Medicaid waivers are for people with disabilities and chronic health conditions. The waivers allow healthcare professionals to provide care in a person’s home or community instead of a long-term care facility. Medicare is a federal program. To be eligible for Medicare, a person must be age 65 years or above.
What are Medicaid waivers and who qualifies?
Medicaid waivers are for people with disabilities and chronic health conditions. The waivers allow healthcare professionals to provide care in a person’s home or community instead of a long-term care facility.
Who is eligible for Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
What is a Medicare waiver for home care?
The waivers allow healthcare professionals to provide care in a person’s home or community instead of a long-term care facility. Medicare is a federal program. To be eligible for Medicare, a person must be age 65 years or above.
Who is eligible for an HCBS waiver?
Generally, states offer HCBS waivers to elderly people (aged 65 or over), physically disabled people, adults and children with developmental disabilities, and medically fragile people (who require life support or other extensive medical equipment).

Who qualifies for a Medi-Cal waiver?
To Access Medi-Cal Waiver Services For disabled individuals requiring Home and Community-Based Services, there may be services available for such target populations as the elderly, developmentally disabled, or Medi-Cal beneficiaries with mid- to late- stage AIDS, or who require assisted living.
What is a Medi-Cal waiver?
Home and Community-Based Services (HCBS) Waivers allow states that participate in Medicaid, known as Medi-Cal in California, to develop creative alternatives for individuals who would otherwise require care in a nursing facility or hospital.
What is Arkansas Medicaid waiver?
The DDS Alternative Community Services (ACS) Waiver assists persons with disabilities in Arkansas. The ACS Waiver serves individuals with ID/DD of any age who meets institutional level of care eligibility, financial eligibility, and who has an opening (slot) in the program.
What is the PA Aging waiver Program?
The Pennsylvania Department of Aging (PDA) Medicaid Waiver provides home and community based services (HCBS) to seniors who require nursing facility care, but elect to live and receive care in their own homes or in other community living arrangements, such as a Domiciliary Care Home.
What is the Medi-Cal 2020 waiver?
Medi-Cal 2020 is a five year renewal of California's Section 1115 Medicaid Waiver, which could provide California with more than $7.1 billion in federal funding through programs that shift the focus away from hospital-based and inpatient care, towards outpatient, primary and preventive care – in other words, from ...
What is IHO waiver?
The IHO Waiver provides services to either 1) Medi-Cal beneficiaries who have been continuously enrolled in an In Home Operations administered waiver since prior to January 1, 2002 and require direct care services provided primarily by a licensed nurse; or 2) those who have been receiving continuous care in a hospital ...
What is Arkansas Waiver Program?
AR Autism Waiver (0936. Provides consultative clinical and therapeutic services, individual assessment/treatment development/monitoring, lead therapy intervention, line therapy intervention, and therapeutic aides and behavioral reinforcers for children with autism ages 1-7 years.
Who qualifies for home health in Arkansas?
To be eligible for AR Choices, an applicant must be a resident of Arkansas who is physically disabled between the ages of 21 and 64, or is 65 years of age or older. In addition, functional and financial requirements must be met.
What is CES waiver in Arkansas?
The Community and Employment Support (CES) Waiver offers services in your community to support clients with intellectual or developmental disabilities (IDD) with all major life activities, such as living independently and working at a job with help from an employment coach.
How do I get a waiver service in PA?
Call the PA Independent Enrollment Broker (PA IEB) at 1-877-550-4227.Eligibility Determination.Determination within 86 days of the first in-home visit.STEP 2 Have your first in-home visit.Have your second in-home visit.The CAO reviews your waiver application and makes a decision.More items...
Does PA Medicaid pay for in home care?
Pennsylvania's Medicaid program will pay for a nursing home or home care if you have limited income and assets and your doctor certifies that you need the care. Nursing homes and assisted living facilities in Pennsylvania are expensive, and even alternative long-term care like home health care can be costly.
What is the Commcare waiver in PA?
COMMCARE Waiver: Home and community-based program developed for individuals who experience a medically determinable diagnosis of traumatic brain injury.
