
What items are not covered by Medicaid?
Some of the items and services that Medicaid does not cover include: Services that have been deemed by the peer review organization, DHS, Dental, or Optometric specialist not to be clinically essential. Services that are provided by direct relatives or members of the beneficiary’s home. Home remedies, nutritional supplements, vitamins ...
What medications are not covered by Part D?
Usually, Part D plans do not cover drugs for weight management, erectile dysfunction, or fertility. Part D plans cover two drugs in the most commonly prescribed categories. However, different...
What items are covered by Medicare?
- Durable medical equipment (DME)
- Prosthetic devices
- Leg, arm, back and neck braces (orthoses) and artificial leg, arm and eyes, including replacement (prostheses)
- Home dialysis supplies and equipment
- Surgical dressings
- Immunosuppressive drugs
- Erythropoietin (EPO) for home dialysis patients
- Therapeutic shoes for diabetics
- Oral anticancer drugs
What does Medicare no pay mean?
- You are 65 or older and meet the citizenship or residency requirements.
- You are under age 65, disabled, and your premium-free Medicare Part A coverage ended because you returned to work.
- You have not paid Medicare taxes through your employment or have not worked the required time to qualify for premium-free Part A.
Does everyone on Medicare have Part A?
coverage if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A." Most people get premium-free Part A. The health care items or services covered under a health insurance plan.
Can you be denied coverage of Medicare Part A?
Generally, if you're eligible for Original Medicare (Part A and Part B), you can't be denied enrollment into a Medicare Advantage plan. If a Medicare Advantage plan gave you prior approval for a medical service, it can't deny you coverage later due to lack of medical necessity.
Why would a person not have Part A Medicare?
Unless they meet other requirements, such as a qualifying disability, they cannot get Medicare Part A benefits before this age. Some people may be 65 but ineligible for premium-free Medicare Part A. For instance, a person who did not work for 40 quarters and pay Medicare taxes would not be eligible.
Who applies for Medicare Part A?
age 65 or olderYou are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and paid Medicare taxes for at least 10 years. You can get Part A at age 65 without having to pay premiums if: You are receiving retirement benefits from Social Security or the Railroad Retirement Board.
Which of the following is excluded from Medicare coverage?
Non-medical services, including a private hospital room, hospital television and telephone, canceled or missed appointments, and copies of x-rays. Most non-emergency transportation, including ambulette services. Certain preventive services, including routine foot care.
Which of the following is not covered with Medicare Part A quizlet?
Medicare Part A covers 80% of the cost of durable medical equipment such as wheelchairs and hospital beds. The following are specifically excluded: private duty nursing, non-medical services, intermediate care, custodial care, and the first three pints of blood.
Who has to pay Medicare Part A premiums?
The takeaway Most people receive Medicare Part A automatically when they turn age 65 and pay no monthly premiums. If you or your spouse haven't worked at least 40 quarters, you'll pay a monthly premium for Part A.
Does everyone have to pay for Medicare?
A: Most Medicare-eligible people do not have to pay premiums for Medicare Part A. If you are 65 and you or your spouse has paid Medicare taxes for at least 10 years, you don't pay a premium for Part A.
Is Medicare Part A free for everyone?
Medicare Part A (Hospital Insurance) Most people get Part A for free, but some have to pay a premium for this coverage. To be eligible for premium-free Part A, an individual must be entitled to receive Medicare based on their own earnings or those of a spouse, parent, or child.
What is not covered by Part A?
Part A does not cover the following: A private room in the hospital or a skilled nursing facility, unless medically necessary. Private nursing care.
What services are paid for under Part B?
The following services are paid for under Part B instead of Part A: All physicians’ services — including those provided by doctors, surgeons and anesthetists in the hospital or a skilled nursing facility, or as part of the home health care or hospice benefits.
What is private nursing care?
Private nursing care. A television or telephone in your room, and personal items like razors or slipper socks, unless the hospital or skilled nursing facility provides these to all patients at no additional charge.
Can you get Medicare for a stay in a nursing home?
If you have been in the hospital “under observation” — even for longer than three days — you do not qualify for Medicare coverage of a stay in a skilled nursing facility. The costs of staying as a long-term resident in a nursing home or assisted living facility.
What are the drugs covered by Medicare?
Some of the drugs Medicare Part B does cover can include: 1 Drugs used with an item of durable medical equipment such as a nebulizer 2 Certain antigens 3 Injectable osteoporosis drugs 4 Erythropoietin by injection 5 Blood clotting factors 6 Oral drugs given for End-Stage Renal Disease 7 Enteral nutrition, such as intravenous and tube feeding 8 Intravenous Immune Globulin (IVIG) that is provided at home 9 Transplant and immunosuppressive drugs
What is Medicare Part B?
