If Medicare is primary, it means that Medicare will pay any health expenses first. Your health insurance through your employer will pay second and cover either some or all of the costs left over. If Medicare pays secondary to your insurance through your employer, your employer’s insurance pays first. Medicare covers any remaining costs.
Full Answer
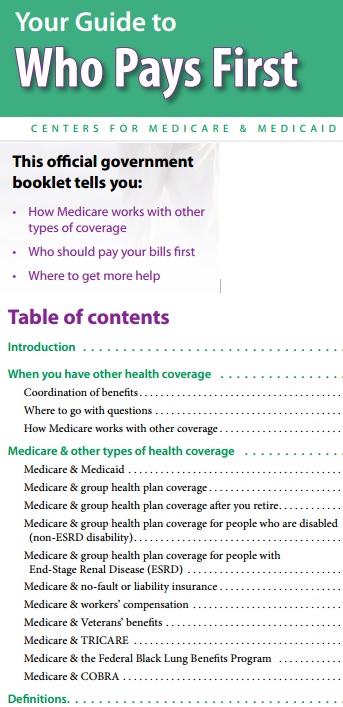
How does Medicare work with employer insurance?
- You will always have the choice of keeping your employer health insurance when you are eligible for Medicare if you work for a large company
- Depending on the size of your company, Medicare may be your primary or secondary insurance
- Medicare also works with COBRA, TRICARE, VA benefits, and HRAs
Is Medicare Secondary to employer insurance?
Medicare will either be the primary payer or secondary payer based on the size of your company, and you can receive Medicare after you retire while on an employer-sponsored plan. There are even more situations when Medicare works with employer insurance, plus other forms of insurance tied to your employment status, like COBRA.
Who pays first with Medicare?
You also may be asked for additional information, like:
- Your Social Security Number (SSN)
- Address
- Medicare effective date (s)
- Whether you have Medicare Part A (Hospital Insurance) and/or Medicare Part B (Medical Insurance) coverage
Can employers pay their employees' Medicare premiums?
Employers can pay Medicare premiums for active employees if the company’s payment plan is integrated with the group’s health plan. For example, the linked group plan must provide minimum value by paying for at least 60 percent of the actuarial value of services received. These payments must be limited to Medicare Part B and Medicare Part D.

Does Medicare get billed first?
gov . Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
Who pays first with a Medicare Advantage plan?
Your workers' compensation will pay first if you're injured or become sick on the job. Medicare will pay second. For any medical services received that are not related to the workers' compensation claim, Medicare will pay first.
Can you have Medicare and employer insurance at the same time?
Can I have Medicare and employer coverage at the same time? Yes, you can have both Medicare and employer-provided health insurance. In most cases, you will become eligible for Medicare coverage when you turn 65, even if you are still working and enrolled in your employer's health plan.
Is Medicare always the primary?
If you don't have any other insurance, Medicare will always be your primary insurance. In most cases, when you have multiple forms of insurance, Medicare will still be your primary insurance.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Does Medicare coverage start the month you turn 65?
The date your coverage starts depends on which month you sign up during your Initial Enrollment Period. Coverage always starts on the first of the month. If you qualify for Premium-free Part A: Your Part A coverage starts the month you turn 65.
Can my employer pay for my Medicare premiums?
Can my employer pay my Medicare premiums? Employers can't pay employees' Medicare premiums directly. However, they can designate funds for workers to apply for health insurance coverage and premium payments with a Section 105 plan.
How do you determine which insurance is primary?
Primary insurance is a health insurance plan that covers a person as an employee, subscriber, or member. Primary insurance is billed first when you receive health care. For example, health insurance you receive through your employer is typically your primary insurance.
How does working affect Medicare?
It depends on how you get your health insurance now and the number of employees that are in the company where you (or your spouse) work. Generally, if you have job-based health insurance through your (or your spouse's) current job, you don't have to sign up for Medicare while you (or your spouse) are still working.
When Can Medicare be a secondary payer?
Make sure your healthcare providers know that you have more insurance than just Medicare. Situations when Medicare is a secondary payer include when: You are covered by a group health plan (GHP) through employment, self-employed, or a spouse's employment, AND the employer has more than 20 employees.
How Does Medicare pay as a secondary payer?
As secondary payer, Medicare pays the lowest of the following amounts: (1) Excess of actual charge minus the primary payment: $175−120 = $55. (2) Amount Medicare would pay if the services were not covered by a primary payer: . 80 × $125 = $100.
Does Medicare automatically forward claims to secondary insurance?
If a Medicare member has secondary insurance coverage through one of our plans (such as the Federal Employee Program, Medex, a group policy, or coverage through a vendor), Medicare generally forwards claims to us for processing.
If you're still working when you turn 65, you may be able to delay Medicare enrollment without penalty
If you're like many Americans getting ready to turn 65, you still have health insurance through an employer plan. However, just because you aren't ready to retire doesn't mean you aren't eligible for Medicare. In this post, we look at Medicare and employer coverage to help you understand your options and avoid late penalties.
