Full Answer
What is a Medicare formulary and how does it work?
A formulary is simply a list of covered prescription drugs. If your prescription drug is not on the plan formulary, you may have to pay for it 100% out-of-pocket. You can usually get a copy of the formulary by calling your plan or looking on your plan’s website. Medicare formulary tiers.
Can my planners change my drug formularies?
Plans can change their formularies at any time. Your plan may notify you of any formulary changes that affect drugs you’re taking. Medicare drug coverage includes drugs for medication-assisted treatment for opioid use disorders. It also covers drugs like methadone and buprenorphine when prescribed for pain.
Do Medicare Part D plans have formularies?
Both Medicare Advantage plans and stand-alone Medicare Part D Prescription Drug Plans have formularies. A Medicare Part D formulary is simply a list of covered prescription drugs and vaccines. The formulary may change at any time, but your plan will notify you when necessary.
What are the requirements for a Medicare formulary?
All Medicare formularies generally must include coverage for at least two different drugs within most drug categories, and they must include all available drugs for the following categories: A Medicare formulary won’t include over-the-counter drugs or weight-loss drugs.
Who Develops Medicare formularies?
the Blue Shield Pharmacy and TherapeuticsThe formulary is developed and updated regularly by the Blue Shield Pharmacy and Therapeutics (P&T) Committee and meets all Medicare requirements for included and excluded drugs.
Who sets the formulary?
A drug formulary is a list of generic and brand-name prescription drugs covered by a health plan. The health plan generally creates this list by forming a pharmacy and therapeutics committee consisting of pharmacists and physicians from various medical specialties.
How is a formulary determined?
Formulary Development. The medications and related products listed on a formulary are determined by a pharmacy and therapeutics (P&T) committee or an equivalent entity. P&T committees are comprised of primary care and specialty physicians, pharmacists and other professionals in the health care field.
Who decides what tier a drug is?
Every plan creates its own formulary structure, decides which drugs it will cover and determines which tier a drug is on. One plan may cover a drug that another doesn't. The same drug may be on tier 2 in one plan's formulary and on tier 3 in a different plan's formulary. Formularies change.
What is a formulary agent?
Typically, a team of medical professionals approves the drugs on a health plan's formulary based on safety, quality, and cost-effectiveness. The team is made up of pharmacists and physicians who review new and existing medications. Sometimes health plans choose not to cover a prescription drug.
What does a formulary pharmacist do?
Formulary management. The formulary pharmacist's other significant role is the maintenance and update of the trust formulary. The formulary pharmacist is usually involved at every stage of formulary development, from conception to publication and distribution.
Which committee develops a formulary for an institution?
The P&T committee is responsible for developing, managing, updating and administering the formulary. The P&T committee also designs and implements formulary system policies on utilization and access to medications.
How often are formularies updated?
There are also some instances where the same product can be made by two or more manufacturers, but greatly vary in cost. In these instances, only the lower cost product may be covered. How often is the Formulary updated? Formulary changes typically occur twice per year.
Why do formularies change?
Formulary changes happen from time to time if drugs are: Recalled from the market; Replaced by a new generic drug; or, Clinical restrictions are added, including, but not limited to, prior authorization, quantity limits or step therapy.
Why do formularies exist?
Formularies are tools used by purchasers to limit drug coverage based on favorable clinical performance and relative cost.
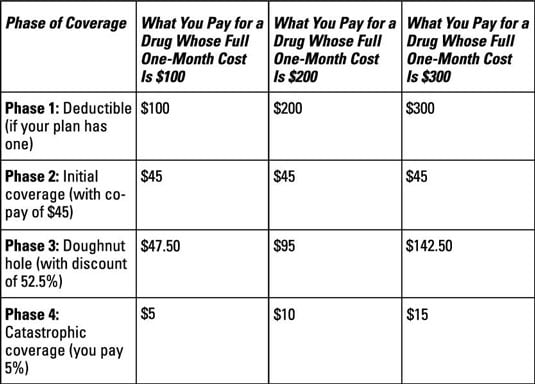
What is the Doughnut hole for 2021?
For 2021, the coverage gap begins when the total amount your plan has paid for your drugs reaches $4,130 (up from $4,020 in 2020). At that point, you're in the doughnut hole, where you'll now receive a 75% discount on both brand-name and generic drugs.
What is the purpose of formularies?