What is Medicaid waiver?
The Medicaid waiver program allows states to choose groups of people with particular needs and health conditions to receive tailor-made healthcare options at home or within the community. For example, some states provide waivers for care relating to developmental disabilities, traumatic brain injuries, AIDS, and substance use disorders.
What is a waiver program?
uses an individualized plan of care centered on the person. A waiver program allows the state to waive some requirements to meet the needs of individuals.
What is the program of all inclusive care for the elderly?
The Program of All-Inclusive Care for the Elderly (PACE) is a joint Medicaid and Medicare program designed to help meet a person’s healthcare needs in the community. The program uses a team of healthcare providers to coordinate and deliver care. A person can have Medicare, Medicaid, or both ...
What is HCBS waiver?
For example, a waiver may help a person with an increased likelihood of requiring long-term care, such as those with behavioral issues or technologically dependent children. Under the HCBS program, states can also offer a variety of non-medical services, including: case management. homemaker services.
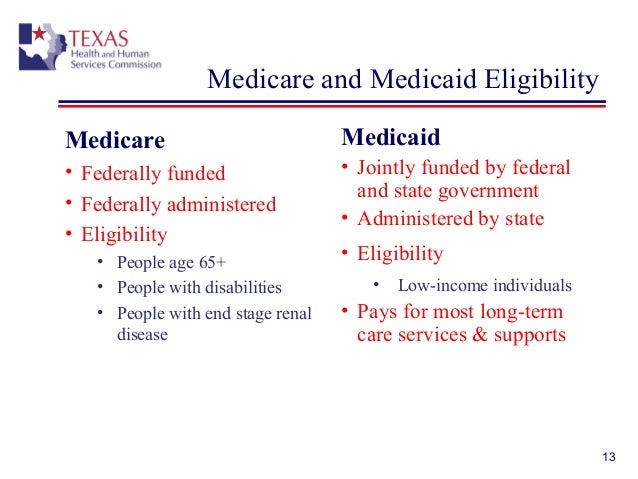
How old do you have to be to get medicare?
Medicare is a federal program. To be eligible for Medicare, a person must be age 65 years or above. People younger than age 65 years may also be eligible, but only if they have specific health conditions. Medicaid is a joint federal and state program providing health benefits for those who meet the eligibility requirements.
How old do you have to be to be eligible for a PACE?
A person can have Medicare, Medicaid, or both to be eligible for PACE. They must also: be 55 years of age or older. live in a PACE service area. require a nursing home level of care. be able to live safely in the community with assistance.
Is Medicaid a federal or state program?
Medicaid is a joint federal and state program . Medicaid waiver programs help people who qualify for inpatient care to receive healthcare services at home. Each state can develop its own waiver programs, so some rules and eligibility criteria may vary. However, some rules are the same in each state.
Is Medicare being waived in Maryland?
Federal Medicare rules are being waived. Instead of following federal Medicare rules for payment, hospitals in Maryland follow Maryland-specific rules. Maryland is the only U.S. state with a Medicare waiver .
Is Medicare paid by the federal government in Maryland?
Because of the waiver, hospital services rendered to Medicare patients in Maryland are paid by the federal government at a higher rate than would be the case without the waiver.
Does Medicare waiver affect only Medicare patients?
Does the Medicare waiver affect only Medicare patients? The Medicare waiver affects all patients, regardless of age or Medicare eligibility, treated in Maryland hospitals. Under its rules, every payer—whether an individual, Medicare, Medicaid or a private insurer—pays the same charge for the same care.
What is Medicaid waiver?
A Medicaid waiver is a provision in Medicaid law which allows the federal government to waive rules that usually apply to the Medicaid program. The intention is to allow individual states to accomplish certain goals, such as reducing costs, expanding coverage, or improving care for certain target groups such as the elderly or women who are pregnant.
What are the benefits of Medicaid waivers?
Benefits of Medicaid Waivers. For those who are a part of an HBCS program, the biggest benefit is they get to stay in their own home or community, instead of being sent to a care institution. Staying at home has been shown to have many quality of life benefits, especially for seniors who get to age in place.
