Always review your Medicare Summary Notice (MSN) or health insurance Explanation of Benefits (EOB) for errors or mistakes. Use our MSN decoder to understand what’s in your summary notice. Check past MSNs or EOBs to see whether there's a pattern of billing issues. Contact the provider.
Full Answer
How do I complain about medical billing errors?
The U.S. Department of Health and Human Services – Office of the Inspector General. Provider fraud or abuse in a Medicare Advantage Plan or a Medicare drug plan (including a fraudulent claim) 1-800-MEDICARE (1-800-633-4227) or. The Investigations Medicare Drug …
How do I report a billing scam to Medicare?
Billing Medicare for appointments patients fail to keep Defrauding the Federal Government and its programs is illegal. Committing Medicare fraud ... in incorrect coding, ordering excessive diagnostic tests, upcoding, or billing for services or supplies not provided may be subject to administrative, civil, or criminal liability. ...
What happens if my doctor doesn't pick the right diagnosis code?
Check past MSNs or EOBs to see whether there's a pattern of billing issues. Contact the provider. It could be an error that your provider will correct, or he or she may explain why the coding is correct. If you have Medicare and need help, you can contact your local Senior Medicare Patrol (SMP). Trained SMP volunteers take complaints about potential health care fraud, investigate …
What should I do if my provider is not billing accurately?
Mar 18, 2016 · If at any time you receive a bill you do not think you should be required to pay, contact your healthcare provider's office. It is possible they have used the wrong ICD-10 code. Your healthcare provider may be able to change the diagnosis code to one that gives you the coverage you need. If ICD-10 coding is not the reason for the billing issue ...

Why do billing errors happen?
Because there are thousands of billing codes, mistakes can happen. These billing errors can be fixed if you call the mistake to the attention of the provider. By changing the codes, providers can get paid differing amounts of money. When providers use the correct codes for the procedures actually done, they get paid what they are due.
What is the billing code for a procedure?
Each procedure that your doctor or other health care provider performs has a billing code. This code is called the CPT code or Current Procedural Terminology. Providers use these codes when they submit claims to insurance companies or Medicare. The code determines how much your provider will be paid. Because there are thousands of billing codes, ...
What is a CPT code?
Each procedure that your doctor or other health care provider performs has a billing code. This code is called the CPT code or Current Procedural Terminology. Providers use these codes when they submit claims to insurance companies or Medicare. The code determines how much your provider will be paid. Because there are thousands of billing codes, mistakes can happen. These billing errors can be fixed if you call the mistake to the attention of the provider. By changing the codes, providers can get paid differing amounts of money. When providers use the correct codes for the procedures actually done, they get paid what they are due.
What is the ICD code?
The International Classification of Diseases (ICD) is a toolbox of diagnosis codes that is used worldwide to track disease and mortality rates. Standardizing diagnosis codes improves the ability to track health initiatives, monitor health trends, and respond to health threats. 1
When did ICD-10 come out?
The World Health Organization released ICD-10 in 1999. The United States, however, was slow to adopt the most recent codes and did not transition from ICD-9 to ICD-10 until October 2015. The number of possible codes your healthcare provider must choose from exponentially increased in October 2015. There are more than 155,000 codes available in ...
Who is Elaine Hinzey?
Elaine Hinzey is a fact checker, writer, researcher, and registered dietitian. It takes years of education and training to teach doctors the skills needed to evaluate a patient, make a diagnosis, and treat that person according to the standard of care.
Does insurance cover prostate cancer?
Insurance covers certain services by gender. For example, cervical, ovarian, and uterine cancers are specific to women and prostate and testicular cancers to men. This is based on anatomy. Screening tests and treatments for these conditions, for the purposes of insurance coverage, are generally binary.
How many ICD-10 codes are there for rhinitis?
Allergic rhinitis (a runny nose from allergies) has at least six different codes from which to choose, pneumonia 20 codes, asthma 15 codes, influenza 5 codes, sinusitis 21 codes, and sore throat 7 codes. 5 Those are the easy ones.
How often is Medicare billed?
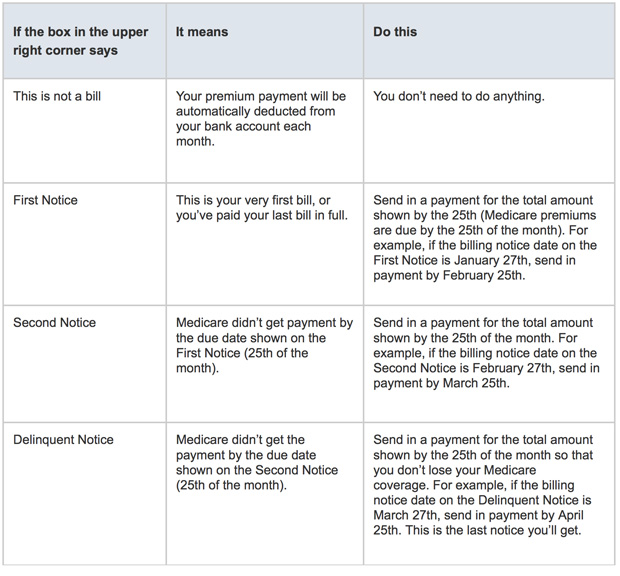
Some people with Medicare are billed either monthly or quarterly. If you are billed for Part A or IRMAA Part D, you will be billed monthly. If this box says:
Does Medicare end if you don't send past due?
