What it means to pay primary/secondary
- The insurance that pays first (primary payer) pays up to the limits of its coverage.
- The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover.
- The secondary payer (which may be Medicare) may not pay all the remaining costs.
Full Answer
Does Medicare get billed first?
Medicare will be billed first, then your supplement plan will be billed second. Does Medicare send claims to your Medicare Supplement insurance? Yes, all claims will be sent to Medicare first, then Medicare will bill the remainder to your Medicare Supplement carrier .
Which insurance pays first?
First Midwest Bank has agreed to pay a $253,500 fine over flood insurance violations, the Federal Reserve said Thursday. The Chicago-based bank did not admit to wrongdoing as part of its agreement with the Fed, but the settlement allows it to avoid formal ...
When does Medicare pay first?
Medicare will pay first. Medicare will pay second. If you are 65 years or older -AND- your employer has less than 20 full-time employees. If you have a disability that is not ESRD - AND- your employer has less than 100 full-time employees. If you have ESRD -AND- your 30-month coordination period for ESRD has ended.
Can you have private insurance and Medicare?
It’s possible to have both Medicare and private insurance. You may have both if you’re covered under an employer-provided plan, COBRA, or TRICARE. If you have both Medicare and private insurance, there are guidelines about which provider pays first for your healthcare services.

Does Medicare get billed first?
gov . Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
Is Medicare a Always primary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
Does Medicare come first or second?
If you're not currently employed, Medicare pays first, and your group health plan coverage pays second. I'm under 65, disabled, retired and I have group health coverage from my family member's current employer.
Can I have Medicare and private insurance at the same time?
It is possible to have both private insurance and Medicare at the same time. When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer.
Does Medicare automatically forward claims to secondary insurance?
If a Medicare member has secondary insurance coverage through one of our plans (such as the Federal Employee Program, Medex, a group policy, or coverage through a vendor), Medicare generally forwards claims to us for processing.
Will secondary pay if primary denies?
If your primary insurance denies coverage, secondary insurance may or may not pay some part of the cost, depending on the insurance. If you do not have primary insurance, your secondary insurance may make little or no payment for your health care costs.
Will Medicare pay my primary insurance deductible?
“Medicare pays secondary to other insurance (including paying in the deductible) in situations where the other insurance is primary to Medicare.
Do retirees pay Medicare premiums?
According to the CMS, most Medicare beneficiaries will pay the standard Medicare Part B premium amount. If you're enrolled in a CalPERS Medicare health plan, you must pay for and maintain enrollment in Medicare Part B to remain enrolled in the CalPERS health program.
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
What will Medicare not pay for?
Generally, Original Medicare does not cover dental work and routine vision or hearing care. Original Medicare won't pay for routine dental care, visits, cleanings, fillings dentures or most tooth extractions. The same holds true for routine vision checks. Eyeglasses and contact lenses aren't generally covered.
What happens if you don't have health insurance and you go to the hospital?
However, if you don't have health insurance, you will be billed for all medical services, which may include doctor fees, hospital and medical costs, and specialists' payments. Without an insurer to absorb some or even most of those costs, the bills can increase exponentially.
Are you automatically enrolled in Medicare if you are on Social Security?
Initial Enrollment Period for Part B If you are already getting benefits from Social Security or the RRB, you will automatically get Part A and Part B starting on the first day of the month when you turn 65.
Which pays first, Medicare or ESRD?
The group health plan pays first for qualified services, and Medicare is the secondary payer. You have ESRD and COBRA insurance and have been eligible for Medicare for 30 months or fewer. COBRA pays first in this situation.
How long do you have to be on Cobra to get Medicare?
You have ESRD and COBRA insurance and have been eligible for Medicare for at least 30 months. COBRA is the secondary payer in this situation, and Medicare pays first for qualified services. You are 65 or over – or you are under 65 and have a disability other than ESRD – and are covered by either COBRA insurance or a retiree group health plan.
What is a group health plan?
The group health plan is your secondary payer after Medicare pays first for your health care costs. You have End-Stage Renal Disease (ESRD), are covered by a group health plan and have been entitled to Medicare for at least 30 months. The group health plan pays second, after Medicare. You have ESRD and COBRA insurance and have been eligible ...