What is the purpose of HCBS waiver?
As outlined above, the purpose of an HCBS waiver is to let states provide care to certain individuals in the community, rather than putting them into institutional care. Beneficiaries may live in their own home, at a relative’s home, or in a senior living community that isn’t a nursing home.
What is Medicaid Home and Community Based Services?
One such program is Medicaid Home and Community Based Services – a Medicaid waiver that helps people stay in their home instead of receiving care in a nursing home or other institution.
What are the requirements for HCBS?
Those who are accepted into their state’s HCBS waiver program will receive a range of medical and non-medical care, which can vary depending on the individual’s needs and situation, as well as state guidelines. This may include: 1 Personal care services and supervision, at home or in an assisted living facility 2 A home health aide 3 Nursing 4 Medical supplies and medical equipment 5 Chore and homemaking services, such as shopping, laundry, and cleaning 6 Hot meal delivery services 7 Respite care to relieve a primary caregiver 8 Counseling services 9 Home and/or vehicle modifications, such as ramps and safety rails, to increase independence 10 Support and case management 11 Assistance transitioning from a nursing home into the community 12 Access to senior centers or adult group day care 13 Transport to and from non-emergency medical appointments 14 Non-medical transportation services 15 Personal emergency response systems
What is the difference between Medicare and Medicaid?
Medicare is a federal program that provides health care to all individuals over the age of 65 as well as people with disabilities under the age of 65. Medicaid, on the other hand, is for people with very limited resources and income. Because Medicaid is run by each individual state, the specific eligibility requirements ...
What is freedom of choice waiver?
Section 1915 (b) waivers – “Freedom of choice waivers” allow states to provide care via managed care delivery systems. These organizations contract with state Medicaid agencies, and are paid from the state Medicaid fund for providing health care services to the beneficiaries, thus limiting the individual’s ability to choose their own providers.
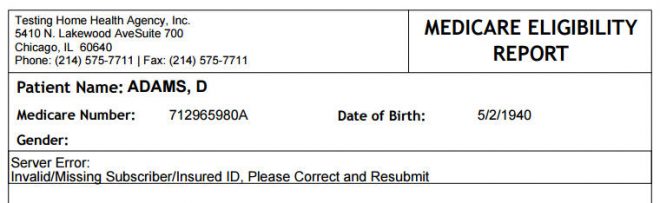
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
When are Medicare premiums due?
Pay on time to avoid coverage cancellation. Medicare premiums are due the 25th day of the month. Don’t miss more than 3 consecutive months of payments to Medicare. Coverage will end in the fourth month if payments aren’t made.
What percentage of FPL can I get for Medicare Part B?
Not have an income that is more than 200% of the FPL (You may only get partial aid if your income is between 150% to 200% of the FPL.) Part B Only: Both the Specified Low-Income Medicare Beneficiary (SLMB) and Qualifying Individual (QI) programs will help pay for Medicare Part B premiums.
What is the difference between Medicare Part A and Part B?
All programs require eligibility for Medicare Part A, but the main difference between each is the federal poverty level (FPL) range that those seeking help must be within.
How much does Medicare Part D cost?
Medicare Part D plans are also provided through private insurance companies. The national average Part D premium is $33.19, according to My Medicare Matters. But depending on where you live and the type of plan you have, Medicare Part D costs will vary.
Is QMB coverage 100%?
But if you’re approved as a QMB, you are not responsible for paying any cost-sharing, according to the Center for Medicare Advocacy. This means that your Medicare costs, including your premiums, are 100% covered. To qualify for the QMB program, your income must not exceed 100% of the FPL.
Can you get Medicare out of pocket?
Each state manages MSP funds and decides who qualifies. Programs can pay for all, or just some, of your Medicare out-of-pocket expenses, which includes premiums.
Which states have different income limits?
Alaska and Hawaii are the only two states that have different income limits. Three of the four MSPs have the same resources limits, and these limits are the same for all states, including Alaska and Hawaii. If you earn equal to or less than these limits, then you may qualify for assistance. Program Name.
What is dual eligible for Medicare?
