Who determines medical necessity?
Jul 02, 2021 · Medicare’s Criteria for Medical Necessity. CMS allows its Medicare Administrative Contractors (MACs) to determine whether services provided to their beneficiaries are reasonable and necessary, and therefore medically necessary. MACs use the following criteria to determine if an item or service is medically necessary: It is safe and effective.
What are medically necessary services under Medicare?
Sep 10, 2021 · Some cases say the doctor is the sole responsibility for determining medical necessity. Others say “necessity” is a contract term that a doctor must prove a service is appropriate. If the doctor submits documentation to show necessity, in some cases, Medicare covers, but, sometimes, services don’t have coverage no matter how necessary.
How does Medicare define “medical necessity?
Medically necessary services under Original Medicare. Original Medicare is the government-run health-care program, made up of Medicare Part A (hospital insurance) and Part B (medical insurance). Medicare Part A covers medically necessary services and treatment you get in an inpatient setting, including: Hospital care.
How does Medicare determine if a service is necessary?
Apr 05, 2019 · Medicare defines “medical necessity” as services or items reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member. CMS has the power under the Social Security Act to determine, on a case-by-case basis, if the method of treating a patient is reasonable and necessary.

What department is responsible for determining medical necessity?
The Office of Inspector General at the Department of Health and Human Services (DHHS) in its draft compliance program for Individual and Small Group Physician Practices states that "Medicare (and many insurance plans) may deny payment for a service that the physician believes is clinically appropriate, but which is not ...
Who determines medical necessity for reimbursement?
A service has to be deemed medically necessary in order to be covered by health insurance. Health plans use various guidelines, including state and federal benefit mandates, and case management procedures, to determine what services are considered medically necessary.Mar 11, 2022
How do you establish medical necessity?
Well, as we explain in this post, to be considered medically necessary, a service must:“Be safe and effective;Have a duration and frequency that are appropriate based on standard practices for the diagnosis or treatment;Meet the medical needs of the patient; and.Require a therapist's skill.”Dec 27, 2018
Who decides what is medically necessary in US healthcare?
Without a federal definition of medical necessity or regulations listing covered services, health insurance plans will retain the primary authority to decide what is medically necessary for their patient subscribers.
Which procedure does not meet the criteria for medical necessity?
What is the main purpose of capitation payments? To control health care costs by limiting physician payments. Which procedure does NOT meet the criteria for medical necessity? The procedure is elective.
What is not a common reason Medicare may deny a procedure?
What are some common reasons Medicare may deny a procedure or service? 1) Medicare does not pay for the procedure / service for the patient's condition. 2) Medicare does not pay for the procedure / service as frequently as proposed. 3) Medicare does not pay for experimental procedures / services.
Is medical necessity only for Medicare?
Who Determines Necessity? There is no difference in the definition of "medical necessity" based on whether you are on Medicare or Medicaid. However, the list of included services in any other health plan may vary.
What is failed medical necessity?
Medical necessity documentation, or lack of it, is one of the most common reasons for claim denials. For a service to be considered medically necessary, it must be reasonable and necessary to diagnosis or treat a patient's medical condition.
Why is medical necessity determination important in the healthcare setting?
If the physician determines the procedure is medically necessary even though the coverage policy does not approve it, this gives you the opportunity to educate your patients that the service may be denied by their insurance carrier. The patient then has the choice whether to have the procedure.Nov 21, 2012
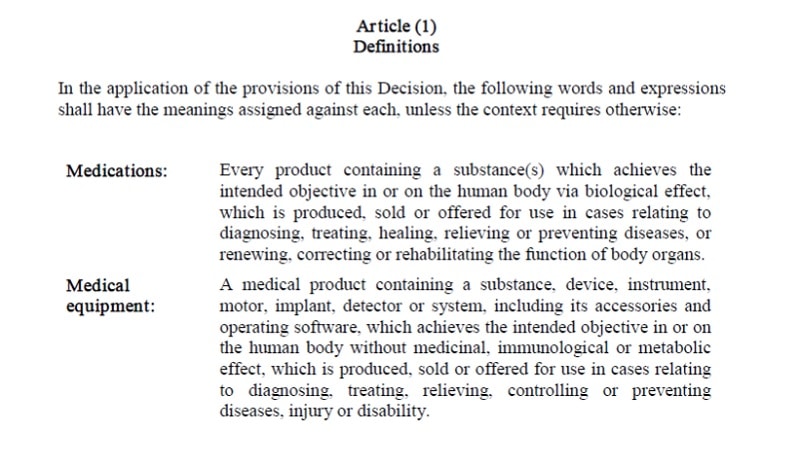
What defines medically necessary?
Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease or its symptoms and that meet accepted standards of medicine.
What does ABN mean in Medicare?
If a provider feels a service is medically necessary for a Medicare patient and, upon policy review, the payer denies medically necessity, an ABN will protect the provider from loss of revenue. The patient should be given the ABN form to complete in its entirety and sign prior to having the service rendered.
Why is medical necessity important?
