The Medicare Part D formulary is a list of drugs that have coverage under your policy. The formulary must include at least two drugs per category, and the insurance company can choose the options. But what exactly is a drug formulary? What happens if your medication isn’t part of this formulary?
What is a Medicare Part D formulary?
The Medicare Part D formulary is a list of drugs that have coverage under your policy. The formulary must include at least two drugs per category, and the insurance company can choose the options.
What does Medicare Part D’s five-tier system look like?
Below is an example of how the most common five-tier system might look: Tier 1 is the least expensive of the Medicare Part D tiers, and includes the lower-cost preferred generic drugs.
What is part D Medicare Part A and B?
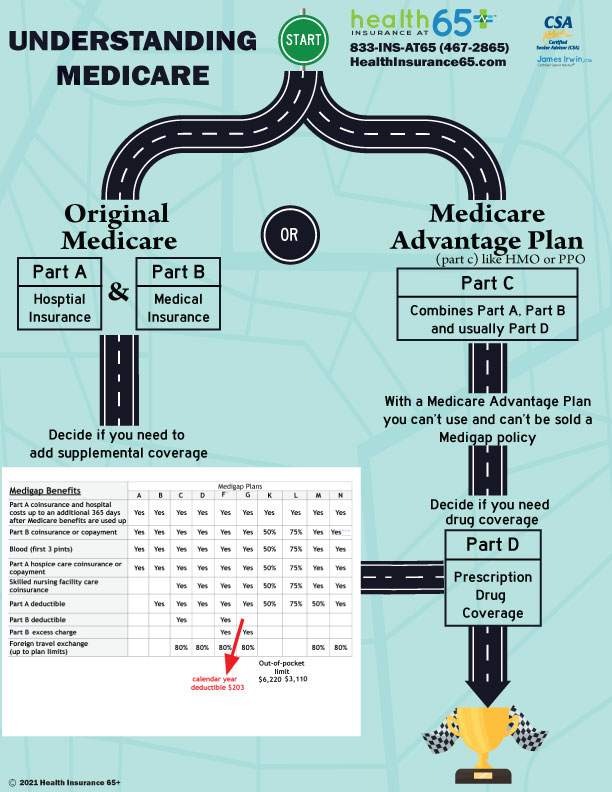
Part D plans are designed to defray the cost of your medications, but they do not kick in automatically when you enroll in Medicare Parts A and B. Once eligible, you would apply for the coverage through a private insurance company.
What is the Medicare Part D formulary tier 6 Select Care?
Each Medicare Part D formulary is different, so some might include more tiers like a Tier 6 Select Care. Tier 6 tends to refer to a few generic drugs for diabetes and high cholesterol available with some specific insurance plans.
Who determines drug formulary?
A drug formulary is a list of generic and brand-name prescription drugs covered by a health plan. The health plan generally creates this list by forming a pharmacy and therapeutics committee consisting of pharmacists and physicians from various medical specialties.
Is formulary developed by CMS?
A: The Formulary Reference NDC File is a file created and maintained by CMS that contains a list of drugs that may be included on Part D formularies.
How is a formulary determined?
Formulary Development. The medications and related products listed on a formulary are determined by a pharmacy and therapeutics (P&T) committee or an equivalent entity. P&T committees are comprised of primary care and specialty physicians, pharmacists and other professionals in the health care field.
What best defines Medicare Part D?
Medicare Part D is a prescription drug benefit program that is offered as part of the broader Medicare federal health insurance program for persons 65 years and older, certain younger people with disabilities, and people with end-stage renal disease.
Is formulary based on CMS guidelines?
CMS will evaluate formulary classification systems as well as the actual list of drugs included in the formulary, using existing widely used classification systems and drug plans as checks.
What is the CMS formulary Reference File?
Guidance for frequently asked questions pertain to CMS' Formulary Reference File (FRF). The FRF serves as a listing of drug products that can be included on Part D sponsors' Health Plan Management System (HPMS) formulary files that are submitted to CMS for review and approval.
Which develops a formulary for an institution?
The P&T committee is responsible for developing, managing, updating and administering the formulary. The P&T committee also designs and implements formulary system policies on utilization and access to medications.
What does a formulary pharmacist do?
Formulary management. The formulary pharmacist's other significant role is the maintenance and update of the trust formulary. The formulary pharmacist is usually involved at every stage of formulary development, from conception to publication and distribution.
