Full Answer
What is the maximum premium for Medicare Part B?
The standard monthly premium for Part B, which covers outpatient care and durable equipment ... or offers a different copay and an out-of-pocket maximum (a Medicare Advantage Plan). The Aduhelm situation highlights the ripple effect that expensive drugs ...
How much does Part B insurance cost?
Part B costs: What you pay 2021: Premium $170.10 each month (or higher depending on your income). The amount can change each year. You’ll pay the premium each month, even if you don’t get any Part B-covered services.
How much does Medicare Part B costs?
and Part B which covers doctor’s visits and other medical services, and costs $170.10 per month for most enrollees in 2021. Everyone is eligible for Medicare at age 65, even if your full Social ...
Does Medicare Part B cost money?
• Part B Medicare Part B has a monthly premium. The amount you pay depends on your yearly income. Most people pay the standard premium amount of $144.60 (as of 2020) because their individual income is less than $87,000.00, or their joint income is less than $174,000.00 per year.
What is Part B?
What are the factors that determine Medicare coverage?
What is national coverage?
About this website
Is Medicare Part B an HMO?
A Medicare Advantage HMO plan delivers all your Medicare Part A and Part B benefits, except hospice care – but that's still covered for you directly under Part A, instead of through the plan. Medicare Advantage plans are offered by private, Medicare-approved insurance companies.
What does a Medicare HMO cover?
A Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan's network (except emergency care, out-of-area urgent care, or out-of-area dialysis).
Is Medicare Part B acquired through private insurers?
Medicare Supplement (Medigap) policies are sold by private insurance companies to work alongside your Medicare Part A and Part B (Original Medicare) benefits. These plans can help pay your Original Medicare out-of-pocket expenses, such as deductibles, copayments, and coinsurance.
What is Part B of Medicare funded by?
Part B, the Supplementary Medical Insurance (SMI) trust fund, is financed through a combination of general revenues, premiums paid by beneficiaries, and interest and other sources. Premiums are automatically set to cover 25 percent of spending in the aggregate, while general revenues subsidize 73 percent.
Which is better PPO or HMO?
HMO plans typically have lower monthly premiums. You can also expect to pay less out of pocket. PPOs tend to have higher monthly premiums in exchange for the flexibility to use providers both in and out of network without a referral. Out-of-pocket medical costs can also run higher with a PPO plan.
What is the difference between Medicare and HMO?
There are differences between Medicare Advantage plans. The specific structure of the plan you choose dictates how much you pay for care and where you can seek treatment. HMO plans limit you to a specific network of providers, while PPO plans offer lower rates to beneficiaries who seek care from a preferred provider.
Can I have Medicare and private insurance at the same time?
It is possible to have both private insurance and Medicare at the same time. When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer.
What is the best supplemental insurance for Medicare?
Best Medicare Supplement Insurance Companies of 2022Best Overall: Mutual of Omaha.Best User Experience: Humana.Best Set Plans and Coverage: AARP.Best Medigap Coverage Information: Aetna.Best Discounts for Multiple Policyholders: Cigna.
When should I apply for Medicare Part B?
Part B (Medical Insurance) Generally, you're first eligible to sign up for Part A and Part B starting 3 months before you turn 65 and ending 3 months after the month you turn 65. (You may be eligible for Medicare earlier, if you get disability benefits from Social Security or the Railroad Retirement Board.)
Who pays for Medicare coverage?
Medicare is funded by the Social Security Administration. Which means it's funded by taxpayers: We all pay 1.45% of our earnings into FICA - Federal Insurance Contributions Act - which go toward Medicare. Employers pay another 1.45%, bringing the total to 2.9%.
What is Medicare Part B also known as?
Medicare Part B (also known as medical insurance) is an insurance plan that covers medical services related to outpatient and doctor care.
Who pays for Medicare Part A?
Most people receive Medicare Part A automatically when they turn age 65 and pay no monthly premiums. If you or your spouse haven't worked at least 40 quarters, you'll pay a monthly premium for Part A.
2021 Medicare Parts A & B Premiums and Deductibles | CMS
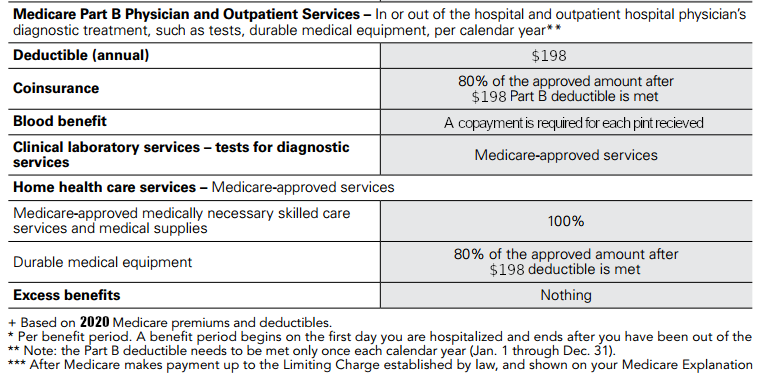
On November 6, 2020, the Centers for Medicare & Medicaid Services (CMS) released the 2021 premiums, deductibles, and coinsurance amounts for the Medicare Part A and Part B programs. Medicare Part B Premiums/Deductibles Medicare Part B covers physician services, outpatient hospital services, certain home health services, durable medical equipment, and certain other medical and health services ...
Medicare Part B Coverage - OPM.gov
Medicare Part B Coverage Do I Have to Take Part B Coverage? You don't have to take Part B coverage if you don't want it, and your FEHB plan can't require you to take it.
