When it comes to Medicare, who pays first?
pays first and Medicare pays second during a coordination period that lasts up to 30 months . After the coordination period ends, Medicare pays first and the group health plan pays second . If you originally got Medicare due to your age or a disability other than ESRD, and your group health plan was your primary payer, then it will continue
Who pays first Medicare or supplemental insurance?
This means that the group health plan is the primary payer (see example below). The group health plan pays first on your hospital and medical bills. If the group health plan didn’t pay all of your bill, the doctor or other provider should send the bill to Medicare for secondary payment.
Who pays first Medicaid or Tricare?
If you're not on active duty, Medicare pays first for Medicare-covered services, and TRICARE may pay second. If you get items or services from a military hospital or any other federal health care provider, TRICARE pays first.
Which insurance pays first?
Nov 23, 2021 · Medicare pays first when it serves as your primary payer. If you have Medicare as well as another type of insurance, your coverage is provided through a coordination of benefits. In some situations, Medicare will serve as your primary payer, which means Medicare pays first.
See more
Aug 23, 2018 · If you have Medicare and other health coverage, each type of coverage is called a “payer.” When there’s more than one payer, “coordination of benefits” rules decide who pays first. The “primary payer” pays what it owes on your bills first, and then your provider sends the rest to the “secondary payer” to pay. In some cases, there may also be a “third payer.”

Is Medicare always the first payer?
Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
Does Medicare pay first or second?
If the employer has 100 or more employees, then your family member's group health plan pays first, and Medicare pays second. If the employer has less than 100 employees, but is part of a multi-employer or multiple employer group health plan, your family member's group health plan pays first and Medicare pays second.
How Does Medicare pay as a secondary payer?
This is because when Medicare is primary to your other insurance, your other insurance may not pay for costs until Medicare pays—so you would be responsible for paying these costs out of pocket. When Medicare is secondary, your current insurance will pay the majority of the cost for covered services.
Who pays for my Medicare?
Medicare is funded by the Social Security Administration. Which means it's funded by taxpayers: We all pay 1.45% of our earnings into FICA - Federal Insurance Contributions Act - which go toward Medicare. Employers pay another 1.45%, bringing the total to 2.9%.
When two insurance which one is primary?
Primary insurance: the insurance that pays first is your “primary” insurance, and this plan will pay up to coverage limits. You may owe cost sharing. Secondary insurance: once your primary insurance has paid its share, the remaining bill goes to your “secondary” insurance, if you have more than one health plan.Jan 21, 2022
How do you determine which insurance is primary?
Primary insurance is a health insurance plan that covers a person as an employee, subscriber, or member. Primary insurance is billed first when you receive health care. For example, health insurance you receive through your employer is typically your primary insurance.Oct 8, 2019
Who pays if you buy insurance directly from a marketplace?
With most job-based health insurance plans, your employer pays part of your monthly premium. If you enroll in a Marketplace plan instead, the employer won't contribute to your premiums.
Does Medicare automatically send claims to secondary insurance?
Medicare will send the secondary claims automatically if the secondary insurance information is on the claim. As of now, we have to submit to primary and once the payments are received than we submit the secondary.Aug 19, 2013
How do I submit a secondary claim to Medicare?
Medicare Secondary Payer (MSP) claims can be submitted electronically to Novitas Solutions via your billing service/clearinghouse, directly through a Secure File Transfer Protocol (SFTP) connection, or via Novitasphere portal's batch claim submission.Sep 9, 2021
Does everyone have to pay Medicare?
Everyone pays for Part B of Original Medicare. In 2020, the standard premium is $144.60/month for those making no more than $87,000 per year ($174,000 per year for married couples filing jointly). For 2020, the threshold for having to pay higher premiums based on income increased.
Does everyone pay the same for Medicare?
Most people will pay the standard premium amount. If your modified adjusted gross income is above a certain amount, you may pay an Income Related Monthly Adjustment Amount (IRMAA). Medicare uses the modified adjusted gross income reported on your IRS tax return from 2 years ago.
Do you have to pay for Medicare?
Most people don't have to pay a monthly premium for their Medicare Part A coverage. If you've worked for a total of 40 quarters or more during your lifetime, you've already paid for your Medicare Part A coverage through those income taxes.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
Which pays first, Medicare or ESRD?
The group health plan pays first for qualified services, and Medicare is the secondary payer. You have ESRD and COBRA insurance and have been eligible for Medicare for 30 months or fewer. COBRA pays first in this situation.
How long do you have to be on Cobra to get Medicare?
You have ESRD and COBRA insurance and have been eligible for Medicare for at least 30 months. COBRA is the secondary payer in this situation, and Medicare pays first for qualified services. You are 65 or over – or you are under 65 and have a disability other than ESRD – and are covered by either COBRA insurance or a retiree group health plan.
What is a group health plan?
The group health plan is your secondary payer after Medicare pays first for your health care costs. You have End-Stage Renal Disease (ESRD), are covered by a group health plan and have been entitled to Medicare for at least 30 months. The group health plan pays second, after Medicare. You have ESRD and COBRA insurance and have been eligible ...
What is Medicare Advantage?
