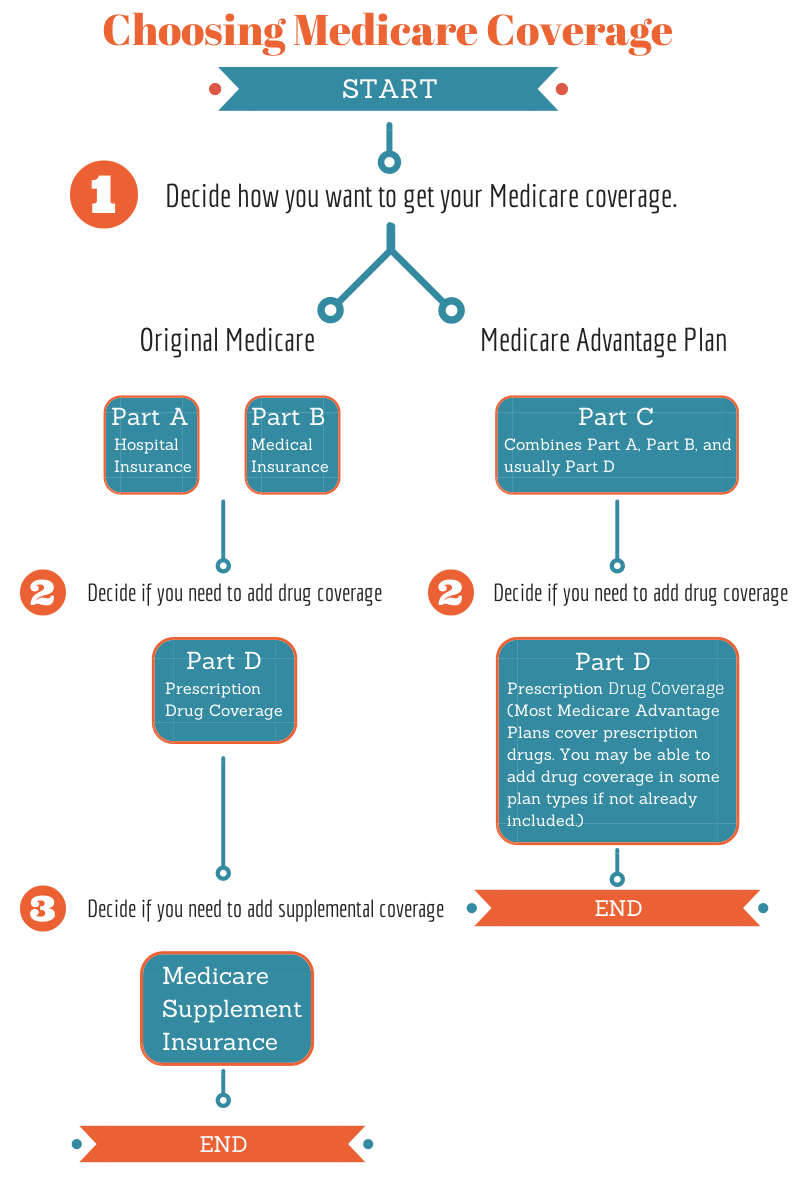
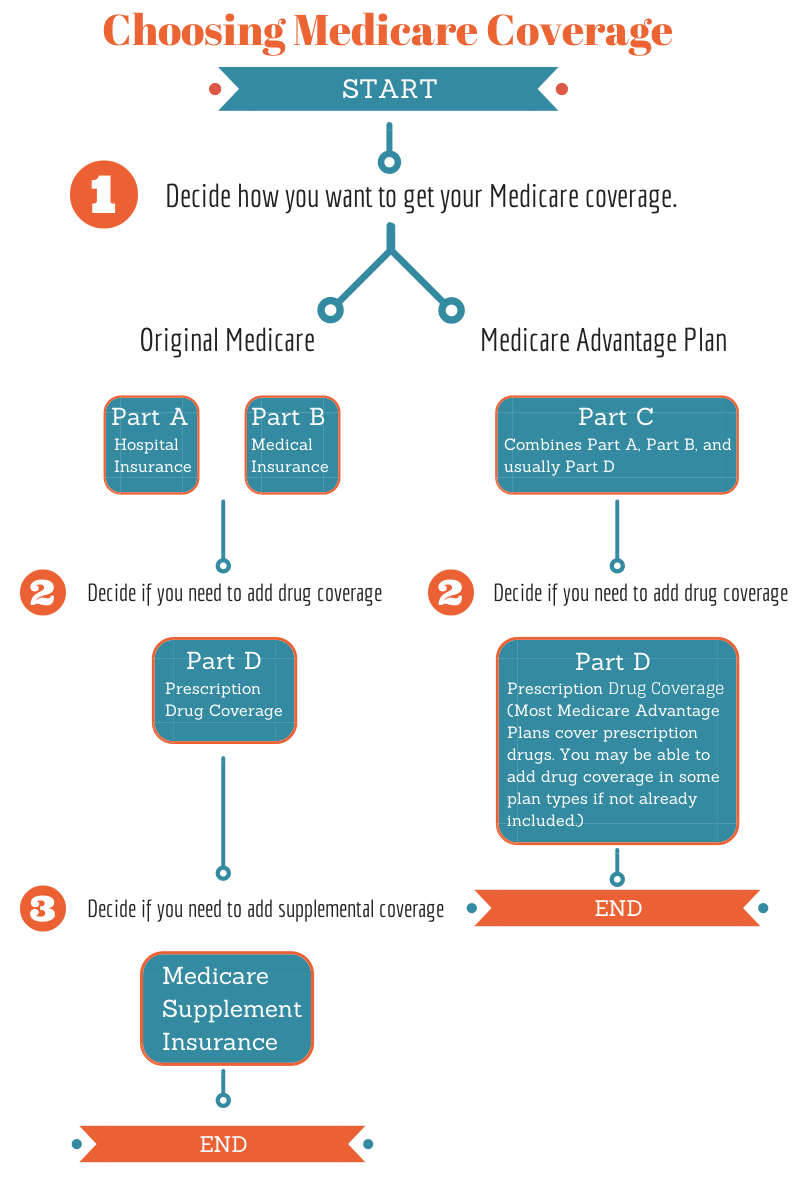
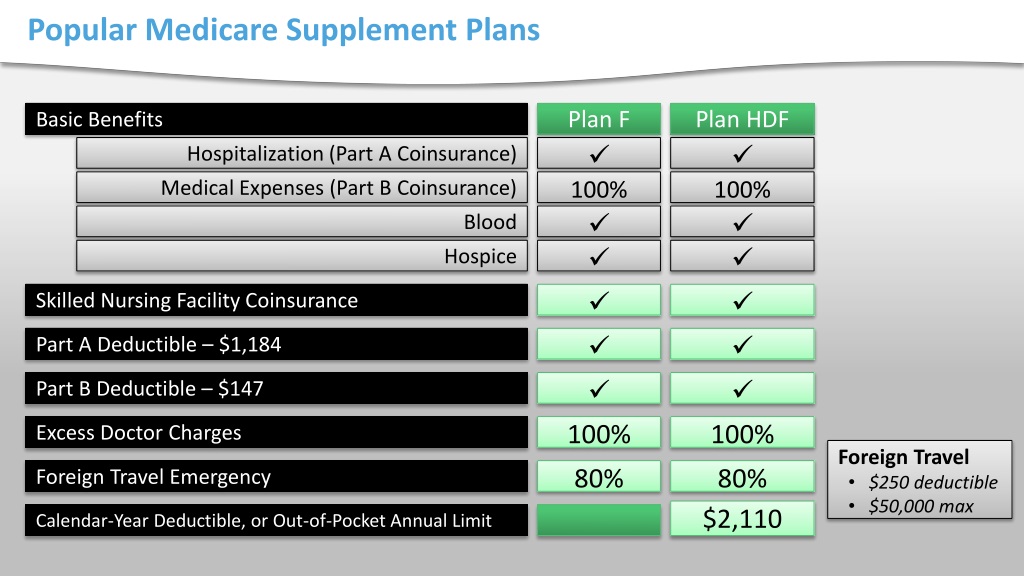
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people new to Medicare can no longer cover the Part B deductible.
What is Medicare supplement insurance (Medigap) under 65?
If you’re enrolled in Medicare under 65 because of a disability, you may be eligible to purchase a Medicare Supplement Insurance (or Medigap) plan. Medicare Supplement Insurance can help cover some of the health care costs that come with Original Medicare.
Who pays first – Medicare or Medicare supplement insurance?
If you're retired, have Medicare and have group health plan coverage from a former employer, generally Medicare pays first. Your retiree coverage pays second. What's Medicare Supplement Insurance (Medigap)? Read about Medigap (Medicare Supplement Insurance), which helps pay some of the health care costs that Original Medicare doesn't cover.
What do you need to know about Medicare Medigap insurance?
