Who is eligible for Medicare?
You are typically eligible for Medicare when you turn 65 if you are a U.S. citizen or permanent legal resident. You can become eligible at a younge...
When are you eligible for Medicare?
You have a window to enroll in Medicare that begins three months before the month of your 65th birthday and ends three months after. You may be aut...
Does income affect eligibility for Medicare?
Income does not affect your eligibility for Medicare but may impact how much you pay for it. Your Part B premium, which is typically $170.10 in 202...
Is Medicare enrollment automatic at age 65?
Medicare enrollment is automatic only if you are already receiving Social Security benefits. If you have not received Social Security benefits, you...
Do I have to sign up for Medicare when I turn 65?
If you have health insurance through your or your spouse’s employer, you may not have to enroll in Medicare when you turn 65.If the employer has 20...
What happens if I miss my Medicare enrollment?
If you miss your initial or special enrollment periods, you can still enroll in Medicare during the next open enrollment period. But you may incur...
When will I get my Medicare card?
If you actively enroll, you will get your Medicare card about three weeks after you sign up. If you are already receiving Social Security benefits...
When is the Medicare open enrollment period?
The Medicare open enrollment period is Oct. 15 to Dec. 7 each year. You will be able to enroll in Medicare coverage during that time if you didn't...
How old do you have to be to get Medicare?
If you are age 65 or older, you are generally eligible to receive Medicare Part A (hospital insurance) and Medicare Part B (medical insurance) if you are a United States citizen or a permanent legal resident who has lived in the U.S. for at least five years in a row.
How long do you have to work to pay Medicare?
You or your spouse worked long enough (40 quarters or 10 years) while paying Medicare taxes. You or your spouse had Medicare-covered government employment or retiree who has paid Medicare payroll taxes while working but has not paid into Social Security. Normally, you pay a monthly premium for Medicare Part B, no matter how many years you’ve worked.
What happens if you refuse Medicare Part B?
If you refuse it, you don’t lose your Medicare Part B eligibility. However, you may have to wait for a valid enrollment period before you can enroll . You may also have to pay a late enrollment penalty for as long as you have Medicare Part B coverage.
When do you get Medicare Part A and Part B?
If you meet Medicare eligibility requirements and you have received Social Security benefits for at least four months prior to turning age 65, you will typically get Medicare Part A and Part B automatically the first day of the month you turn age 65.
Is Medicare available to everyone?
Medicare coverage is not available to everyone. To receive benefits under this federal insurance program, you have to meet Medicare eligibility requirements. Find affordable Medicare plans in your area. Find Plans. Find Medicare plans in your area. Find Plans.
Who is Medicare eligible?
The simplest category of Medicare eligible individuals includes most senior citizens. Any individual 65 years of age or older who is a United States citizen and paid into the Medicare system through their payroll taxes is Medicare eligible. Married individuals who did not pay into the system through taxes are still eligible ...
How many seniors are eligible for Medicare?
The system provides insurance coverage to roughly 45 million Americans, 38 million of whom are senior citizens over the age of 65. Medicare eligibility is not restricted to senior citizens however; in fact not even all senior citizens are eligible for Medicare.
How long is the waiting period for Medicare?
Those who are receiving Social Security disability benefits due to an illness or disability are eligible to receive Medicare but there is a two year waiting period. The Medicare program provides eligible individuals with many benefits despite some drawbacks.
How many people are covered by Medicare?
The system provides insurance coverage to roughly 45 million Americans, 38 million of whom are senior citizens over the age of 65.
Who is eligible for Medicare if they are 65?
Individuals who are 65 years of age or older, but only paid into Medicare through taxes for less than 10 years, are still eligible for Medicare but must pay a monthly premium for Part A. Individuals in this group will pay less of a premium than those who never paid into the Medicare system. Certain groups of individuals born outside ...
Can illegal aliens collect Medicare?
No illegal aliens are allowed to collect Medicare benefits. Those who are legal aliens in the United States and have lived in the country for at least five years continuously may be Medicare eligible but need to contact a local Medicare office for specific eligibility information as it can vary from person to person.
Is there a waiting period for Medicare for ALS?
Also, individuals who are suffering from Lou Gehrig’s Disease (also known as ALS) are eligible for Medicare coverage. For these individuals, there is no waiting period;
How old do you have to be to get Medicare?
citizen or have been a legal resident for at least five years, you can get full Medicare benefits at age 65 or older. You just have to buy into them by: Paying premiums for Part A, the hospital insurance.