How does Medicare coordinate with employer coverage?
The way Medicare coordinates with an employer insurance plan depends on the answers to two questions:
How Medicare works with an employer health plan
Medicare defines a large company as one that employs 20 or more people. If your group health plan is through a large employer, Medicare is your secondary payer. That means that Medicare pays after your employer plan pays its share.
Enrolling in Medicare when actively employed
If you are actively employed when you turn 65, Medicare enrollment is not automatic. That means you must sign up for Medicare through Social Security.
Keep your proof of creditable coverage
Having creditable coverage when you become eligible for Medicare qualifies you for a Special Enrollment Period (SEP). This means you can delay Medicare enrollment without incurring late penalties. However, you must be able to prove you had creditable coverage to qualify for the SEP.
What happens with Medicare if you go back to work after you retire?
Many Americans decide to go back to work after they retire. If this describes you, and your new job offers a group health plan, you may cancel Part B. Then, when you're ready to retire again, you'll qualify for another SEP. You'll also be able to enroll in a Medigap plan without having to undergo medical underwriting.
How Medicare works with COBRA
COBRA is a health insurance program that provides continued coverage for people who are no longer actively employed. The "actively employed" part is crucial. Remember, Medicare can only be secondary coverage if you are actively employed.
Which pays first, Medicare or ESRD?
The group health plan pays first for qualified services, and Medicare is the secondary payer. You have ESRD and COBRA insurance and have been eligible for Medicare for 30 months or fewer. COBRA pays first in this situation.
How long do you have to be on Cobra to get Medicare?
You have ESRD and COBRA insurance and have been eligible for Medicare for at least 30 months. COBRA is the secondary payer in this situation, and Medicare pays first for qualified services. You are 65 or over – or you are under 65 and have a disability other than ESRD – and are covered by either COBRA insurance or a retiree group health plan.
What is a group health plan?
The group health plan is your secondary payer after Medicare pays first for your health care costs. You have End-Stage Renal Disease (ESRD), are covered by a group health plan and have been entitled to Medicare for at least 30 months. The group health plan pays second, after Medicare. You have ESRD and COBRA insurance and have been eligible ...
What is Medicare Advantage?
A Medicare Advantage plan replaces your Original Medicare coverage. In addition to those basic benefits, Medicare Advantage plans can also offer some additional coverage for things like prescription drugs, dental, vision, hearing aids, SilverSneakers programs and more.
Is Medicare a secondary payer?
Medicare serves as the secondary payer in the following situations: You are 65 or older and are covered by a group health plan because you or your spouse is still working and the employer has 20 or more employees. The group health plan is the primary payer, and Medicare pays second.
Does tricare work with Medicare?
You may use both types of insurance for your health care , but they will operate separately from each other. TRICARE does work with Medicare. Active-duty military personnel who are enrolled in Medicare may use TRICARE as a primary payer, and then Medicare pays second as a secondary payer. For inactive members of the military who are enrolled in ...
Is Medicare Part A or Part B?
While you must remain enrolled in Medicare Part A and Part B (and pay the associated premiums), your Medicare Advantage plan serves as your Medicare coverage. Medicare Part D, which provides coverage for prescription drugs, is another type of private Medicare insurance.
Why do I need additional coverage for Medicare?
You may want additional coverage to make sure you get all the healthcare services you need. Medicare and other insurers, on the other hand, have another vested interest. If you have more than one health plan, they may be able to shift the burden of payment onto the other party. Don't worry.
How does tricare work?
Third, TRICARE and Medicare work in concert. Medicare acts as the primary payer for Medicare-covered services and TRICARE covers any Medicare deductibles or coinsurance amount that relates to those services. When a service is not covered by Medicare, TRICARE will act as the primary payer.
How many full time employees can you have if you are not ESRD?
If you have a disability that is not ESRD - AND- your employer has less than 100 full-time employees. If you have ESRD -AND- your 30-month coordination period for ESRD has ended. If you are 65 years or older -AND- your employer has more than 20 full-time employees.
How long can you keep your health insurance after you leave your job?
Thanks to the Consolidated Omnibus Budget Reconciliation Act (COBRA) of 1985 you can continue your employer-sponsored health plan after you leave your job. The law requires employers of 20 or more full-time employees to offer continued access to their health plan for a period of time, usually 18 months, after your job ends by way of termination or a layoff. The duration of COBRA coverage may be extended up to 36 months if certain conditions are met.
What happens if you don't meet the criteria for Medicare?
If you do not meet the criteria for Medicare to pay first, your employer-sponsored health plan will be billed instead.
Is Worker's Compensation a state mandated plan?
Worker's compensation works a bit differently than does your employer-sponsored health plan. It is a state-mandated agreement between you and your employer that states you will not sue them as long as they cover your medical expenses for any on-the-job injuries.
Does Medicare cover everything?