Eligibility for the Medicare Savings Programs, through which Medicaid pays Medicare premiums, deductibles, and/or coinsurance costs for beneficiaries eligible for both programs (often referred to as dual eligibles) is determined using SSI methodologies..
How many people are covered by medicaid?
Medicaid is a joint federal and state program that, together with the Children’s Health Insurance Program (CHIP), provides health coverage to over 72.5 million Americans, including children, pregnant women, parents, seniors, and individuals with disabilities. Medicaid is the single largest source of health coverage in the United States.
What is Medicaid Spousal Impoverishment?
Spousal Impoverishment : Protects the spouse of a Medicaid applicant or beneficiary who needs coverage for long-term services and supports (LTSS), in either an institution or a home or other community-based setting, from becoming impoverished in order for the spouse in need of LTSS to attain Medicaid coverage for such services.
What is MAGI for Medicaid?
MAGI is the basis for determining Medicaid income eligibility for most children, pregnant women, parents, and adults. The MAGI-based methodology considers taxable income and tax filing relationships to determine financial eligibility for Medicaid. MAGI replaced the former process for calculating Medicaid eligibility, ...
What is Medicaid coverage?
Medicaid is the single largest source of health coverage in the United States. To participate in Medicaid, federal law requires states to cover certain groups of individuals. Low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI) are examples of mandatory eligibility groups (PDF, ...
How long does medicaid last?
Benefits also may be covered retroactively for up to three months prior to the month of application, if the individual would have been eligible during that period had he or she applied. Coverage generally stops at the end of the month in which a person no longer meets the requirements for eligibility.
Does Medicaid require income?
Certain Medicaid eligibility groups do not require a determination of income by the Medicaid agency. This coverage may be based on enrollment in another program, such as SSI or the breast and cervical cancer treatment and prevention program.
What is a CCC Plus Medicaid waiver?
The CCC Plus Medicaid Waiver is not an entitlement program, which means meeting eligibility requirements does not equate to immediate receipt of program benefits.
How much can a spouse keep on Medicaid?
In this case, the applicant spouse can retain up to $2,000 in assets and the non-applicant spouse can keep up to $130,380. This larger allocation of assets to the non-applicant spouse is called a community spouse resource allowance. Some assets are not counted towards Medicaid’s asset limit.
How long does it take for a medicaid application to be approved?
In most cases, it takes between 45 and 90 days for the Medicaid agency to review and approve or deny one’s application. Based on law, Medicaid offices have up to 45 days to complete this process (up to 90 days for disability applications). Despite the law, applications are sometimes delayed even further.
How long does it take to get medicaid?
The Medicaid application process can take up to 3 months, or even longer, from the beginning of the application process through the receipt of the determination letter indicating approval or denial. Generally, it takes one several weeks to complete the application and gather all of the supportive documentation. If the application is not properly completed, or required documentation is missing, the application process will be delayed even further. In most cases, it takes between 45 and 90 days for the Medicaid agency to review and approve or deny one’s application. Based on law, Medicaid offices have up to 45 days to complete this process (up to 90 days for disability applications). Despite the law, applications are sometimes delayed even further. Additionally, as wait-lists may exist, approved applicants may spend many months waiting to receive benefits.
Can you enroll in CCC+ with both Medicare and Medicaid?
There are several managed care plans from which to choose. Persons who are “dual eligible” can enroll in CCC+, but will receive their Medicaid and Medicare benefits separately. The term, “ dual eligible ”, is used for persons who are eligible for both Medicaid and Medicare.
Does Virginia have medicaid?
Virginia has a Medically Needy Medicaid Program for applicants who have high medical expenses relative to their income. Also known as a “spend down” program, applicants are permitted to spend “excess” income on medical expenses and health care premiums, such as Medicare Part B, in order to meet Medicaid’s income limit.
Does Medicaid have a 60 month look back rule?
Unfortunately, some planning strategies violate Medicaid’s 60-month look back rule and should be implemented well in advance of the need for long-term care. However, there are some workarounds, such as the Modern Half a Loaf, and Medicaid planners are aware of them.