Formularies establish prescriptive norms and improve quality by optimizing the selection of agents with the highest therapeutic value at the lowest possible cost. In the hospital or health system, drug formularies serve the purposes of minimizing variation and improving the level of prescribing performance.
What is a formulary for prescription drugs?
A formulary is simply a list of covered prescription drugs. If your prescription drug is not on the plan formulary, you may have to pay for it 100% out-of-pocket. You can usually get a copy of the formulary by calling your plan or looking on your plan’s website.
When does a formulary change?
A formulary may change when a new more cost-effective prescription drug comes to market or when new safety information about a prescription drug is released.
How many tiers of Medicare are there?
A Medicare formulary may categorize prescription drugs into five tiers: Tier 1– preferred generic: These are the prescription drugs that typically have the lowest cost share for you.
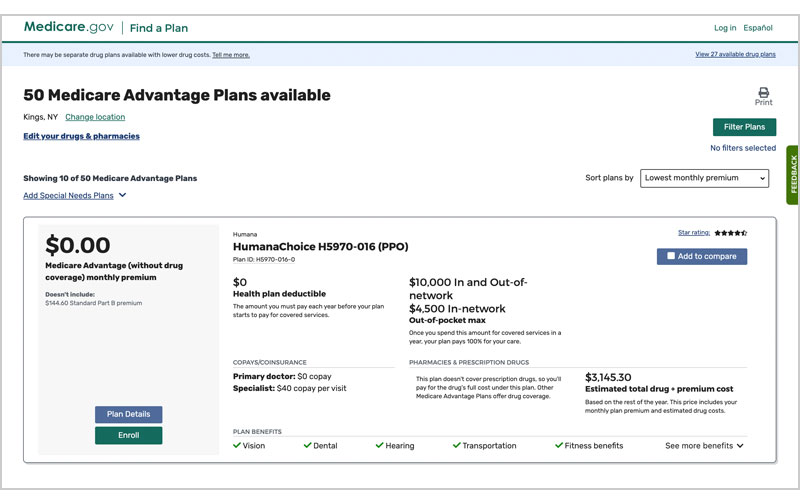
How to know if Medicare Advantage covers all prescriptions?
If you have a stand-alone Part D Prescription Drug Plan or a Medicare Advantage prescription drug plan from a private insurance company, you may assume that all your prescription drugs will be covered. One way to know in detail what prescription drugs your plan covers is to check the plan’s formulary. A formulary is simply a list of covered ...
What is covered by Part D?
This means that if you are about to get an organ transplant, if you are suffering from depression or other mental health conditions, if you have seizures or an HIV infection, or if you need certain types of treatment for a precancerous condition, some of your medications will usually be covered by your Part D plan.
Is Medicare formulary covered by prescription drugs?
Prescription drugs not included in the Medicare formulary. If your prescription drug is not covered by your plan’s formulary, you have some options. You can contact the plan and ask them for a list of similar prescription drugs they do cover. You can bring the list to your doctor and ask him or her to prescribe a similar drug ...
Can a manufacturer remove a prescription drug from the market?
However, if the Food and Drug Administration (FDA) decides your prescription drug is unsafe or the manufacturer removes the prescription drug from the market, the plan may remove it from the formulary immediately.
How long does it take for a Medicare plan to change formulary?
Please keep in mind that a plan may change its drug formulary at any time, but Medicare requires that the plan gives you a written notification at least 60 days before the change occurs.
How is formulary pricing determined?