Why You May Want More Than What Medicare Offers. Medicare provides health care for more than 59.8 million Americans, but that does not mean it necessarily covers everything they need. Consider these common items that Medicare leaves you to pay for out of pocket: Acupuncture.
What is the original Medicare plan?
The Original Medicare Plan—This a fee-for-service plan . Thismeans you are usually charged a fee for each health care service orsupply you get. This plan, managed by the Federal Government, isavailable nationwide. You will stay in the Original Medicare Planunless you choose to join a Medicare Advantage Plan.
Why does Bill have Medicare?
Bill has Medicare coverage because of permanent kidney failure.He also has group health plan coverage through his company.Bill’s group health plan coverage will be the primary payer forthe first 30 months after he becomes eligible for Medicare. After30 months, Medicare becomes the primary payer.
What does Medicare Part B cover?
Medicare Part B—Medical Insurance, helps pay fordoctors’services and outpatient care. It also covers some other medicalservices that Medicare Part A doesn’t cover, such as some of theservices of physical and occupational therapists, and some homehealth care. Medicare Part Bhelps pay for these covered services andsupplies when they are medically necessary.
Which Medicare plans cover more services?
Medicare Advantage Plans and Other Medicare HealthPlans—These plans, which include HMOs, PPOs, and PFFS plans,may cover more services and have lower out-of-pocket costs than theOriginal Medicare Plan. However, in some plans, like HMOs, youmay only be able to see certain doctors or go to certain hospitals.
Does Medicare know if you have other insurance?
Medicaredoesn’t automatically know if you have other insurance orcoverage. Medicare sends you a questionnaire called the “InitialEnrollment Questionnaire”about three months before you areentitled to Medicare. This questionnaire will ask you if you havegroup health plan insurance through your work or that of a familymember and if you plan to keep it. Your answers to thisquestionnaire are used to help Medicare set up your file, and makesure that your claimsare paid by the right insurance.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
How long does Medicare coverage last?
This special period lasts for eight months after the first month you go without your employer’s health insurance. Many people avoid having a coverage gap by signing up for Medicare the month before your employer’s health insurance coverage ends.
Does Cobra pay for primary?
The only exception to this rule is if you have End-Stage Renal Disease and COBRA will pay primary. Your COBRA coverage typically ends once you enroll in Medicare. However, you could potentially get an extension of the COBRA if Medicare doesn’t cover everything the COBRA plan does like dental or vision insurance.
Does Medicare pay second to employer?
Your health insurance through your employer will pay second and cover either some or all of the costs left over. If Medicare pays secondary to your insurance through your employer, your employer’s insurance pays first. Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance ...
Does Medicare cover health insurance?
Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance coverage in different ways. If your company has 20 employees or less and you’re over 65, Medicare will pay primary. Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage ...
Can an employer refuse to pay Medicare?
The first problem is that your employer can legally refuse to make any health-related medical payments until Medicare pays first. If you delay coverage and your employer’s health insurance pays primary when it was supposed to be secondary and pick up any leftover costs, it could recoup payments.
How to learn more about Medicare?
How to Learn More About Your Medicare Options. Primary insurance isn't too hard to understand; it's just knowing which insurance pays the claim first. Medical billing personnel can always help you figure it out if you're having trouble. While it's not hard to understand primary insurance, Medicare is its own beast.
What is a small employer?
Those with small employer health insurance will have Medicare as the primary insurer. A small employer means less than 20 employees in the company. When you have small employer coverage, Medicare will pay first, and the plan pays second. If your employer is small, you must have both Part A and Part B. Having small employer insurance without ...
Is Medicare a primary or secondary insurance?
Mostly, Medicare is primary. The primary insurer is the one that pays the claim first, whereas the secondary insurer pays second. With a Medigap policy, the supplement is secondary. Medicare pays claims first, and then Medigap pays. But, depending on the other policy, you have Medicare could be a secondary payer.
Does Medicare pay your claims?
Since the Advantage company pays the claims, that plan is primary. Please note that Medicare WON’T pay your claims when you have an Advantage plan. Medicare doesn’t become secondary to an Advantage plan. So, you’ll rely on the Advantage plan for claim approvals.
Can you use Medicare at a VA hospital?
Medicare and Veterans benefits don’t work together; both are primary. When you go to a VA hospital, Veteran benefits are primary. Then, if you go to a civilian doctor or hospital, Medicare is primary. But, you CAN’T use Veterans benefits at a civilian doctor. Also, you can’t use Medicare benefits at the VA.
Is Medicare primary insurance in 2021?
Updated on July 13, 2021. Many beneficiaries wonder if Medicare is primary insurance. But, the answer depends on several factors. While there are times when Medicare becomes secondary insurance, for the most part, it’s primary. Let’s go into further detail about what “primary” means, and when it applies.
Is Medicare a part of tricare?
Medicare is primary to TRICARE. If you have Part A, you need Part B to remain eligible for TRICARE. But, Part D isn’t a requirement. Also, TRICARE covers your prescriptions. Your TRICARE will be similar to a Medigap plan; it covers deductibles and coinsurances.