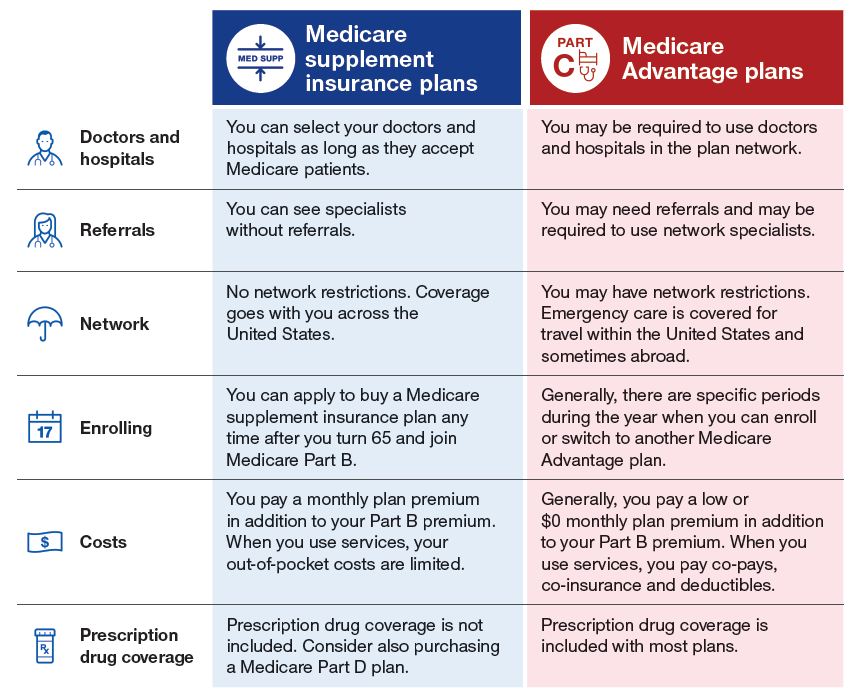
What is Medicare Advantage?
A Medicare Advantage plan replaces your Original Medicare coverage. In addition to those basic benefits, Medicare Advantage plans can also offer some additional coverage for things like prescription drugs, dental, vision, hearing aids, SilverSneakers programs and more.
Is Medicare a secondary payer?
Medicare serves as the secondary payer in the following situations: You are 65 or older and are covered by a group health plan because you or your spouse is still working and the employer has 20 or more employees. The group health plan is the primary payer, and Medicare pays second.
Does tricare work with Medicare?
You may use both types of insurance for your health care , but they will operate separately from each other. TRICARE does work with Medicare. Active-duty military personnel who are enrolled in Medicare may use TRICARE as a primary payer, and then Medicare pays second as a secondary payer. For inactive members of the military who are enrolled in ...
Is Medicare Part A or Part B?
While you must remain enrolled in Medicare Part A and Part B (and pay the associated premiums), your Medicare Advantage plan serves as your Medicare coverage. Medicare Part D, which provides coverage for prescription drugs, is another type of private Medicare insurance.
Why do I need additional coverage for Medicare?
You may want additional coverage to make sure you get all the healthcare services you need. Medicare and other insurers, on the other hand, have another vested interest. If you have more than one health plan, they may be able to shift the burden of payment onto the other party. Don't worry.
How does tricare work?
Third, TRICARE and Medicare work in concert. Medicare acts as the primary payer for Medicare-covered services and TRICARE covers any Medicare deductibles or coinsurance amount that relates to those services. When a service is not covered by Medicare, TRICARE will act as the primary payer.
What happens if you don't meet the criteria for Medicare?
If you do not meet the criteria for Medicare to pay first, your employer-sponsored health plan will be billed instead.
Is Worker's Compensation a state mandated plan?
Worker's compensation works a bit differently than does your employer-sponsored health plan. It is a state-mandated agreement between you and your employer that states you will not sue them as long as they cover your medical expenses for any on-the-job injuries.
Does Medicare cover everything?
Why You May Want More Than What Medicare Offers. Medicare provides health care for more than 59.8 million Americans, but that does not mean it necessarily covers everything they need. Consider these common items that Medicare leaves you to pay for out of pocket: Acupuncture.
Does Medicare pay for two different health plans?
This could save you considerable dollars since you would not have to pay the premium for two different plans. When you have both Medicare and an employer-sponsored health plan, Medicare will pay first only in certain circumstances.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is the original Medicare plan?
The Original Medicare Plan—This a fee-for-service plan . Thismeans you are usually charged a fee for each health care service orsupply you get. This plan, managed by the Federal Government, isavailable nationwide. You will stay in the Original Medicare Planunless you choose to join a Medicare Advantage Plan.
Why does Bill have Medicare?
Bill has Medicare coverage because of permanent kidney failure.He also has group health plan coverage through his company.Bill’s group health plan coverage will be the primary payer forthe first 30 months after he becomes eligible for Medicare. After30 months, Medicare becomes the primary payer.
What does Medicare Part B cover?
Medicare Part B—Medical Insurance, helps pay fordoctors’services and outpatient care. It also covers some other medicalservices that Medicare Part A doesn’t cover, such as some of theservices of physical and occupational therapists, and some homehealth care. Medicare Part Bhelps pay for these covered services andsupplies when they are medically necessary.
Which Medicare plans cover more services?
Medicare Advantage Plans and Other Medicare HealthPlans—These plans, which include HMOs, PPOs, and PFFS plans,may cover more services and have lower out-of-pocket costs than theOriginal Medicare Plan. However, in some plans, like HMOs, youmay only be able to see certain doctors or go to certain hospitals.
Does Medicare know if you have other insurance?
