The following insurance carriers are some who offer Medicare Advantage plans in Illinois for 2022: Aetna Medicare Ascension Complete Blue Cross and Blue Shield of Illinois
Full Answer
How do you contact Illinois Medicaid?
- Medicaid Office Location
- Illinois Department of Healthcare and Family Services 201 South Grand Avenue East Springfield, IL 62763
- Medicaid Office Phone Number
- The phone number to call the Illinois Medicaid office is 800-843-6154 or call 800-226-0768.
- Medicaid Online
- To view the website for Illinois Medicaid online, click here.
What is the phone number for Medicare in Illinois?
Phone 1-800-MEDICARE (1-800-633-4227) For specific billing questions and questions about your claims, medical records, or expenses, log into your secure Medicare account, or call us at 1-800-MEDICARE.. If you want Medicare to be able to give your personal information to someone other than you, you need to fill out an "Authorization to Disclose Personal Health Information."
What is the toll - free number for Illinois Medicaid?
We suggest contacting the Medicaid office to find out specifically what coverage is provided as it can be different in each state. The phone number to call the Illinois Medicaid office is 800-843-6154 or call 800-226-0768. To view the website for Illinois Medicaid online, click here.
What is the Medicare age for Illinois?
You may be eligible for Medicare in Illinois if you’re a U.S. citizen or a permanent legal resident who has lived in the U.S. for more than five years and one or more of the following applies to you: 3 You are age 65 or older. You are under 65, disabled, and receive disability benefits from Social Security or the Railroad Retirement Board.

Who administers Medicare in Illinois?
the Centers for Medicare and Medicaid ServicesThe Medicare Program is administered by the Centers for Medicare and Medicaid Services (also known as the federal CMS). Medicare has the following parts: F Part A is insurance that helps pay for inpatient hospital facility charges, skilled nursing facility charges, hospice care and some home healthcare services.
What is Medicare called in Illinois?
Some Illinois seniors purchase a Medicare Supplement Insurance policy, also known as Medigap.
What is Illinois Medicaid program called?
HealthChoice IllinoisHealthChoice Illinois is the statewide Medicaid managed care program. Most Medicaid customers are required to choose a primary care provider (PCP) and health plan. We can help you understand your plan choices, find providers and enroll.
How do I find a Medicaid provider in Illinois?
You can easily do this by using the state's Medicaid lookup tool, visiting insurers' websites, using doctor lookup tools or contacting providers directly. Once you've found an Illinois provider, be sure to have your Medicaid card handy.
How do I contact Medicare in Illinois?
1-800-MEDICARE (1-800-633-4227)
How do I choose a Medicare plan in Illinois?
To find the plan that best suits your needs, consider these factors:Covered services. Medicare Advantage plans may cover services that original Medicare doesn't, such as dental, vision, or hearing care. ... Cost. The cost of Medicare Advantage plans varies. ... Provider network. ... Service area. ... Ratings.
Who is in charge of Medicaid in Illinois?
Theresa Eagleson, Director Theresa Eagleson has served as Director of the Department of Healthcare and Family Services since January 2019. Immediately prior to her appointment by Governor Pritzker, she was the Executive Director of the Office of Medicaid Innovation at the University of Illinois for four years.
What is the difference between Medicare and Medicaid?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
What is Illinois State insurance called?
Illinois Comprehensive Health Insurance Plan (CHIP) - A State health insurance program for Illinois residents that are considered high risk.
Is IlliniCare Medicaid?
CHICAGO — Aetna Better Health, a CVS Health company, today announced IlliniCare Health, a Medicaid managed care plan that serves members across Illinois, has officially rebranded and changed its name to Aetna Better Health of Illinois (ABH-IL).
How do I contact Illinois Medicaid?
To get more information on applying for Medicaid, please contact the Health Benefits Hotline at 1-800-843-6154. TTY users can call 855-889-4326.
What is health Choice Illinois?
HealthChoice Illinois is a mandatory program for seniors and physically disabled persons who are Medicaid and Medicare eligible (dual eligible), reside in a nursing home or receive long-term home and community based services, and are not enrolled in the IL Medicare-Medicaid Alignment Initiative Program.