What is a formulary in a health insurance plan?
A list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list.
What is Medicare Part D and how does it work?
It is an optional prescription drug program for people on Medicare. Medicare Part D is simply insurance for your medication needs. You pay a monthly premium to an insurance carrier for your Part D plan. In return, you use the insurance carrier's network of pharmacies to purchase your prescription medications.
Why is there a donut hole in Medicare Part D?
Why is there a donut hole in Medicare Part D? The donut hole was created to incentivize people to use generic drugs. Thus, keeping beneficiary costs low and reducing Medicare expenses on the program level.
What is Medicare Part D?
The Medicare Part D formulary is a list of drugs that have coverage under your policy. The formulary must include at least two drugs per category, and the insurance company can choose the options.
How to know what medications are in Medicare Part D?
How to Know What Medications are in a Medicare Part D Formulary. If you have a health insurance agent, they can assist in finding your plan’s formulary list. You can check insurance carrier websites to view the drug formularies they offer. Those with Medicare are eligible for a drug plan and should enroll as soon as possible.
What does a doctor's report state?
If you’re seeking a tiering exception, your doctor’s report must state that the preferred medications would adversely affect you. If you’re trying to obtain a formulary exception, your doctor’s statement must indicate that the non-formulary drug is necessary.
What is formulary exception?
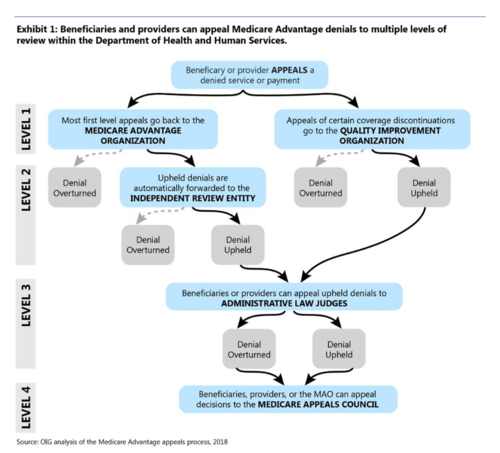
A Formulary Exception is a form of a request to determine coverage. By obtaining an exception, you may be able to get a drug that’s not on your plan’s formulary or ask your plan to bypass step therapy or prior authorizations.
How many protected classes does an insurance plan cover?
Plans must cover the six protected classes. But, every formulary may not contain your medication. Every insurance plan has its drug formularies. Each medication must adhere to the Food and Drug Administration’s (FDA) regulations.
Is Medicare Part D 5 star?
Medicare Part D plans have a star-rating system similar to Medicare Advantage. Many locations don’t have 5-star plans, but some areas will have those options. The best Part D plan in 2021 varies by county; in some areas, Cigna may have higher ratings, whereas Humana could have higher ratings in other areas.
Can a pharmacy plan change the formulary?
The plan can change the formulary anytime, but they must notify you. Each plan has a different list of drugs. You’ll want to find the formulary that fits with the medications you take. But, it can be hard to predict next year’s prescriptions.
What does Medicare Part D cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary.
What are the tiers of Medicare?
Here's an example of a Medicare drug plan's tiers (your plan’s tiers may be different): Tier 1—lowest. copayment. An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug.
What is formulary exception?
A formulary exception is a drug plan's decision to cover a drug that's not on its drug list or to waive a coverage rule. A tiering exception is a drug plan's decision to charge a lower amount for a drug that's on its non-preferred drug tier.
What happens if you don't use a drug on Medicare?
If you use a drug that isn’t on your plan’s drug list, you’ll have to pay full price instead of a copayment or coinsurance, unless you qualify for a formulary exception. All Medicare drug plans have negotiated to get lower prices for the drugs on their drug lists, so using those drugs will generally save you money.
How many prescription drugs are covered by Medicare?
Plans include both brand-name prescription drugs and generic drug coverage. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes. This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per ...
How many drugs does Medicare cover?
All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug. However, in most cases, a similar drug should be available.
What is a tier in prescription drug coverage?
Tiers. To lower costs, many plans offering prescription drug coverage place drugs into different “. tiers. Groups of drugs that have a different cost for each group. Generally, a drug in a lower tier will cost you less than a drug in a higher tier. ” on their formularies. Each plan can divide its tiers in different ways.
How to get prescription drug coverage
Find out how to get Medicare drug coverage. Learn about Medicare drug plans (Part D), Medicare Advantage Plans, more. Get the right Medicare drug plan for you.