Medicaredoesn’t automatically know if you have other insurance orcoverage. Medicare sends you a questionnaire called the “InitialEnrollment Questionnaire”about three months before you areentitled to Medicare. This questionnaire will ask you if you havegroup health plan insurance through your work or that of a familymember and if you plan to keep it. Your answers to thisquestionnaire are used to help Medicare set up your file, and makesure that your claimsare paid by the right insurance.
What is Medicare and other health insurance called?
If you have Medicare and other health coverage, each type of coverage is called a “payer.”. When there’s more than one payer, “coordination of benefits” rules decide who pays first. The “primary payer” pays what it owes on your bills first, and then your provider sends the rest to the “secondary payer” to pay. ...
What is the number to call for Medicare?
If you have questions about who pays first, or if your coverage changes, call the Benefits Coordination & Recovery Center (BCRC) toll-free at 1-855-798-2627. TTY users should call 1-855-797-2627. To better serve you, have your Medicare number ready when you call.
Is there a third payer for Medicare?
In some cases, there may also be a “third payer.”. Whether Medicare pays first depends on a number of things. Be sure to tell your doctor and other health care providers if you have health coverage in addition to Medicare. This will help them send your bills to the correct payer to avoid delays.
Who pays first for Medicare?
When it comes to Medicare, ‘Who Pays First’ is a very common dilemma these days. That’s because people are working longer than ever and often have other insurance coverage in place alongside Medicare. In most cases of other coverage, one insurance becomes the primary payer, and the other insurance becomes the secondary payer.
Is Medicare the same as Medicaid?
Original Medicare is a federal health insurance program for people age 65 or older, and for people with certain disabilities. Medicaid is a joint federal and state program for people with limited incomes and assets. If you have qualified for both, Medicare will always pay first, and Medicaid will pay second.
Is Medicare primary or secondary?
Employer health plans with 20 or more employees will be primary and Medicare will be secondary. If there are less than 20 employees, then Medicare is primary and your group health plan is secondary. Again, in both of these situations, you would not need a Medigap plan because you already have a primary and secondary payer.
Does Medicare pay for retirees?
Medicare and Retiree Coverage. If you have group health benefits through a former employer or a spouse’s former employer, Medicare pays first. This means you must be enrolled in both Medicare Parts A and B. After Medicare pays out its benefits, it will send the remainder of those bills on to your retiree health plan.
Is Cobra more expensive than Medicare?
However, COBRA benefits for people over 65 can often be enormously expensive. Be sure to compare costs/benefits against the cost of Medicare with a Medigap plan. Often we find the Medigap option to be significantly less expensive.
Can you get Medicare early if you are 65?
Medicare and Group Health Coverage for Beneficiaries Under 65. Some people qualify for Medicare early due to a disability. If that employee works for a company with less than 100 employees, Medicare will be primary. If the employer has more than 100 employees, the larger group health plan will pay first, and Medicare will pay secondary.
Do you have to use Medicare or VA?
If you wish to use your VA benefits, you must seek care from a VA facility. Many Veterans choose to have Medicare as well as VA benefits so that they have the freedom to treat with a civilian doctor if they wish to do so.
How to learn more about Medicare?
How to Learn More About Your Medicare Options. Primary insurance isn't too hard to understand; it's just knowing which insurance pays the claim first. Medical billing personnel can always help you figure it out if you're having trouble. While it's not hard to understand primary insurance, Medicare is its own beast.
Is Medicare primary insurance in 2021?
Updated on July 13, 2021. Many beneficiaries wonder if Medicare is primary insurance. But, the answer depends on several factors. While there are times when Medicare becomes secondary insurance, for the most part, it’s primary. Let’s go into further detail about what “primary” means, and when it applies.
Is Medicare a primary or secondary insurance?
Mostly, Medicare is primary. The primary insurer is the one that pays the claim first, whereas the secondary insurer pays second. With a Medigap policy, the supplement is secondary. Medicare pays claims first, and then Medigap pays. But, depending on the other policy, you have Medicare could be a secondary payer.
Does Medicare pay your claims?
Since the Advantage company pays the claims, that plan is primary. Please note that Medicare WON’T pay your claims when you have an Advantage plan. Medicare doesn’t become secondary to an Advantage plan. So, you’ll rely on the Advantage plan for claim approvals.
Can you use Medicare at a VA hospital?
Medicare and Veterans benefits don’t work together; both are primary. When you go to a VA hospital, Veteran benefits are primary. Then, if you go to a civilian doctor or hospital, Medicare is primary. But, you CAN’T use Veterans benefits at a civilian doctor. Also, you can’t use Medicare benefits at the VA.
Is Medicare a part of tricare?
Medicare is primary to TRICARE. If you have Part A, you need Part B to remain eligible for TRICARE. But, Part D isn’t a requirement. Also, TRICARE covers your prescriptions. Your TRICARE will be similar to a Medigap plan; it covers deductibles and coinsurances.