“Medical necessity” is an important concept for medical coders and auditors to understand. Health insurance companies (payers) use criteria to determine whether items or services provided to their beneficiaries or members are medically necessary.
Why is it important for the physician, coder, biller, and insurance company to all be on the same answer
It is important for the physician, coder, biller, and insurance company to all be on the same page when it comes to medical necessity. A provider may feel specific procedures or tests are medically necessary for a patient, but the insurance company can also make that determination based on their clinical policies.
What is billing provider for Medicare?
For Medicare patients, billing providers should refer to local and national coverage determinations for medical necessity criteria. Commercial insurances may also have their own policies. Providers should document the patient’s progress, response to treatment, and any necessary change (s) in diagnosis or treatment.
When discussing medical necessity denials or potential denials with a clinician, what is the medical necessity criteria?
When discussing medical necessity denials or potential denials with a clinician, present the medical necessity criteria the payer used to make the determination. This will prevent the debate of why non-clinical personnel can tell a provider a service is not medically necessary.
How often are preventive services limited?
Payers often set frequency limitations on certain services. For instance, preventive services are generally limited to one per year. To protect the provider’s or facility’s revenue stream, due diligence must be taken to properly identify any coverage limitations ahead of the patient’s encounter.
What is Cigna's clinically appropriate?
Cigna goes on to state, “Clinically appropriate, in terms of type, frequency, extent, site, and duration and considered effective for the patient’s illness, injury, or disease.
What does Medicare cover?
What might this mean for you as a beneficiary? According to the above definition, Medicare covers services that it views as medically necessary to diagnose or treat your health condition. Services must also meet criteria supplied by national coverage determinations and local coverage determinations.
What is medically necessary?
According to Medicare.gov, “medically necessary” is defined as “health-care services or supplies needed to prevent, diagnose, or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.”. In any of those circumstances, if your condition produces debilitating symptoms or side effects, ...
What is hospital-administered treatment?
Hospital-administered treatment that could have been delivered in a lower-cost setting. Prescription of drugs to treat fertility, sexual or erectile dysfunction, weight loss or weight gain, and cosmetic purposes.
Is glaucoma covered by Medicare?
Glaucoma screenings are covered for all beneficiaries with Medicare Part B who have a high risk for glaucoma. Factors that put you at high risk for glaucoma include having diabetes; having a family history of glaucoma; being African American and age 50 or older; and being Hispanic American and age 65 or older.
Do I need Medicare for an abdominal aortic aneurysm?
You must have Medicare Part B and meet one of the criteria that put you at risk for an abdominal aortic aneurysm: You’re eligible for this screening if you have a family history for the condition or if you’re a male age 65 to 75 who has smoked at least 100 cigarettes over your lifetime.
Does Medicare cover mammograms?
Intensive behavioral therapy for obesity is covered for all beneficiaries with Medicare Part B who have a body mass index (BMI) of 30 or higher. Mammograms are covered for women with Medicare Part B who are 40 or older; one baseline mammogram is covered for women with Part B between 35 to 39 years old.
Is Medicare Part B covered by Medicare?
Services that are not considered medically necessary. Services that aren’t deemed medically necessary are not covered by Original Medicare , Part A and Part B. It’s possible that some of these services may be covered by a Medicare Advantage plan, but that depends on your specific plan benefits. Non-medically necessary services according ...
What is medical necessity?
Defining “Medically Necessary”. Medical necessity is the procedure, test, or service that a doctor requires following a diagnosis. Anything “necessary” means Medicare will pay to treat an injury or illness. But, most procedures and medical equipment are necessary. You may run into a service or supply that needs approval from your doctor.
What is the term for a doctor to prove a service is necessary?
Others say “necessity” is a contract term that a doctor must prove a service is appropriate. If the doctor submits documentation to show necessity, in some cases, Medicare covers, but, sometimes, services don’t have coverage no matter how necessary.
What does "medically necessary" mean?
What Does Medically Necessary Mean. Medically necessary refers to health services or supplies that you need for treatment. You may feel that your condition warrants specific care, but your insurance may disagree. Below we’ll discuss what qualifies as necessary and what doesn’t meet the requirement.
Does Medicare consider a health service necessary?
Medicare considers a health service necessary if your condition meets all medical standards. The services need to diagnose and treat the health condition or injury. Medicare makes its determinations on state and federal laws. Local coverage makes determinations through individual state companies that process claims.
Does Advantage cover long term care?
Some Advantage plans will even cover long-term care and at-home services. The things that are “necessary” are dependant on the plan you select . You may want a document that advises you which services have coverage. But, if you’re wanting to find out your exact coverage, you can ask for an Advance Coverage decision.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare. You can also find her over on our Medicare Channel on YouTube as well as contributing to our Medicare Community on Facebook.
Does insurance cover xrays?
While insurance may cover the first set of x-rays, they may not pay for the second. So, the term “covered” is a loose term. Other cases may provide full coverage and full reimbursement. Alternative treatment options may be available. Also, your doctor can offer alternatives to see if you might get full coverage.
What is Medicare Part A?