You must have Medicare Part A and Part B. A Medigap policy is different from a Medicare Advantage Plan. Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. You pay the private insurance company a monthly
What does Medicare supplement insurance primarily cover?
When you buy a Medicare Supplement insurance plan, you are still enrolled in Original Medicare, Part A and Part B. Medicare pays for your health-care bills primarily, while the Medigap plan simply covers certain cost-sharing expenses required by Medicare, such as copayments or deductibles.
Do Medicare supplements require referrals?
Which Medicare plans require referrals? Original Medicare (parts A and B) doesn't require referrals for specialist care. However, if you have Part A or Part B coverage through a Medicare Advantage (Part C) plan, you may need a referral before seeing a specialist.
What are the advantages and disadvantages of Medicare Supplement plans?
Medicare Advantage offers many benefits to original Medicare, including convenient coverage, multiple plan options, and long-term savings. There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling.
Does Medicare Supplement requires you to use a defined network of doctors?
The short answer is, YES! Because Medicare is primary and your supplement is secondary, networks will not differ in any way between insurance companies. You have the same access to providers with almost all plans.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
How much does AARP Medicare Supplement Plan G cost?
1. AARP Medigap costs in states where age doesn't affect the pricePlan nameAverage monthly cost for AARP MedigapPlan G (1)$173Plan K$70Plan L$136Plan N$1676 more rows•Jan 24, 2022
What are the disadvantages of a Medicare supplement plans?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
What is the downside to Medigap?
Some disadvantages of Medigap plans include: Higher monthly premiums. Having to navigate the different types of plans. No prescription coverage (which you can purchase through Plan D)
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
Which Medicare deductible is no longer covered under Supplement plans?
But as a result of legislation just passed by Congress, starting in 2020 Medigap plans will no longer be allowed to offer coverage of the Medicare Part B deductible, which is currently $203 (in 2021).
What is the difference between a Medicare Supplement plan and a Medicare Advantage plan?
Medicare Supplement plans. A Medicare Advantage plan (Medicare Part C) is structured to be an all-in-one option with low monthly premiums. Medicare Supplement plans offer additional coverage to Original Medicare with low to no out-of-pocket costs.
Which of the following is not covered under Part A in Medigap insurance?
Part A does not cover the following: A private room in the hospital or a skilled nursing facility, unless medically necessary. Private nursing care.
What is Medicare Supplement Plan?
A Medicare Supplement Plan (also called a Medigap plan) can help pay Medicare Part A and Part B costs, such as deductibles, copayments, and coinsurance. If you’re eligible for a Medicare Supplement Plan, enrollment is a good idea, as these plans take much of the worry out of escalating medical costs by having no cap on the coverage they offer.
How old do you have to be to get Medicare Supplement?
You must be age 65 or older (in several states, some Plans are offered to those under 65 who are on disability). You must reside in the state in which ...
How long do you have to wait to buy a Medigap policy?
Under certain circumstances, there is a waiting period of up to six-months for pre-existing conditions for Medigap policies purchased during the OEP.
When does Medigap OEP start?
If you delay Part B coverage, your Medigap OEP will be the six-month period beginning on the first day of the month you enroll in Part B. Example 1: If you turn 65 on May 1 and your Part B begins May 1, your Medigap OEP begins May 1 and runs through October 31. Example 2: If you turn 65 on May 1, 2020 but wait until your Employer Group Coverage ...
When do you join a Medicare Advantage Plan?
You joined a Medicare Advantage Plan when you first became eligible for Medicare and disenrolled within 12 months, or your previous Medigap policy, Medicare Advantage Plan, or PACE program ends its coverage or committed fraud. If you have a Medicare Advantage Plan, Medicare SELECT policy, or PACE program and you move out of the plan’s service area, ...
When is the best time to buy a Medigap policy?
The best time to buy a Medigap policy is during your Medigap Open Enrollment Period. OEP is the six-month period that begins on the first day of the month in which you’re 65, or older, and enrolled in Medicare Part B. If you delay Part B coverage, your Medigap OEP will be the six-month period beginning on the first day of ...
What is SEP medical underwriting?
Included in the SEP category is the SEP for relocation to the U.S. from a foreign country.
How Medicare works with other insurance
Learn how benefits are coordinated when you have Medicare and other health insurance.
Retiree insurance
Read 5 things you need to know about how retiree insurance works with Medicare. If you're retired, have Medicare and have group health plan coverage from a former employer, generally Medicare pays first. Your retiree coverage pays second.
