Health plan formularies are typically created by a committee set up by the plan’s health insurance company. The formulary committee would likely include pharmacists and doctors from various medical areas. This committee would then choose which prescription drugs to include on the health plan formulary.
Full Answer
What is a Medicare formulary?
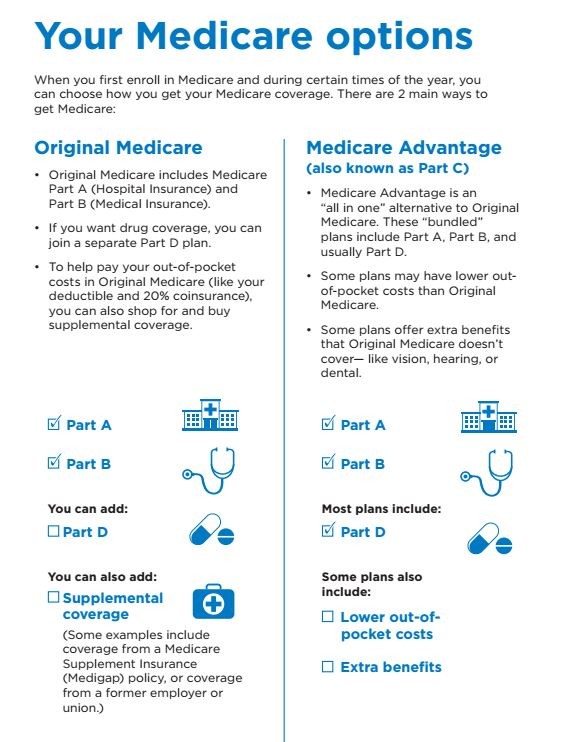
A Medicare formulary is the list of prescription drugs that are covered by a particular Medicare Part D or Medicare Advantage plan. Each plan includes its own formulary that determines which drugs are covered by the plan and how much the drugs cost based on which tier the drug is classified into.
What drugs are covered by Medicare drug plans?
Most Medicare drug plans (Medicare drug plans and Medicare Advantage Plans with prescription drug coverage) have their own list of what drugs are covered, called a formulary. Plans include both brand-name prescription drugs and generic drug coverage.
Why do I need a formulary for prescription drugs?
This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug.
Can drug plans remove brand name drugs from Medicare formularies?
For 2019 and beyond, drug plans offering Medicare prescription drug coverage (Part D) that meet certain requirements also can immediately remove brand name drugs from their formularies and replace them with new generic drugs, or they can change the cost or coverage rules for brand name drugs when adding new generic drugs.

Who develops formularies for Medicare?
The formulary is developed and updated regularly by the Blue Shield Pharmacy and Therapeutics (P&T) Committee and meets all Medicare requirements for included and excluded drugs.
What is a Medicare formulary?
Most Medicare drug plans have their own list of covered drugs, called a formulary. Plans cover both generic and brand-name prescription drugs. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes.
Why do insurance companies have formularies?
The purpose of a drug formulary is to help manage which drugs care providers can prescribe and that would be covered by a health plan in 2022. The goal of a medical formulary is to make sure that the drugs covered by a health plan are safe, effective and available at a reasonable cost.
What are payer formularies?
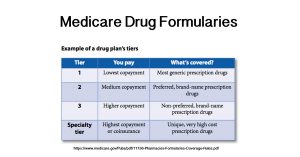
Formularies are lists of drug products covered by payers that distinguish between preferred or discouraged products by dividing outpatient therapies into three to five "tiers," each with a different level of patient cost sharing.
Who decides formulary?
Typically, a drug formulary is developed by experts using clinical evidence. A drug formulary usually consists of two to five groups of drugs – called tiers – with different levels of copayments or coinsurance by tier.
What does a formulary pharmacist do?
Formulary management. The formulary pharmacist's other significant role is the maintenance and update of the trust formulary. The formulary pharmacist is usually involved at every stage of formulary development, from conception to publication and distribution.