How long do you have to live to qualify for Medicare?
You qualify for full Medicare benefits if: You are a U.S. citizen or a permanent legal resident who has lived in the United States for at least five years and. You are receiving Social Security or railroad retirement benefits or have worked long enough to be eligible for those benefits but are not yet collecting them.
How much will Medicare premiums be in 2021?
If you have 30 to 39 credits, you pay less — $259 a month in 2021. If you continue working until you gain 40 credits, you will no longer pay these premiums. Paying the same monthly premiums for Part B, which covers doctor visits and other outpatient services, as other enrollees pay.
How long do you have to be on disability to receive Social Security?
You have been entitled to Social Security disability benefits for at least 24 months (that need not be consecutive); or. You receive a disability pension from the Railroad Retirement Board and meet certain conditions; or.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
When do you have to be on Medicare before you can get Medicare?
Individuals already receiving Social Security or RRB benefits at least 4 months before being eligible for Medicare and residing in the United States (except residents of Puerto Rico) are automatically enrolled in both premium-free Part A and Part B.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
What is the income related monthly adjustment amount for Medicare?
Individuals with income greater than $85,000 and married couples with income greater than $170,000 must pay a higher premium for Part B and an extra amount for Part D coverage in addition to their Part D plan premium. This additional amount is called income-related monthly adjustment amount. Less than 5 percent of people with Medicare are affected, so most people will not pay a higher premium.
How long does Medicare take to pay for disability?
A person who is entitled to monthly Social Security or Railroad Retirement Board (RRB) benefits on the basis of disability is automatically entitled to Part A after receiving disability benefits for 24 months.
What is MEC in Medicare?
Medicare and Minimum Essential Coverage (MEC) Medicare Part A counts as minimum essential coverage and satisfies the law that requires people to have health coverage. For additional information about minimum essential coverage (MEC) for people with Medicare, go to our Medicare & Marketplace page.
How long does Part A coverage last?
If the application is filed more than 6 months after turning age 65, Part A coverage will be retroactive for 6 months. NOTE: For an individual whose 65th birthday is on the first day of the month, Part A coverage begins on the first day of the month preceding their birth month.
What is Medicare a federal program?
Medicare is a federal healthcare program that Americans pay into with taxes. It makes sense that the government would want to make sure that you have ties to the country before they allowed you access to that benefit.
What happens if you don't sign up for Medicare?
If you do not sign up yourself, you will be automatically enrolled in Original Medicare and a Part D plan by the government. You will have the option to change to a MA-PD or pick a different Part D plan at a later time. What It Means to Be Dual Eligible for Medicare and Medicaid.
How long does a disability last?
You have a disability that is expected to last longer than 12 months. This disability can be for any number of reasons but must be approved for Social Security Disability Insurance (SSDI) to be eligible for Medicare. You cannot sign up for Medicare until you have been on SSDI for 24 months.
What is the second requirement for Medicare?
The second requirement for Medicare eligibility is to demonstrate medical need. Medicare leaves no room for interpretation here. You will be eligible for the program if you meet at least one of the following criteria.
Is Medicare and Medicaid the same?
Millions of Americans are eligible for both Medicare and Medicaid every year. This dual eligibility may provide extra coverage to beneficiaries but with that comes extra regulation. It is important to note that both programs are managed by the same federal agency, the Centers for Medicare and Medicaid Services (CMS).
Can you get Medicare if you have kidneys?
This does not mean your kidneys are just having a tough time. It means that your kidneys are functioning so poorly they require dialysis or a kidney transplant for you to stay alive. In order to be eligible for Medicare, you or your spouse must have also paid a certain amount of Social Security taxes into the system.
Can you sign up for Medicare Part D?
Although Part D plans are voluntary for most Medicare beneficiaries, those who are dual eligible have no choice. Medicaid requires that you sign up for Medicare as soon as you are eligible and this includes signing up for a Part D plan.
How old do you have to be to get Medicare?
To enroll in original Medicare (to be eligible for Part C), in general, you must qualify by: Age. You must be at least age 65 or older and a U.S. citizen or legal permanent resident for a minimum of 5 contiguous years. Disability.
When is Medicare open enrollment?
Finally, there’s also the Medicare Advantage open enrollment period. This is from January 1 to March 31 each year. However, this period only lets you make changes to your plan if you’re already enrolled in a Medicare Advantage plan.
What is Medicare Part C?