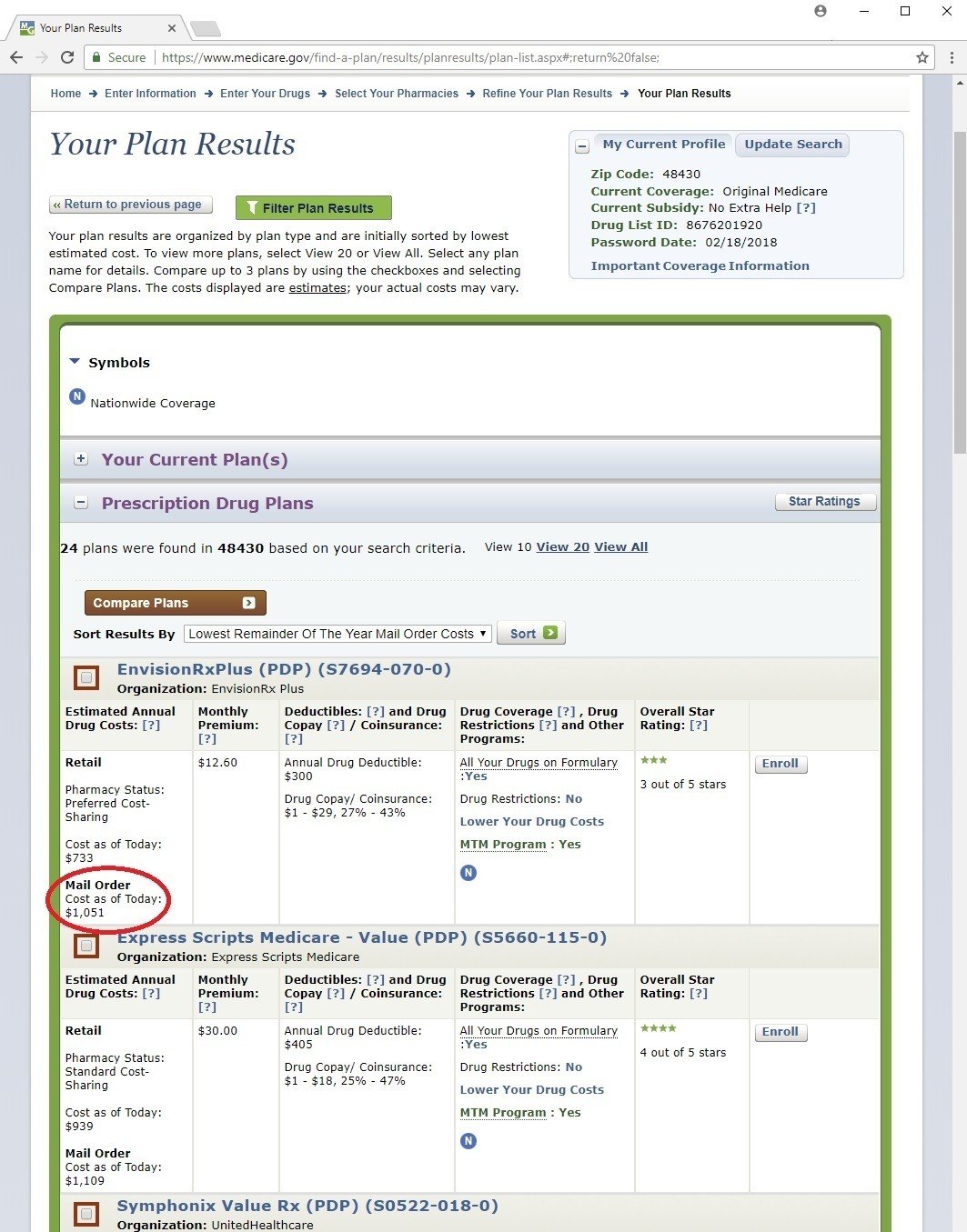
Because each plan is administered by a private insurance company contracted with Medicare, prescription drug formulary pricing is determined by the individual plan. One of the more common is the tiered approach to formulary prices, in which different types and classes of prescription drugs have different copayments.
What is Medicare Part D?
Each Medicare Part D Prescription Drug Plan must develop a drug formulary to cover a broad range of the most commonly prescribed medications, including both brand-name and generic formulations, to ensure that people with common conditions can get the treatment they need.
Which tier of a drug formulary has the lowest copayment?
For example, tier 1, which typically includes mainly generic drugs, would have the lowest copayment, followed by tier 2 for preferred brand-name prescription drugs with a slightly higher copayment. Tier 3 is the most expensive drug formulary tier, which might include the most expensive and unique medications and non-preferred brand-name ...
How to contact Medicare about appeal?
You can also get more information about the appeals by calling Medicare directly at 1-800-MEDICARE (1-800-633-4227) . TTY users should call 1-877-486-2048. Representatives are available 24 hours a day, seven days a week.
Does Medicare require private insurance?
Medicare requires that every private insurance company approved to offer Medicare Part D Pre scription Drug Plans provide a certain minimum level of coverage. However, the individual companies have some flexibility in deciding which prescription drugs they will cover and how much they will charge for each. This list of covered prescription drugs and ...