SPOTLIGHT & RELEASES
09/15/2021 : CMS released the Second Evaluation Report and associated Findings At-a-Glance for the Illinois capitated model demonstration under the Medicare-Medicaid Financial Alignment Initiative
Key Dates
September 14, 2016 - CMS, Illinois, & participating plans execute an updated three-way contract
MMAI Model
On February 22, 2013, the Department of Health and Human Services announced that the State of Illinois will partner with the Centers for Medicare & Medicaid Services (CMS) to test a new model for providing Medicare-Medicaid enrollees with a more coordinated, person-centered care experience.
What is Medicare in Illinois?
Plan options. Enrollment. Resources. Takeaway. Medicare is a federal health insurance program that helps people age 65 and older pay for necessary medical care. You may also be eligible if you are younger than age 65 and living with certain disabilities.
How many Medicare Advantage plans are there in Illinois?
There are 147 Medicare Advantage plans available in Illinois for 2021, compared to 126 plans in 2020. All Illinois residents with Medicare have access to buy a Medicare Advantage plan, including plans with $0 premiums. There are 31 stand-alone Medicare Part D plans available in Illinois for 2021, compared to 28 plans in 2020.
How many people in Illinois are on Medicare in 2020?
The takeaway. Over 2.2 million people in Illinois were enrolled in Medicare in 2020. There are several private insurance companies offering many types of Medicare Advantage and Medigap plans in Illinois. Overall, Medicare Advantage plan monthly premium costs have decreased in Illinois for 2021.
How many Medicare plans are there in Illinois in 2021?
There are 31 stand-alone Medicare Part D plans available in Illinois for 2021, compared to 28 plans in 2020. All Illinois residents with a stand-alone Part D plan have access to a plan with a lower monthly premium than they paid in 2020. There are 12 different Medigap plans offered in Illinois for 2021.
What is the difference between Medicare Advantage and Original?
Original Medicare provides nationwide coverage, while Medicare Advantage plans serve more limited areas. If you plan to travel, you may prefer a Medicare plan that offers travel or visitor benefits. Ratings. Every year, the Centers for Medicare & Medicaid Services (CMS) rates plans from one to five stars.
What are the benefits of Medicare Advantage in Illinois?
Medicare Advantage plans in Illinois may offer many other benefits that aren’t included in original Medicare, such as: hearing, vision, and dental care. prescription drug coverage. wellness programs.
How long do you have to be on Medicare to receive SSDI?
If you’re eligible for Medicare due to a disability, you’ll be enrolled after you receive SSDI checks for 24 months. If you get Railroad Retirement benefits or Social Security retirement benefits, you’ll be enrolled when you turn 65 years old.
What age does Medicare cover?
Medicare is a federal health insurance program for individuals age 65 and older, individuals under age 65 with certain disabilities and individuals of any age with End-Stage Renal Disease (ESRD).
What is Medicare crossover?
Medicare Crossover is an electronic transmittal of claim data from Medicare (after Medicare has processed their portion of the claim) to the QCHP plan administrator for secondary benefit determination.
How old do you have to be to get Medicare Part A?
Eligibility for premium-free Medicare Part A occurs when an individual is age 65 or older and has earned at least 40 work credits from paying into Medicare through Social Security. An individual who is not eligible for premium-free Medicare Part A benefits based on his/her own work credits may qualify for premium-free Medicare Part A benefits based on the work history of a current, former or deceased spouse. All plan participants that are determined to be ineligible for Medicare Part A based on their own work history are required to apply for premium-free Medicare Part A on the basis of a spouse (when applicable).
Can a provider opt out of Medicare?
Some healthcare providers choose to opt-out of the Medicare program. When a plan participant has medical services rendered by a provider who has opted-out of the Medicare program, a private contract is usually signed explaining that the planparticipant is responsible for the cost of the medical services rendered. Neither providers nor plan participants are allowed to bill Medicare. Therefore, Medicare will not pay for the service (even if it would normally qualify as being Medicare eligible) or provide a Medicare Summary Notice to the plan participant. If the service(s) would have normally been covered by Medicare, the plan administrator will estimate the portion of the claim that Medicare would have paid. The plan administrator will then subtract that amount from the total charge and adjudicate the claim for an eligible secondary reimbursement amount is the member's responsibility.
