If you are age 65 or older, you are generally eligible to receive Medicare Part A (hospital insurance) and Medicare Part B (medical insurance) if you are a United States citizen or a permanent legal resident who has lived in the U.S. for at least five years in a row. Younger than age 65: who is eligible for Medicare?
Full Answer
Who is eligible for the peehip Supplemental Medical Plan?
peehip. Get Ready for Your New Medicare Card Personal identity theft affects a large and growing number of seniors. People over age 65 are increasingly victims of this type of crime. This is why the Centers for Medicare & Medicaid Services (CMS) will be removing Social Security Numbers from Medicare cards. This change will mean that all people
Who is eligible for Medicare?
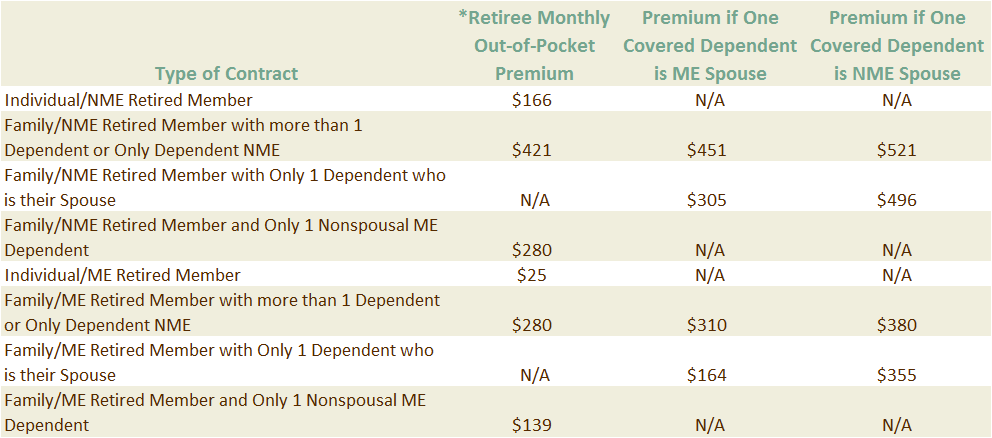
A PEEHIP member who has a combined household income of 300% or less of that level may qualify for a reduced premium on his or her hospital medical premium. The discount can reduce the member's premium contribution by 10, 20, 30, 40 or 50% depending on the member's household income and family size.
Does my peehip plan include Medicare Part C and D?
include Medicare plans in the new at-home test requirements. However, members in the PEEHIP Humana Group Medicare Advantage Plan can still use the USPS link to order four free at-home tests per household. If you have any questions, contact PEEHIP at 877.517.0020.
How does peehip work with Medicare Advantage?
The following members enrolled in the PEEHIP Hospital Medical (Group # 14000) plan are required to complete all required activities in order to obtain their $50 monthly wellness premium waiver: ♦ Active Employees ♦ Non-Medicare-eligible retirees ♦ All covered spouses of active employees and non-Medicare-eligible spouses of retirees
How long can you get a prescription for Peehip?
1. Am I able to receive a 90-day supply of my medication? Yes, your pharmacy benefit allows you to obtain a 90-day supply of a medication at a retail pharmacy that is on the PEEHIP Maintenance Drug List. However, if you are obtaining your maintenance medication for the first time, your first prescription will be limited to a 30-day supply. After your first fill, you can receive quantities up to, but not more than, a 90-day supply as long as the prescription is written for 90 days and no more than 130 days have lapsed between medication fills. Prior Authorization may be required for certain drugs. Due to an error, you may have had a problem in obtaining a 90-day supply. This error has been fixed. If this happened to you, please contact your pharmacist to tell them you want a 90-day supply on your next fill. To determine if your medication is on the Maintenance Drug List and any other questions, you can contact UnitedHealthcare Customer Service at 877.298.2341, TTY 711 or go online to www.UHCRetiree.com/peehip.
Does Medicare provide PEEHIP?
hospital medical and prescription drug coverage for Medicare-eligible PEEHIP retirees is now provided by the UnitedHealthcare® Group Medicare Advantage PPO plan. In previous PEEHIP Advisors, which can be found at
What is Peehip insurance?
PEEHIP offers the Cancer, Dental, Hospital Indemnity, and Vision plans. Claims administration is provided through Southland Benefit Solutions. Once enrolled, these plans must be retained for the entire insurance year, i.e. until September 30.
How to add dependent to Peehip?
Go to Member Online Services. Once you log in, click the “Enroll or Change PEEHIP Coverage” link, then select the Qualifying Life Event (QLE) option.
How to get your PID mailed?
You can request to have your PID mailed to you by clicking here. Once you receive your PID letter, you can revisit Member Online Services to register your account.
How long does it take to add a new baby to my PEEHIP?
You can add your new baby, adopted child, or new spouse as a dependent on your insurance coverage but it must be done within 45 days of the applicable Qualifying Life Event (QLE), unless the change is made during PEEHIP's Open Enrollment for an October 1 effective date. There are two options to add your new dependent:
How to change name on Peehip?
Submit a copy of your corrected Social Security card showing your new name to PEEHIP. You must also contact the insurance clerk or payroll officer at your employer so that they can change your name on your Retirement Contribution Report. Once your name is changed in PEEHIP's system, the insurance carriers will issue new insurance cards with your new name. Name changes cannot be made online through the Member Online Services.
What are qualifying life events?
There are certain qualifying life events (QLE) that can occur outside of the set annual Open Enrollment period that might require changes to your MEDICAL coverage. Examples of QLEs to add a person would be the birth or adoption of a child, marriage, loss of a dependent’s employer coverage for certain reasons. Examples of QLEs to remove someone from your Medical coverage outside of Open Enrollment include death of a dependent, divorce, a dependent’s employment with a group health plan. YOU MUST NOTIFY PEEHIP WITHIN 45 DAYS OF THE QLE! The change can be made with the New Enrollment and Status Change form or (for certain types of QLES) the change can be made online through Member Online Services (MOS).
What is a Peehip claim hold?
Your PEEHIP account may be on “claim hold.” PEEHIP accounts are placed in “claim hold” status when a premium is past due or when certain required documents have not been received after several request.
How old do you have to be to get Medicare?
If you are age 65 or older, you are generally eligible to receive Medicare Part A (hospital insurance) and Medicare Part B (medical insurance) if you are a United States citizen or a permanent legal resident who has lived in the U.S. for at least five years in a row.
When do you get Medicare Part A and Part B?
If you meet Medicare eligibility requirements and you have received Social Security benefits for at least four months prior to turning age 65, you will typically get Medicare Part A and Part B automatically the first day of the month you turn age 65.
What happens if you refuse Medicare Part B?
If you refuse it, you don’t lose your Medicare Part B eligibility. However, you may have to wait for a valid enrollment period before you can enroll . You may also have to pay a late enrollment penalty for as long as you have Medicare Part B coverage.
How long do you have to work to pay Medicare?
You or your spouse worked long enough (40 quarters or 10 years) while paying Medicare taxes. You or your spouse had Medicare-covered government employment or retiree who has paid Medicare payroll taxes while working but has not paid into Social Security. Normally, you pay a monthly premium for Medicare Part B, no matter how many years you’ve worked.
Is Medicare available to everyone?
Medicare coverage is not available to everyone. To receive benefits under this federal insurance program, you have to meet Medicare eligibility requirements. Find affordable Medicare plans in your area. Find Plans. Find Medicare plans in your area. Find Plans.
Do you pay Medicare Part B monthly?
Normally, you pay a monthly premium for Medicare Part B, no matter how many years you’ve worked. Read more about the Part A and Part B premiums.