Enteral nutrition, such as intravenous and tube feeding. Intravenous Immune Globulin (IVIG) that is provided at home. Transplant and immunosuppressive drugs. Medicare Part B also covers vaccinations and flu shots.
How often does Medicare cover diabetic eye exams?
Eye exams for diabetic retinopathy can be covered once a year, but only if you have diabetes. Medicare beneficiaries who want coverage for routine vision care, glasses and contact lenses may consider a Medicare Advantage plan that offers vision benefits.
What is Medicare Supplement Insurance?
Medicare Supplement Insurance (Medigap) Medicare Supplement Insurance plans are used to cover some of the out-of-pocket expenses associated with Original Medicare, such as deductibles and copayments. Medicare Supplement Insurance plans can work alongside your Original Medicare benefits. You cannot have a Medigap plan and a Medicare Advantage plan ...
Can Medicare beneficiaries get additional coverage?
How Medicare beneficiaries can get coverage for additional services. Medicare beneficiaries looking for coverage for the above services are not entirely out of luck. There are three Medicare options that may be used for coverage outside of or in addition to Original Medicare benefits. Medicare Advantage (Medicare Part C)
Does Medicare cover everything?
Original Medicare doesn’t cover everything. Learn about your coverage options, including Medicare Advantage plans that may cover additional services you need. Medicare provides coverage for a wide range of services and products, but it doesn’t cover everything. In this guide, we take a look at what is not covered by Original Medicare ...
Does Medicare cover prescription drugs?
Prescription drugs. Original Medicare does not cover most prescription drugs. Only a select few prescription drugs are covered by Original Medicare, and only under limited conditions. Medicare Part B also covers vaccinations and flu shots.
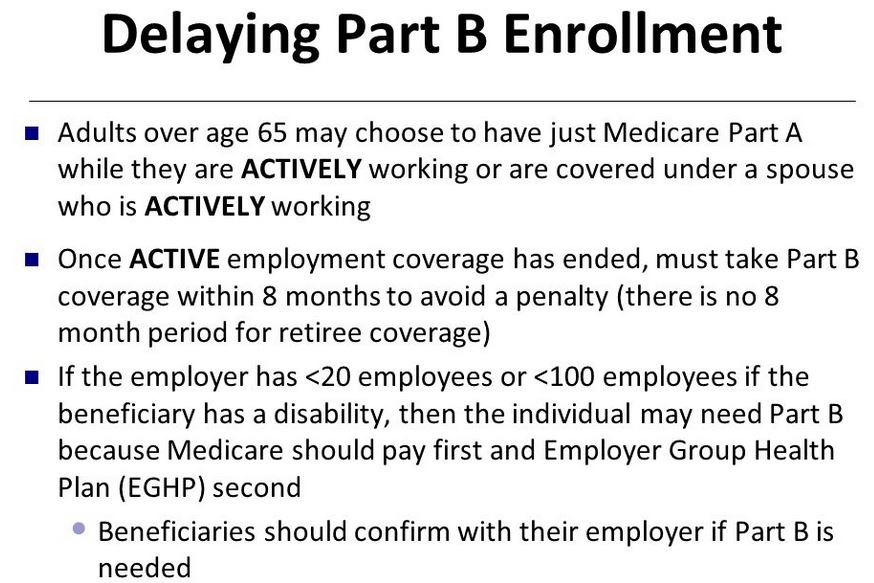
What happens if you don't enroll in Medicare B?
People who don’t enroll in Medicare B when first eligible are charged a late enrollment penalty that amounts to a 10 percent increase in premium for each year they were eligible for Medicare B but not enrolled.
How long does Medicare coverage last?
Medicare coverage begins as soon as your SSDI begins, and Medicare Part A has no premiums as long as you or your spouse (or parent, if you’re a dependent child) worked and paid Medicare taxes for at least 10 years.
How long do you have to pay Medicare taxes if you have end stage renal disease?
You have end-stage renal disease (ESRD) and are receiving dialysis, and either you or your spouse or parent (if you’re a dependent child) worked and paid Medicare taxes for at least 10 years.
How much is Medicare premium for 2020?
These premiums are adjusted annually. Everyone pays for Part B of Original Medicare. In 2020, the standard premium is $144.60/month for those making no more than $87,000 per year ($174,000 per year for married couples filing jointly). For 2020, the threshold for having to pay higher premiums based on income increased.
Do you have to pay Social Security premiums if you are 65?
You may also not have to pay the premium: If you haven’t reached age 65, but you’re disabled and you’ve been receiving Social Security benefits or Railroad Retirement Board disability benefits for two years. You have end-stage renal disease (ESRD) and are receiving dialysis, and either you or your spouse or parent (if you’re a dependent child) ...