Medicare Part A covers medically necessary services and treatment you get in an inpatient setting, including: *Medicare covers nursing care when non-skilled, custodial care (such as help with daily tasks like bathing or eating) isn’t the only care you need. This coverage is generally for a limited period of time.
What happens if Medicare doesn't cover medical expenses?
In most cases, if Medicare decides that your service or equipment doesn’t meet its definition of medically necessary, you won’t be covered , and you’ll have to pay for the full cost out of pocket. However, you have a few options if Medicare doesn’t cover a health-care service or item that you think you need.
What is advance coverage decision?
If you aren’t sure whether a service or item you may need is covered, you can ask Medicare for an advance coverage decision, which is a document from Medicare letting you know whether a particular service or equipment is covered and what your costs may be.
What is a county select?
County Select... “Medically necessary” is a standard that Medicare uses when deciding whether to cover a health-care service or item. This applies to everything from flu shots and preventive screenings, to kidney dialysis and wheelchairs.
What are medical supplies?
According to Medicare.gov, health-care services or supplies are “medically necessary” if they: 1 Are needed to diagnose or treat an illness or injury, condition, disease (or its symptoms). 2 Meet accepted medical standards.
Does Medicare cover cataract surgery?
However, if you get cataract surgery to implant an intraocular lens, Medicare helps cover the cost of corrective lenses (either one pair of eyeglasses or one set of contact lenses). You’ll pay 20% of the Medicare-approved amount, and the Medicare Part B deductible applies.
Does Medicare Advantage cover hospice?
By law, Medicare Advantage plans are required to cover at least the same level of health coverage as Original Medicare, including all medically necessary services under Medicare Part A and Part B (with the exception of hospice care). However, individual Medicare Advantage plans also have the flexibility to cover extra services ...
What is medical necessity?
Medicare defines “medical necessity” as services or items reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member.
What happens if a provider knows that a claim is not medically necessary?
If a pattern of such claims can be established, and the provider knows or should know that the services reported were not medically necessary, the provider may face monetary penalties, exclusion from Medicare program, and criminal prosecution.
How to support medical necessity for services reported?
To better support medical necessity for services reported, you should apply the following principles: 1. List the principal diagnosis, condition, problem, or other reason for the medical service or procedure. 2.
Can you be denied if you are not medically necessary?
Claims for services deemed to be not medically necessary will be denied. Further, if Medicare (or any other payer) pay for services that they later determine to be not medically necessary, they may demand that those payments be refunded (with interest).
Is coverage limited for medical services?
For all payors and insurance plans, even if a service is reasonable and necessary, coverage may be limited if the service is provided more frequently than allowed under a national coverage policy, a local medical policy, or a clinically accepted standard of practice.
Can a rule out statement be used for outpatient?
For office and/or outpatient services, never use a “rule-out” statement (a suspected but not confirmed diagnosis); a clerical error could permanently tag a patient with a condition that does not exist. Code symptoms, if no definitive diagnosis is yet determined, instead of using rule-out statements. 4.
Who is John Verhovshek?
John Verhovshek, MA, CPC, is a contributing editor at AAPC. He has been covering medical coding and billing, healthcare policy, and the business of medicine since 1999. He is an alumnus of York College of Pennsylvania and Clemson University.

Determining Medical Necessity
- No one wants to hear that a service is “not medically necessary.” To find out if Medicare covers what you need, talk to your doctor or other health care provider about why certain services or supplies are necessary, and ask if Medicare will cover them. If you have a private insurance plan…
Not Medically Necessary Services and Supplies
- The Medicare program covers many services and supplies that are needed to diagnose or treat medical conditions. Most beneficiaries do not have problems receiving covered services and treatments they need for their health. However, it is important to understand the types of services and supplies that are considered “not medically reasonable and necessary.” According to CMS, s…
Advance Beneficiary Notice of Noncoverage
- If you need something that is usually covered, but your doctor, health care provider, or supplier thinks that Medicare will not cover it, you will have to read and sign a notice called an “Advance Beneficiary Notice of Noncoverage” (ABN), and will serve as your acceptance that you may have to pay for the item, service, or supply.
Services Considered Medically Necessary
- What might this mean for you as a beneficiary? According to the above definition, Medicare covers services that it views as medically necessary to diagnose or treat your health condition. Services must also meet criteria supplied by national coverage determinations and local coverage determinations. These determinations are decided by the federal g...
Services That Are Not Considered Medically Necessary
- Services that aren’t deemed medically necessary are not covered by Original Medicare, Part A and Part B. It’s possible that some of these services may be covered by a Medicare Advantage plan, but that depends on your specific plan benefits. Non-medically necessary services according to CMS include, but may not be limited to, the following: 1. Times where your hospital service surp…
Exceptions to The Medically Necessary Requirement
- The following procedures are covered by Medicare if you meet the eligibility criteria for the health-care service. Most of these services are covered under Medicare Part B. If you have a Medicare Advantage plan, also called Medicare Part C, then these services are covered under that plan, as Medicare Advantage plans must cover everything under Part A and Part B. Covered preventive s…