What are the two types of formularies?
Types of FormulariesOpen Formulary: The payer may provide coverage for all formulary and non-formulary drugs. The payers include the health plan, the employer, or a PBM acting on behalf of the health plan or employer. ... Closed Formulary: Non-formulary drugs are not reimbursed by the payer.
What are the three types of formulary systems?
An open formulary has no limitation to access to a medication. Open formularies are generally large. A closed formulary is a limited list of medications. A closed formulary may limit drugs to specific physicians, patient care areas, or disease states via formulary restrictions.
Is formulary the same as preferred?
A drug formulary is a list of prescription drugs, both generic and brand name, that is preferred by your health plan. Your health plan may only pay for medications that are on this "preferred" list.
Who is responsible for obtaining precertification for a referral to another physician or specialist?
The patientAkin to an official recommendation, referrals are made from one physician to another. The patient is usually responsible for obtaining the original referral from their doctor. Following the request, the physician may simply write a script for treatment that references a specific doctor, such as a specialist.
What is the meaning of formularies?
A list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list.
What is formulary process?
A formulary system is the ongoing process through which a healthcare organization establishes policies regarding the use of drugs, therapies, and drug-related prod- ucts, including medication delivery devices, and identifies those that are most medically appropriate, safe, and cost-effective to best serve the health ...
What is a drug formulary?
A drug formulary is a list of medications covered by a Medicare drug plan. Here are 7 facts about Medicare drug formularies that every beneficiary should know. A Medicare formulary is the list of prescription drugs that are covered by a particular Medicare Part D or Medicare Advantage plan. Each plan includes its own formulary ...
What is tier 1 drug?
Drugs on a Medicare formulary are divided into tiers that determine the cost paid by beneficiaries. For example, a tier 1 drug might consist of low-cost, generic drugs and require only a small copayment in order to fill a prescription.
Does Medicare have to include certain drugs?
You can also request to pay a lower amount for a covered drug. 5. Each formulary must include certain drugs. All Medicare formularies generally must include coverage for at least two different drugs within most drug categories, and they must include all available drugs for the following categories: HIV/AIDS treatments.
Can Medicare formulary change?
A Medicare formulary can change throughout the year. Drugs may be added or removed from the market at any time, and therefore drugs may be added or removed from a plan’s formulary. Drugs may also remain for sale on the market but be removed from a plan’s formulary for a variety of reasons.
Does Medicare have restrictions on prescription drugs?
All Medicare plans with prescription drug coverage must make sure that members have access to all medically necessary drugs listed on their formulary. 7. There are restrictions on some drugs on a formulary. Some drugs on a Medicare formulary come with certain types of restrictions, such as: Prior authorization.
What do pharmacists do when filling prescriptions?
When you fill a prescription at the pharmacy, Medicare drug plans and pharmacists routinely check to make sure the prescription is correct, that there are no interactions, and that the medication is appropriate for you. They also conduct safety reviews to monitor the safe use of opioids and other frequently abused medications. These reviews are especially important if you have more than one doctor who prescribes these drugs. In some cases, the Medicare drug plan or pharmacist may need to first talk to your doctor before the prescription can be filled.
What to do if your prescription is not filled?
If your pharmacy can’t fill your prescription as written, the pharmacist will give you a notice explaining how you or your doctor can call or write to your plan to ask for a coverage decision. If your health requires it, you can ask the plan for a fast coverage decision. You may also ask your plan for an exception to its rules before you go to the pharmacy, so you’ll know if your plan will cover the medication. Visit Medicare.gov/medicare-prescription-drug-coverage-appeals to learn how to ask for an exception.
Does Medicare cover prescription drugs?
Medicare drug plans have contracts with pharmacies that are part of the plan’s “network.” If you go to a pharmacy that isn’t in your plan’s network, your plan might not cover your drugs. Along with retail pharmacies, your plan’s network might include preferred pharmacies, a mail-order program, or an option for retail pharmacies to supply a 2- or 3-month supply.