Do generic drugs have the same ingredients?
These generic prescription drug formulary medications, according to the Food and Drug Administration (FDA), must have the “ same active ingredient, strength, dosage form, and route of administration, performance characteristics ...
What do pharmacists do when filling prescriptions?
When you fill a prescription at the pharmacy, Medicare drug plans and pharmacists routinely check to make sure the prescription is correct, that there are no interactions, and that the medication is appropriate for you. They also conduct safety reviews to monitor the safe use of opioids and other frequently abused medications. These reviews are especially important if you have more than one doctor who prescribes these drugs. In some cases, the Medicare drug plan or pharmacist may need to first talk to your doctor before the prescription can be filled.
What to do if your prescription is not filled?
If your pharmacy can’t fill your prescription as written, the pharmacist will give you a notice explaining how you or your doctor can call or write to your plan to ask for a coverage decision. If your health requires it, you can ask the plan for a fast coverage decision. You may also ask your plan for an exception to its rules before you go to the pharmacy, so you’ll know if your plan will cover the medication. Visit Medicare.gov/medicare-prescription-drug-coverage-appeals to learn how to ask for an exception.
Does Medicare cover prescription drugs?
Medicare drug plans have contracts with pharmacies that are part of the plan’s “network.” If you go to a pharmacy that isn’t in your plan’s network, your plan might not cover your drugs. Along with retail pharmacies, your plan’s network might include preferred pharmacies, a mail-order program, or an option for retail pharmacies to supply a 2- or 3-month supply.
Does Medicare cover opioids?
Some Medicare drug plans will have a drug management program to help patients who are at risk for prescription drug abuse. If you get opioids from multiple doctors or pharmacies, your plan may talk with your doctors to make sure you need these medications and that you’re using them appropriately. If your Medicare drug plan decides your use of prescription opioids and benzodiazepines may not be safe, the plan will send you a letter in advance. This letter will tell you if the plan will limit coverage of these drugs for you, or if you’ll be required to get the prescriptions for these drugs only from a doctor or pharmacy that you select.
What is a formulary in Medicare?
The Medicare & You handbook defines a formulary as “a list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits.”. Most people simply refer to it as a drug list.
How long do you have to give a prescription drug plan to change the formulary?
Coverage rules and costs can change. Brand name drugs can be replaced by generic drugs. In these cases, the plan should give you at least 30 days of notice in writing before the effective date.
What is Medicare Part D?
Medicare Part D is the prescription drug coverage for Medicare recipients. Part D plans are designed to defray the cost of your medications, but they do not kick in automatically when you enroll in Medicare Parts A and B. Once eligible, you would apply for the coverage through a private insurance company. Though all Part D plans are required ...
Why is formulary inclusive?
Cost savings is the reason a formulary inclusive of your medications is important. The drugs on these lists reflect those for which plans negotiate for the best price. The consequence of non-compliance with the list of covered drugs may result in your responsibility for full price versus a copayment or coinsurance.
How long do you have to give a drug plan before the effective date?
Brand name drugs can be replaced by generic drugs. In these cases, the plan should give you at least 30 days of notice in writing before the effective date. Sometimes, the Food and Drug Administration (FDA) decides certain drugs are unsafe.
What to do if your insurance does not include your drug?
If the list of covered drugs does not include your specific drug, it will usually include one that is comparable. Consult with your physician in this case . If necessary, submit an exception request to your plan administrator.
Do all Part D plans have the same coverage?
Though all Part D plans are required to comply with the same standard federal government guidelines, there are differences in cost and coverage . Therefore, it is best to do some comparison shopping before making a decision. The first step is to look at each plan’s formulary.
When will Medicare start paying for insulin?
Starting January 1, 2021, if you take insulin, you may be able to get Medicare drug coverage that offers savings on your insulin. You could pay no more than $35 for a 30-day supply. Find a plan that offers this savings on insulin in your state. You can join during Open Enrollment (October 15 – December 7, 2020).
What is a drug plan's list of covered drugs called?
A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary. Many plans place drugs into different levels, called “tiers,” on their formularies. Drugs in each tier have a different cost. For example, a drug in a lower tier will generally cost you less than a drug in a higher tier.
What is formulary exception?
A formulary exception is a drug plan's decision to cover a drug that's not on its drug list or to waive a coverage rule. A tiering exception is a drug plan's decision to charge a lower amount for a drug that's on its non-preferred drug tier.