How Part C works. Takeaway. Medicare Part C, also called Medicare Advantage, is an insurance option for people who are eligible for Medicare. These plans are offered through private insurance companies. You don’t need to buy a Medicare Part C plan. It’s an alternative to original Medicare that offers additional items and services.
How old do you have to be to get Medicare?
People can enroll in Original Medicare if they are 65 years of age or older and are a citizen of the United States or have been a legal permanent resident for at least 5 years. Specific rules apply to those younger than 65 who have certain illnesses or disabilities. Read more about eligibility under the age of 65 here.
How long do you have to be a resident to qualify for Medicare?
They must also be a U.S. citizen or have been a legal permanent resident for at least 5 years.
What is Medicare Part C?
Medicare Part C, or Medicare Advantage, provides an alternative way for individuals with Medicare Parts A and B to receive their benefits. Medicare contracts private insurance companies to administer Medicare Part C plans.
What is a SNP plan?
Medicare has designed SNPs specifically for people who have particular health needs. The eligibility criteria for an SNP depends on the health conditions that the plan covers. SNP membership is available to individuals who: live in certain institutions, such as a nursing home.
What is the enrollment period for Medicare?
The Medicare initial enrollment period (IEP) begins from 3 months before a person turns 65 and lasts for 7 months. During this enrollment period, a person can enroll in: 1 Medicare Parts A and B 2 Medicare Part C (Medicare Advantage) 3 Medicare Part D
What is a medical savings account?
Medical Savings Accounts. A Medical Savings Account (MSA) plan allows the insured person to choose their healthcare services and providers. An MSA has two parts. The first part is a health plan that covers costs once the insured person has met a high yearly deductible. The second part is a Medical Savings Account.
When is the AEP for Medicare?
It is also called the annual enrollment period or Medicare open enrollment. The AEP dates run from October 15 through December 7.
What happens if you don't enroll in Medicare Part D?
If you don’t enroll when you’re first eligible and don’t have creditable coverage, you could face a late enrollment penalty. Let’s take a closer look at using an example. Tip: Medicare Plan D and Part D aren’t the same things.
Why is Medicare Part D important?
For many, prescription medications are vital to maintaining a healthy lifestyle. The costs of medications can drain finances, Medicare Part D prescription helps those who need assistance with medications .
How long do you have to change your plan if you are no longer eligible for Part D?
If you’re no longer eligible for Extra Help for the following year, you will have a 3-month window to change plans. This period starts either the date you’re notified or when you’re no longer eligible;
Is it necessary to take prescriptions on a regular basis?
For many seniors, taking prescription drugs on a regular basis is not optional. Patients who have regular medication needs should be sure to enroll as soon as Medicare Part D eligibility begins. Unexpected or not, the cost of medications can be financially exhausting, Part D plans provide you with a much lower cost for the same quality ...
Can Medicare delay Part D?
Delaying Part D When Eligible. Medicare may add a Part D Late Enrollment Penalty to your Part D premium each month you have Part D coverage. Unless you enroll in a Part D plan when you’re first eligible during your IEP. As we grow older our chances of needing prescriptions will often increase. If you have no creditable prescription drug coverage, ...
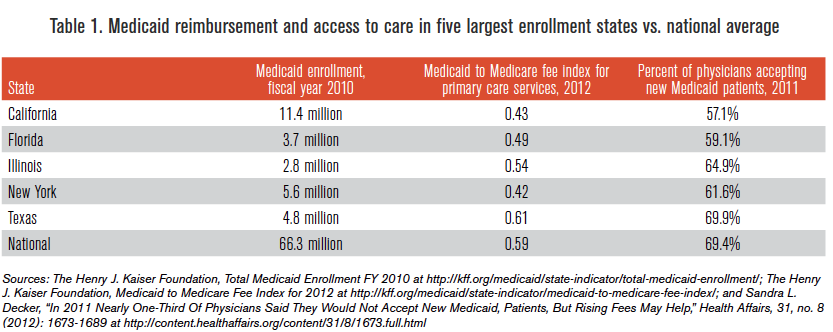
Is Medicaid a federal or state program?
Medicaid is another Federal and State government medical health insurance program. Medicaid provides coverage for individuals and families that have low incomes or limited resources. Not all will qualify for Medicaid coverage in addition to Medicare coverage. Medicare beneficiaries with full Medicaid benefits are dually eligible.
Do I need a Medicare Advantage plan if I have supplemental insurance?
But if you have a Medicare Advantage plan that includes Part D, you can’t have a separate Part D plan.