Does Medicare cover opioids?
Some Medicare drug plans will have a drug management program to help patients who are at risk for prescription drug abuse. If you get opioids from multiple doctors or pharmacies, your plan may talk with your doctors to make sure you need these medications and that you’re using them appropriately. If your Medicare drug plan decides your use of prescription opioids and benzodiazepines may not be safe, the plan will send you a letter in advance. This letter will tell you if the plan will limit coverage of these drugs for you, or if you’ll be required to get the prescriptions for these drugs only from a doctor or pharmacy that you select.
How many drugs does Medicare cover?
All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug. However, in most cases, a similar drug should be available.
How many prescription drugs are covered by Medicare?
Plans include both brand-name prescription drugs and generic drug coverage. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes. This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per ...
What is formulary exception?
A formulary exception is a drug plan's decision to cover a drug that's not on its drug list or to waive a coverage rule. A tiering exception is a drug plan's decision to charge a lower amount for a drug that's on its non-preferred drug tier.
What happens if you don't use a drug on Medicare?
If you use a drug that isn’t on your plan’s drug list, you’ll have to pay full price instead of a copayment or coinsurance, unless you qualify for a formulary exception. All Medicare drug plans have negotiated to get lower prices for the drugs on their drug lists, so using those drugs will generally save you money.
What does Medicare Part D cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary.
What is a tier in prescription drug coverage?
Tiers. To lower costs, many plans offering prescription drug coverage place drugs into different “. tiers. Groups of drugs that have a different cost for each group. Generally, a drug in a lower tier will cost you less than a drug in a higher tier. ” on their formularies. Each plan can divide its tiers in different ways.
What is a drug plan's list of covered drugs called?
A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary. Many plans place drugs into different levels, called “tiers,” on their formularies. Drugs in each tier have a different cost. For example, a drug in a lower tier will generally cost you less than a drug in a higher tier.
How to know what medications are in Medicare Part D?
How to Know What Medications are in a Medicare Part D Formulary. If you have a health insurance agent, they can assist in finding your plan’s formulary list. You can check insurance carrier websites to view the drug formularies they offer. Those with Medicare are eligible for a drug plan and should enroll as soon as possible.
What is Medicare Part D?
The Medicare Part D formulary is a list of drugs that have coverage under your policy. The formulary must include at least two drugs per category, and the insurance company can choose the options.
What does a doctor's report state?
If you’re seeking a tiering exception, your doctor’s report must state that the preferred medications would adversely affect you. If you’re trying to obtain a formulary exception, your doctor’s statement must indicate that the non-formulary drug is necessary.
What is formulary exception?
A Formulary Exception is a form of a request to determine coverage. By obtaining an exception, you may be able to get a drug that’s not on your plan’s formulary or ask your plan to bypass step therapy or prior authorizations.
How many protected classes does an insurance plan cover?
Plans must cover the six protected classes. But, every formulary may not contain your medication. Every insurance plan has its drug formularies. Each medication must adhere to the Food and Drug Administration’s (FDA) regulations.
Can I pay for a drug yourself?
You may pay for the medication yourself. But, sometimes, you can find a manufacturer coupon to help cover the cost. Or, you can file an appeal or request a formulary exception. Then, during AEP, you can change your Part D plan.
Can a doctor prescribe a prescription?
A doctor prescribes a prescription, but it requires prior authorization or step therapy; however, you don’t feel you can meet the requirements. Your plan removes your medication from the formulary, and there aren’t other drugs you can use.
How to get prescription drug coverage
Find out how to get Medicare drug coverage. Learn about Medicare drug plans (Part D), Medicare Advantage Plans, more. Get the right Medicare drug plan for you.
What Medicare Part D drug plans cover
Overview of what Medicare drug plans cover. Learn about formularies, tiers of coverage, name brand and generic drug coverage. Official Medicare site.
How Part D works with other insurance
Learn about how Medicare Part D (drug coverage) works with other coverage, like employer or union health coverage.