The date your Medicare Insurance will end if you do not send the ‘past due amount’ by the date shown. You’ll only see a termination date(s) on a bill that says “Delinquent” at the top.
What to do if you suspect someone has been fraudulently billed?
If you suspect that a friend or family member—e.g., an aging parent—may have been fraudulently billed, talk with them about the bill. You can also enlist the services of a medical billing advocate on their behalf .
Does insurance pay for medical bills?
In almost all circumstances, your insurance company will be paying for the majority of your medical bill, so they'll be very interested to hear about suspected fraud. Your insurance company will contact the doctor or hospital and inquire about the suspicions medical procedures or tests you've been billed for.
Is WikiHow a copyright?
All rights reserved. wikiHow, Inc. is the copyright holder of this image under U.S. and international copyright laws. This image is <b>not</b> licensed under the Creative Commons license applied to text content and some other images posted to the wikiHow website.
What is Medicare Advantage reimbursement?
Medicare Advantage organizations, Cost plans, and PACE organizations are required to reimburse non-contract providers for Part A and Part B services provided to Medicare beneficiaries with an amount that is no less than the amount that would be paid under original Medicare.
What is a non contract provider?
Non-contract providers are required to accept as payment, in full, the amounts that the provider could collect if the beneficiary were enrolled in original Medicare. Plans should refer to the MA Payment Guide for Out of Network Payments in situations where they are required to pay at least the Medicare rate to out of network providers.
What to do if your Medicare records don't match?
Whenever you see something that does not match up with your records, reach out to your doctor or medical office for clarification. There could have been a misunderstanding or a true billing error. In the worst-case scenario, it could be a sign of Medicare fraud and abuse.
How often do you get a Medicare summary notice?
The Medicare Summary Notice. If you are on Original Medicare (Part A and Part B), you will receive a Medicare Summary Notice (MSN) quarterly, i.e., every 3 months. You will receive separate MSNs for Part A and Part B coverage.
What is an EOB for Medicare?
The document you receive is called an Explanation of Benefits (EOB). Your commercial Medicare plan will mail you an EOB monthly. Similar information will be presented to you as on the Medicare Summary Notice. Like an MSN, an EOB is not a bill.
What is MSN bill?
An MSN is a detailed statement about services that have been charged to Medicare during that time frame but is not a bill in and of itself. THIS IS NOT A BILL will be printed in bold capitalized letters at the top of the statement.
When does a benefit period end?
It ends when you have not received inpatient hospital or skilled nursing facility care for 60 days in a row. You will pay a deductible for each benefit period and multiple deductibles may be listed here.
Who is Ashley Hall?
Ashley Hall is a writer and fact checker who has been published in multiple medical journals in the field of surgery. Learn about our editorial process. Ashley Hall. on December 14, 2020. You do not want to pay more than necessary, but if you don't read your Medicare bill, you could do just that.
What to do if you are not getting a resolution on your medical billing?
Finally, the last step, if you're still not getting resolution on your medical billing dispute is to seek legal counsel. You will want to find an attorney that specializes in medical billing disputes.
How to make progress on disputing medical bills?
If you're covered and using your insurance to pay for a medical procedure (or at least part of it), a great way to make progress on disputing your medical bill is to also file an appeal with your insurance company.
What is the first thing you get before your medical bill arrives?
The first thing you get (typically before your medical bill even arrives) is your explanation of benefits from your insurance company. I would venture that 95% of people throw these away and don't even know what they are for.
What is a patient advocate?
Depending on your medical provider, they may have a patient advocate that could help you reduce your bill, help expedite resolution of errors, and more. Patient advocates are usually found in hospitals and large medical provider networks (like HMOs) that serve a lot of patients.
What is the explanation of benefits?
Amount you will owe the provider. Most explanation of benefits forms will also include information about your deductible, co-pay, co-insurance, and more. If a procedure is not covered, the explanation of benefits will also typically have a code or error, with a short explanation as to why it's not covered.
Review the itemized bill
Never pay a medical bill that doesn’t itemize each charge. For example, the bill might show a charge of $160 for an office visit, another $160 for a biopsy and a separate $160 for a visit to the same doctor on a different date.
Compare the Explanation of Benefits
Most insurance companies send an explanation of benefits (EOB) after receiving your claim from a hospital, doctor or other healthcare provider. The EOB may look like a bill and even show an amount owed under “patient responsibility” or a similar term. But don’t pull out your credit or debit card yet, since the EOB isn’t a bill.
Ensure accuracy of medical codes
Make sure that the coding, the numerical and/or alphabetical code used to specify the visit, procedure or other service received, is correct on your EOB and/or the medical bill from the doctor, hospital or other health care provider, since that code tells the billing office how much to bill.
Keep an eye out for duplicate bills
Depending on the nature of the doctor’s visit, hospital stay or procedure, you could have medical bills rolling in for months afterward from multiple doctors, pathology labs and other health care providers. With so many different bills, it’s easy to just want to pay them all right away to ease your medical bill headache.
Watch out for canceled work
Doctors’ offices are busy places, and if your doctor ordered a shot, vaccine or other procedure and then canceled it for some reason, you could still be billed for the canceled work if the order wasn’t changed in your records. If you see a charge for work that never occurred, call the billing office and explain.
About the Author
Deb Hipp is a full-time freelance writer based in Kansas City, Mo. Deb went from being unable to get approved for a credit card or loan 20 years ago to having excellent credit today and becoming a homeowner. Deb learned her lessons about money the hard way.