Do you have to pay Medicare premiums?
A: Most Medicare-eligible people do not have to pay premiums for Medicare Part A. If you are 65 and you or your spouse has paid Medicare taxes for at least 10 years, you don’t pay a premium for Part A. You may also not have to pay the premium: If you haven’t reached age 65, but you’re disabled and you’ve been receiving Social Security benefits ...
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
Is Medicare Advantage the same as Original Medicare?
What's covered? Note. If you're in a Medicare Advantage Plan or other Medicare plan, your plan may have different rules. But, your plan must give you at least the same coverage as Original Medicare. Some services may only be covered in certain settings or for patients with certain conditions.
Learn About Additional Medicare Insurance
Medigap and Medicare Advantage help you cover what Medicare leaves out.
Do Medicare Parts C And D Cover What Original Medicare Does Not
Because of the limitations of Original Medicare, many enrollees choose to boost their coverage by signing up for a Medicare Supplement plan. Supplements come in many different forms, each having their own levels of coverage and costs. Two options for covering services that Medicare Parts A and B do not cover are Medicare Parts C and D.
Does Medicare Part A Cover 100 Percent
For a qualifying inpatient stay, Medicare Part A covers 100 percent of hospital-specific costs for the first 60 days of the stay after you pay the deductible for that benefit period. Part A doesnt completely cover Days 61-90 or the 60 lifetime reserve days you can use after Day 90. After 60 days, you must pay coinsurance that Part A doesnt cover.
Does Medicare Cover Cataracts
Cataracts cloud the lens of the eye, making it difficult to see. Surgery is generally needed to correct the condition, and under original Medicare, you have two choices in this regard.
What Is Medicare Part A
Medicare Part A is hospital insurance. It may cover your care in certain situations, such as:
Does Medicare Cover Wigs For Cancer Patients
According to the National Institute of Health , some types of chemotherapy cancer treatment cause the hair on the head and other parts of the body to fall out. You could wear a hat or scarf to cover your head, but some people may prefer a wig of natural-looking hair.
Whats The Difference Between Medicare Part A And Medicare Part B
Part A is the hospital services part of Medicare. This benefit covers inpatient care, hospital stays, skilled nursing facility care, hospice care, and medically needed home health care services.
When do you have to be on Medicare before you can get Medicare?
Individuals already receiving Social Security or RRB benefits at least 4 months before being eligible for Medicare and residing in the United States (except residents of Puerto Rico) are automatically enrolled in both premium-free Part A and Part B.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
What is the income related monthly adjustment amount for Medicare?
Individuals with income greater than $85,000 and married couples with income greater than $170,000 must pay a higher premium for Part B and an extra amount for Part D coverage in addition to their Part D plan premium. This additional amount is called income-related monthly adjustment amount. Less than 5 percent of people with Medicare are affected, so most people will not pay a higher premium.
What happens if you don't enroll in Part A?
If an individual did not enroll in premium Part A when first eligible, they may have to pay a higher monthly premium if they decide to enroll later. The monthly premium for Part A may increase up to 10%. The individual will have to pay the higher premium for twice the number of years the individual could have had Part A, but did not sign up.
How long does Medicare take to pay for disability?
A person who is entitled to monthly Social Security or Railroad Retirement Board (RRB) benefits on the basis of disability is automatically entitled to Part A after receiving disability benefits for 24 months.
What is MEC in Medicare?
Medicare and Minimum Essential Coverage (MEC) Medicare Part A counts as minimum essential coverage and satisfies the law that requires people to have health coverage. For additional information about minimum essential coverage (MEC) for people with Medicare, go to our Medicare & Marketplace page.
What is covered benefits and excluded services?
Covered benefits and excluded services are defined in the health insurance plan's coverage documents. from Social Security or the Railroad Retirement Board. You're eligible to get Social Security or Railroad benefits but haven't filed for them yet. You or your spouse had Medicare-covered government employment.
What is Medicare premium?
premium. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage. for. Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
How much will Medicare premiums be in 2021?
People who buy Part A will pay a premium of either $259 or $471 each month in 2021 depending on how long they or their spouse worked and paid Medicare taxes. If you choose NOT to buy Part A, you can still buy Part B. In most cases, if you choose to buy Part A, you must also: Have. Medicare Part B (Medical Insurance)
What does Part B cover?
In most cases, if you choose to buy Part A, you must also: Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. Contact Social Security for more information about the Part A premium. Learn how and when you can sign up for Part A. Find out what Part A covers.
What is premium free Part A?
Most people get premium-free Part A. You can get premium-free Part A at 65 if: The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents.