What happens if you don't use a drug on Medicare?
If you use a drug that isn’t on your plan’s drug list, you’ll have to pay full price instead of a copayment or coinsurance, unless you qualify for a formulary exception. All Medicare drug plans have negotiated to get lower prices for the drugs on their drug lists, so using those drugs will generally save you money.
How many prescription drugs are covered by Medicare?
Plans include both brand-name prescription drugs and generic drug coverage. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes. This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per ...
What does Medicare Part D cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary.
How many drugs does Medicare cover?
All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug. However, in most cases, a similar drug should be available.
What is Medicare Part D formulary?
A Medicare Part D formulary is simply a list of covered prescription drugs and vaccines. The formulary may change at any time, but your plan will notify you when necessary.
When is open enrollment for Medicare Part D?
You can do this during the Open Enrollment Period October 15 to December 7 each year. Appeal the coverage decision.
What prescription drugs are excluded from Medicare Part D?
What prescription drugs are excluded from all Medicare Part D formularies? A non-exhausting list of prescription drugs excluded from Medicare Part D formularies include: Medications for weight loss or weight gain. Medications for cosmetic purposes or hair growth. Medications for symptomatic relief of cough and colds.
What if my prescription is not covered by my Medicare?
What if my prescription drug is not covered by my Medicare Part D formulary? If your prescription drug is not on your Medicare Part D formulary, you may have to pay for that prescription drug out of pocket. Your other options are to: Switch Medicare Advantage or Medicare Part D plans to one that does cover your medication.
Why are antineoplastics covered by the CMS?
Antineoplastics (to inhibit growth and spread of precancerous cells, cancer cells, or tumors) According to the Centers for Disease Control and Prevention (CMS) these drugs must be covered to “mitigate the risks and complications associated with an interruption of therapy for these vulnerable populations.”.
What is tier 5 in insurance?
Tier 5 – specialty: these are the highest cost drugs, including some injectables. Tier 6 – Select care drugs: the copayment may actually be lower than tier 1 drugs. Your plan might let you know when your prescription drug is moved to a higher cost-sharing tier.
Can you appeal a Medicare coverage decision?
According the Centers for Medicare and Medicaid Services (CMS) you have the right to ask your plan to pay for a prescription drug you think should be covered, provided, or continued. Working with your provider, you can ask for an exception. Learn more about Medicare appeals.
What is formulary exception?
A formulary exception is a drug plan's decision to cover a drug that's not on its drug list or to waive a coverage rule. A tiering exception is a drug plan's decision to charge a lower amount for a drug that's on its non-preferred drug tier.
How long can you have opioids on Medicare?
First prescription fills for opioids. You may be limited to a 7-day supply or less if you haven’t recently taken opioids. Use of opioids and benzodiazepines at the same time.
What is the purpose of a prescription drug safety check?
When you fill a prescription at the pharmacy, Medicare drug plans and pharmacists routinely check to make sure the prescription is correct, that there are no interactions, and that the medication is appropriate for you. They also conduct safety reviews to monitor the safe use of opioids ...
What happens if a pharmacy doesn't fill a prescription?
If your pharmacy can’t fill your prescription as written, the pharmacist will give you a notice explaining how you or your doctor can call or write to your plan to ask for a coverage decision. If your health requires it, you can ask the plan for a fast coverage decision.
Does Medicare cover opioid pain?
There also may be other pain treatment options available that Medicare doesn’t cover. Tell your doctor if you have a history of depression, substance abuse, childhood trauma or other health and/or personal issues that could make opioid use more dangerous for you. Never take more opioids than prescribed.
Do you have to talk to your doctor before filling a prescription?
In some cases, the Medicare drug plan or pharmacist may need to first talk to your doctor before the prescription can be filled. Your drug plan or pharmacist may do a safety review when you fill a prescription if you: Take potentially unsafe opioid amounts as determined by the drug plan or pharmacist. Take opioids with benzodiazepines like Xanax®, ...
Does Medicare cover prescription drugs?
In most cases, the prescription drugs you get in a Hospital outpatient setting, like an emergency department or during observation services , aren't covered by Medicare Part B (Medical Insurance). These are sometimes called "self-administered drugs" that you would normally take on your own. Your Medicare drug plan may cover these drugs under certain circumstances.