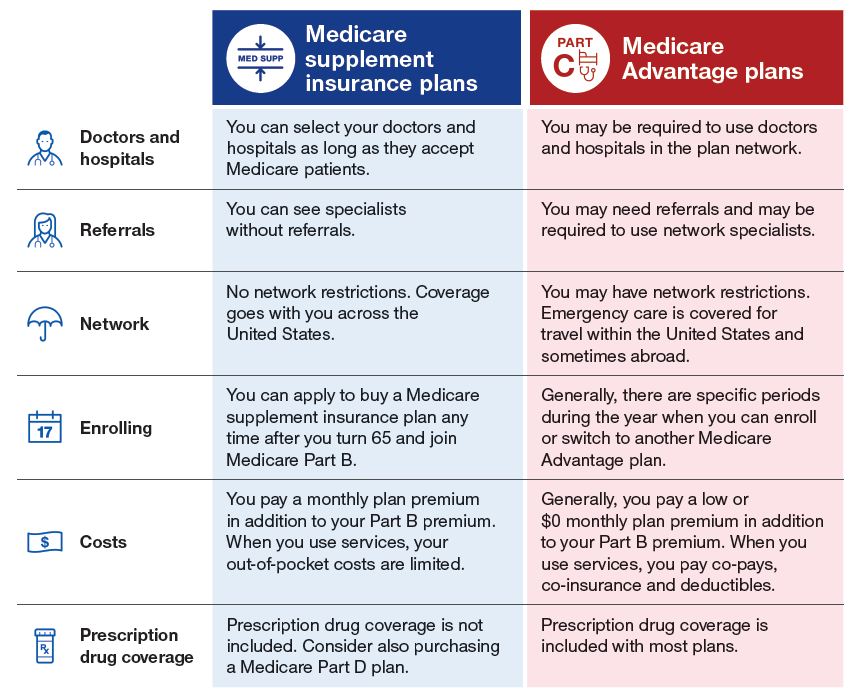
A Medicare Advantage plan replaces your Original Medicare coverage. In addition to those basic benefits, Medicare Advantage plans can also offer some additional coverage for things like prescription drugs, dental, vision, hearing aids, SilverSneakers programs and more.
Is Medicare a secondary payer?
Medicare serves as the secondary payer in the following situations: You are 65 or older and are covered by a group health plan because you or your spouse is still working and the employer has 20 or more employees. The group health plan is the primary payer, and Medicare pays second.
Does tricare work with Medicare?
You may use both types of insurance for your health care , but they will operate separately from each other. TRICARE does work with Medicare. Active-duty military personnel who are enrolled in Medicare may use TRICARE as a primary payer, and then Medicare pays second as a secondary payer. For inactive members of the military who are enrolled in ...
Is Medicare Part A or Part B?
While you must remain enrolled in Medicare Part A and Part B (and pay the associated premiums), your Medicare Advantage plan serves as your Medicare coverage. Medicare Part D, which provides coverage for prescription drugs, is another type of private Medicare insurance.
What is Medicare and other health insurance called?
If you have Medicare and other health coverage, each type of coverage is called a “payer.”. When there’s more than one payer, “coordination of benefits” rules decide who pays first. The “primary payer” pays what it owes on your bills first, and then your provider sends the rest to the “secondary payer” to pay. ...
What is the number to call for Medicare?
If you have questions about who pays first, or if your coverage changes, call the Benefits Coordination & Recovery Center (BCRC) toll-free at 1-855-798-2627. TTY users should call 1-855-797-2627. To better serve you, have your Medicare number ready when you call.
Is there a third payer for Medicare?
In some cases, there may also be a “third payer.”. Whether Medicare pays first depends on a number of things. Be sure to tell your doctor and other health care providers if you have health coverage in addition to Medicare. This will help them send your bills to the correct payer to avoid delays.
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
What is extra help?
And, you'll automatically qualify for. Extra Help. A Medicare program to help people with limited income and resources pay Medicare prescription drug program costs, like premiums, deductibles, and coinsurance. paying for your.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
Can you spend down on medicaid?
Medicaid spenddown. Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid . The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid.
Not sure if you should sign up for Medicare if you get VA benefits? Even the VA says it's a good idea
If you qualify for both Veteran's Affair (VA) and Medicare benefits, who pays for healthcare services can be confusing. Unlike other types of supplemental coverage, it isn't a matter of who pays first between the VA and Medicare. Instead, it comes down to where you receive care. If it's a VA facility, then your VA benefits pay.
What Does the Department of Veterans Affairs Cover?
It's important to remember that the VA only covers care when you go to a VA facility. Your condition does not have to be related to your service.
Should You Sign Up for Medicare Part A If You Get VA Benefits?
Original Medicare includes two parts, A and B. Medicare Part A provides outpatient care received in a hospital or skilled nursing facility (SNF). And we nearly always recommend signing up for Medicare Part A – even if you get VA health benefits.
Should You Sign Up for Medicare Part B If You Get VA Benefits?
Medicare Part B is the second half of Original Medicare. It covers inpatient medical services like doctor appointments, mental health care, and durable medical equipment.
When Should You Sign Up for Medicare?
U.S. citizens age 65 and older qualify for the Medicare program. You may also be eligible if you collect either Railroad Retirement Board (RRB) or Social Security disability benefits for 24 months. In addition, people who have ALS (Lou Gehrig's disease) or end-stage renal disease (ESRD) qualify for Medicare.
Do Vets Need a Medigap Plan?
Medicare Supplement Insurance, more commonly known as Medigap, helps pay your out-of-pocket costs when you have Original Medicare. If you plan to rely more on your Medicare benefits than your VA coverage, you may want to sign up for a Medigap plan.
Do You Need Medicare Advantage If You Have VA Benefits?
Medicare Part C, more commonly known as Medicare Advantage, provides the same coverage as Original Medicare. However, most Advantage plans provide additional benefits, like prescription drug coverage and routine dental care.