What Medicare Part D drug plans cover
Overview of what Medicare drug plans cover. Learn about formularies, tiers of coverage, name brand and generic drug coverage. Official Medicare site.
How Part D works with other insurance
Learn about how Medicare Part D (drug coverage) works with other coverage, like employer or union health coverage.
What is a Part D drug?
Part D covered drug is available only by prescription, approved by the FDA (or is a drug described under section 1927(k)(2)(A)(ii) or (iii) of the Act), used and sold in the United States, and used for a medically accepted indication (as defined in section 1927(k)(6) of the Act). A covered Part D drug includes prescription drugs, biological products, insulin as described in specified paragraphs of section 1927(k) of the Act, vaccines licensed under section 351 of the Public Health Service Act and for vaccine administration on or after January 1, 2008, its administration. The definition also includes medical supplies directly associated with delivering insulin to the body, including syringes, needles, alcohol swabs, gauze, and insulin injection delivery devices not otherwise covered under Medicare Part B, such as insulin pens, pen supplies, and needle-free syringes, can satisfy the definition of a Part D drug. CMS defines those medical supplies to include syringes, needles, alcohol swabs, gauze, and those supplies directly associated with delivering insulin into the body.
Does Medicare cover outpatient prescriptions?
Traditional Medicare (Part A/B) does not cover most outpatient prescription drugs. Medicare bundled payments made to hospitals and skilled nursing facilities generally cover all drugs provided during a stay. Medicare also makes payments to physicians for drug or biological products that are not usually self-administered. This means that coverage is usually limited to
Is inhalation drug covered by Part B?
Answer 1 – No. Since there currently is no coverage under Part B for inhalation drugs delivered through metered-dose inhalers and dispensed by a pharmacy, these drugs would be covered under Part D.
Is IVIG covered by Part B?
Answer 5 – It depends. Part B coverage for IVIG in the home is for individuals whose diagnosis is primary immune deficiency disease. Part D would provide coverage for IVIG in the home for all other medically accepted indications. Prior authorization requirements could be used to ensure appropriate payment in accordance with the Part D sponsor’s medical necessity criteria. It would not be appropriate to routinely require a rejection of a claim under Part B before processing a Part D claim. Such a policy would be disruptive to beneficiaries and pharmacies and would unnecessarily increase Part B contractor costs.
Is an external infusion pump covered by Part B?
Answer 2 – No, drugs that require an external infusion pump are not covered under Part B under those circumstances because the law limits coverage under Part B’s DME benefit to those items that are furnished for use in a patient’s home, and specifies that a hospital or SNF cannot be considered the beneficiary’s “home” for this purpose.
Does Part B coverage affect Part D?
Answer 5 - First, it is important to keep in mind that in most cases Part B drug coverage should not impact payment decisions by Part D sponsors since Part B coverage is generally in a provider setting or physician's office rather than for drugs dispensed at a pharmacy.
Is a drug approved by the FDA a Part D drug?
Answer 4 - No. Once a drug is approved by the FDA it is a Part D drug. While it is not automatically a covered Part D drug, that is, it may not be included on a Part D sponsor’s formulary, a member could request coverage on an exception basis.
What are the tiers of Medicare Part D?
The Medicare Part D tiers refer to how drugs are organized in a formulary. They include both generic and brand name drugs, covered for different prices. Most commonly there are tiers 1-5, with 1 covering the lowest-cost drugs and 5 covering the most expensive specialty medications.
What is Tier 1 Medicare?
Tier 1 is the least expensive of the Medicare Part D tiers, and includes the lower-cost preferred generic drugs. Preferred drugs means a certain set of types of medications that have been approved by the insurance company to be in this low-cost grouping. Generic refers to non-name brand versions of each type of drug.
What is Medicare Advantage Plan?
Some Medicare Advantage plans, known as Medicare Advantage Prescription Drug Plans (MAPD), include Part D coverage. In MAPD plans, the portion of the plan that covers drugs will follow the same standards as stand-alone prescription drug plans. So, you will want to check the plan’s formulary to see how your medications are covered.
Does Medicare Part D cost more than tier 1?
Medicare Part D tiers 1 and 2 are often set up to exempt you from paying a deductible, whereas with drugs in the higher tiers you may have to pay the full drug cost until you meet the deductible, then pay a copay/coinsurance.