What is HealthChoice Illinois managed care?
HealthChoice Illinois is the state’s rebooted managed care program that began rolling out in January 1, 2018. The program provides enhanced quality and improved outcomes, with special upgrades designed to help providers.
Who is eligible and who is not included in HealthChoice Illinois managed care?
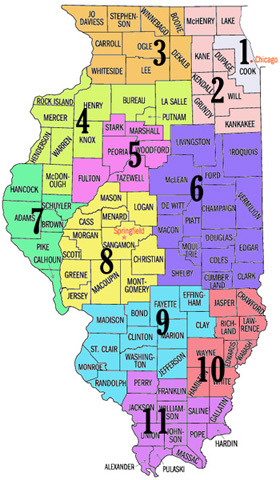
Medicaid members who previously participated in the mandatory managed care program are included in the new HealthChoice Illinois, in addition to special needs children, children receiving SSI, children in the Medically Fragile Technology Dependent waiver, and DCFS youth. HealthChoice Illinois also expanded managed care to every county in Illinois.
How do I become a participating provider and contract with the managed care plans?
New providers should credential through IMPACT. Providers will also need to contract with each plan individually by contacting the plans’ provider services.
Who do I contact for billing questions?
Billing questions should be directed toward the plan that the member is enrolled with.
How do I check eligibility for a client and what plan is my patient enrolled in?
Providers should check eligibility by utilizing the Medical Electronic Data Interchange (MEDI).
What about youth in DCFS care?
Managed care is to be provided by IlliniCare Health to youth in DCFS care starting in 2018.
What if a member is transitioning between different managed care organizations (MCOs) or between managed care and FFS (fee for service), whether due to eligibility changes or a change in MCO enrollment and is in the middle of a treatment?
Health plans must offer an initial 90–day transition period for members new to the plan, in which members may maintain a current course of treatment with a provider who is currently not a part of the plan’s network. The 90–day transition period is applicable to all providers, including Behavioral Health Providers and Providers of LTSS.
Provider Types, Specialties & Subspecialties
The table of IMPACT Provider Types, Specialties and Subspecialties is a reference guide that provides important information for providers enrolling or revalidating via IMPACT – both for providers that only deliver services through the HFS Medical Programs, as well as waiver program providers that deliver services for one or more other funding agencies (DHS, DCFS, IDoA, DSCC)..
IMPACT TAB
Locate your provider type for the services you provide. You can enroll as two different provider types, as long as they have the same enrollment type.
Add your favorite providers
Keep a list of all your favorite providers – Select the button above to find and compare providers. Then, select the heart icon next to any of the providers to add them to your list of favorites.
Not sure what type of provider you need?
Use our provider search tool to find quality data, services offered, and other information for these type of providers:
How to become a Medicare provider?
Become a Medicare Provider or Supplier 1 You’re a DMEPOS supplier. DMEPOS suppliers should follow the instructions on the Enroll as a DMEPOS Supplier page. 2 You’re an institutional provider. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should use the Medicare Enrollment Guide for Institutional Providers.
How to get an NPI?
If you already have an NPI, skip this step and proceed to Step 2. NPIs are issued through the National Plan & Provider Enumeration System (NPPES). You can apply for an NPI on the NPPES website.
How long does it take to change your Medicare billing?
To avoid having your Medicare billing privileges revoked, be sure to report the following changes within 30 days: a change in ownership. an adverse legal action. a change in practice location. You must report all other changes within 90 days. If you applied online, you can keep your information up to date in PECOS.
Do you need to be accredited to participate in CMS surveys?
ii If your institution has obtained accreditation from a CMS-approved accreditation organization, you will not need to participate in State Survey Agency surveys. You must inform the State Survey Agency that your institution is accredited. Accreditation is voluntary; CMS doesn’t require it for Medicare enrollment.
Can you bill Medicare for your services?
You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify. You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.