Medicare Part B Covered Medications - HealthPartners
t. o determine Part B . or Part D coverage, except for drugs flagged with an asterisk. Clinical PA also required for drugs flagged with a PA. Part D Crossover Drug: Drugs will be covered under Part D when prescribed
What is Medicare Part B? | HHS.gov
Medicare Part B helps cover medical services like doctors' services, outpatient care, and other medical services that Part A doesn't cover.Part B is optional. Part B helps pay for covered medical services and items when they are medically necessary. Part B also covers some preventive services like exams, lab tests, and screening shots to help prevent, find, or manage a medical problem.
CMS Releases 2022 Premiums and Cost-Sharing Information for Medicare ...
The Centers for Medicare & Medicaid Services (CMS) released the 2022 premiums, deductibles and other key information for Medicare Advantage and Part D prescription drug plans in advance of the annual Medicare Open Enrollment to help Medicare enrollees decide on coverage that fits their needs.
What is an HMO plan?
Summary. Medicare health maintenance organization (HMO) plans are a type of Medicare Advantage plan. The plans are offered by private insurance companies, with varied coverage and costs. In this article, we discuss Medicare Advantage, look at the HMO plans, and examine how they compare with original Medicare.
How much is the HMO premium in 2021?
Advantage HMO plans may offer premium-free plans, or a person may have to pay the premium. A person has to pay the Medicare Part B monthly premium, which is $148.50 in 2021. Some plans cover the premium. The deductible for the HMP plan may be as low as zero, depending on the plan.
What is HMOPOS in healthcare?
In addition to plans such as the health maintenance organization (HMO) and HMO point-of-service (HMOPOS) plans, the program offers: Advantage healthcare plans are offered by private companies that must follow Medicare rules and offer the same benefits as original Medicare (Part A and Part B).
What is Medicare Advantage?
Medicare Advantage plans combine the benefits of parts A and B and may offer prescription drug coverage. The Balanced Budget Act of 1997 added a new Part C to Medicare called the Medicare+choice program. It included various coordinated healthcare plans, including health maintenance organizations (HMOs). The Medicare+choice program is now known as ...
What is Advantage Healthcare?
Advantage healthcare plans are offered by private companies that must follow Medicare rules and offer the same benefits as original Medicare (Part A and Part B). Many also offer prescription drug coverage.
What is the focus of HMO?
The focus of HMO plans is on prevention and wellness. They provide coordinated care, often using care managers within the company or a primary care doctor. Usually, the doctors and other service providers must either contract with, or work for, the company offering the HMP plan.
What is receivership in Medicare?
The Centers for Medicare and Medicaid Services (CMS) added two special enrollment periods for a person enroll ed in an Advantage plan who has a consistent record of poor performance, or is having financial problems and the assets are held by a third party called receivership.
What is Medicare Advantage HMO?
What are they? Medicare Advantage HMOs are popular options for additional coverage not offered by original Medicare. In a Medicare Advantage HMO plan, services are limited to to in-network providers. There are many different Medicare Advantage HMO plans to choose from in each state.
What happens if you enroll in a Medicare Advantage HMO?
If you enroll in a Medicare Advantage HMO, your care will be provided by in-network providers. Let’s look at what Medicare Advantage HMO plans offer, how to enroll, and some of the advantages and disadvantages of choosing a Medicare Advantage HMO plan over original Medicare.
How much does a PCP visit cost with Medicare Advantage?
When you enroll in a Medicare Advantage HMO plan, there are different copayment amounts for PCP and specialist visits. Copayments can range from about $0 to $50 per visit, depending on the plan and provider.
What is the popularity of HMO plans?
In most major cities, you can easily find plans that have low-cost premiums, deductibles, and copayments. The popularity of Medicare HMO plans also means that you will have a wide in-network selection of providers to choose from.
How much is Medicare Advantage deductible?
Medicare Advantage HMO plans generally have their own in-network deductible amounts, which can start as low as $0. If your plan covers prescription drugs, you can expect to see a drug deductible amount, as well.
What is Medicare Part D?
prescription drug coverage ( Medicare Part D) dental, vision, and hearing coverage. additional health coverage, such as home meal delivery or fitness memberships. To enroll in a Medicare Advantage HMO plan, you must already be enrolled in Medicare parts A and B.
What are the disadvantages of Medicare Advantage?
Disadvantages of Medicare Advantage HMOs. There is less provider flexibility with HMOs compared with other Medicare Advantage plans. You will be required to choose a primary care physician (PCP) when you enroll in the plan, which may mean switching from your current doctor.
What Does Part B Of Medicare Cover in 2022?
Part B of Medicare covers doctor’s bills, outpatient hospital services, durable medical equipment, and other medically-related goods and services.
Enrolling in Medicare Part B
Americans 65 or older are eligible for the Federal Medicare Program, particularly Parts A and B Medicare coverage.
Medicare Part B FAQs
Medicare Part B helps cover medically-necessary services like doctors’ services and tests, outpatient care, home health services, durable medical equipment, and other medical services.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
Who pays first Medicare?
Rules on who pays first. Medicare pays first if you: Have retiree insurance, i.e., from former employment (you or your spouse). Are 65 or more, have group health coverage based on employment (you or your spouse), and the company employs 20 people or less.
How many employees does a group health plan have?
Your group health plan pays first if you: Are 65 or more, have group health coverage based on employment (you or your spouse), and the company employs 20 people or more . Are under 65 and have a disability, have coverage based on current employment (you or a family member), and the company has 100 employees or more.
What is Part B?
Part B covers 2 types of services. Medically necessary services: Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice. Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best.
What are the factors that determine Medicare coverage?
Medicare coverage is based on 3 main factors 1 Federal and state laws. 2 National coverage decisions made by Medicare about whether something is covered. 3 Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