What's Medicare Supplement Insurance (Medigap)?
Read about Medigap (Medicare Supplement Insurance), which helps pay some of the health care costs that Original Medicare doesn't cover.
When can I buy Medigap?
Get the facts about the specific times when you can sign up for a Medigap policy.
How to compare Medigap policies
Read about different types of Medigap policies, what they cover, and which insurance companies sell Medigap policies in your area.
Medigap & travel
Read about which Medigap policies offer coverage when you travel outside the United States (U.S.).
What is Medicare Supplement Plan?
A Medicare Supplement plan (also known as Medigap) is used for exactly what the name suggests — it supplements the gaps in your original Medicare coverage. This means you must have Medicare Parts A and B in order to get a Medigap plan.
How long is the Medigap enrollment period?
Medicare Supplements are no different. There is a 6-month Medigap enrollment period, during which you can enroll at any time.
When do you get Medicare Part B?
If you get Medicare Part B before you turn 65, your OEP automatically begins the month you turn 65. Some states have Medigap open enrollment periods for people under 65. If that’s the case, you’ll still get a Medigap OEP when you turn 65, and you'll be able to buy any policy sold in your state. Before making a purchase, find out what rights you ...
Does Delaware require Medigap coverage for disabled people?
This requirement does not include those under 65 with ESRD. **Delaware requires that insurance carriers offer at least one Medigap policy to those under 65 who have ESRD. This requirement does not include those under 65 who are disabled. Even if your state isn't listed above, you may be able to get coverage. Some insurance companies voluntarily ...
You may not be guaranteed Medigap coverage
Lora Shinn has been writing about personal finance for more than 12 years. Her articles have also been published by CNN Money, U.S. News & World Report, and Bankrate, among others.
What Is Medicare Supplement Insurance?
Medicare Supplement Insurance or Medigap is sold by private insurance companies. You must be enrolled in both Parts A and B to be eligible for a policy. It’s not an option if you have a Medicare Advantage plan, and coverage is for one person only (spouses need to purchase Medigap separately).
Can You Be Denied Medigap Coverage?
The answer is yes, you can be denied Medigap coverage. But you can also be guaranteed Medigap coverage if you apply during your Medigap open enrollment period.
Denial of Medigap Policy Renewal
In most cases your renewal is considered guaranteed and cannot be dropped, however there are certain circumstances when the insurance company can decide not to renew your Medigap policy:
How Do You Get Medigap Coverage?
The best time to get Medigap coverage is during your once-per-lifetime Medigap open enrollment period. This period lasts for six months, beginning the first month you are enrolled in Medicare Part B and are at least 65. 10
Medigap Guaranteed Issue Rights
You may qualify for guaranteed issue in specific situations outside the Medigap open enrollment period by federal law. For example, if:
Medigap and Medicare Advantage
If you have a Medicare Advantage (MA) plan, it’s illegal for an insurance company to sell you a Medigap policy. But if you switch to MA after you’ve purchased a Medigap policy, you’ll probably want to drop your policy since you can’t use it to supplement your MA plan.
Is United American Insurance endorsed by the government?
The purpose of this communication is the solicitation of insurance. United American Insurance Company is not connected with, endorsed by, or sponsored by the U.S. government, federal Medicare program, Social Security Administration, or the Department of Health and Human Services. Policies and benefits may vary by state and have some limitations and exclusions. Individual Medicare Supplement insurance policy forms MSA10, MSB10, MSC10, MSD10, MSF10, MSHDF10, MSG10, MSHDG, MSK06R, MSL06R, MSN10 and in WI, MC4810 and MC4810HD, MC4810HDG are available from our Company where state-approved. Some states require these plans be available to persons under age 65 eligible for Medicare due to disability or End Stage Renal disease (ESRD). You may be contacted by an agent or producer representing United American Insurance Company, PO Box 8080, McKinney, TX 75070-8080. OUTLINE OF COVERAGE PROVIDED UPON REQUEST.
Is United American a Medicare Supplement?
United American has been a prominent Medicare Supplement insurance provider since Medicare began in 1966. Additionally, we’ve been a long-standing participant in the task forces working on Medicare Supplement insurance policy recommendations for the National Association of Insurance Commissioners.
Does Medicare Supplement Insurance cover deductibles?
The purpose of Medicare Supplement Insurance is to cover the cost left by deductibles and coinsurance in Original Medicare, but as full Medicaid coverage should cover the majority of those costs, a Medicare Supplement Insurance policy isn’t necessary. 3.