Mostly, Medicare is primary. The primary insurer is the one that pays the claim first, whereas the secondary insurer pays second. With a Medigap policy, the supplement is secondary. Medicare pays claims first, and then Medigap pays. But, depending on the other policy, you have Medicare could be a secondary payer.
What does Medicare Part a pay for?
Medicare Part A premiums from people who aren't eligible for premium-free Part A What does it pay for? Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
What does Medicare pay for hospital stays?
Medicare is the federal health insurance program for adults aged 65 and older, as well as for some younger people. Medicare pays for inpatient hospital stays of a certain length. Medicare covers the first 60 days of a hospital stay after the person has paid the deductible.
Does Medicare pay for inpatient care?
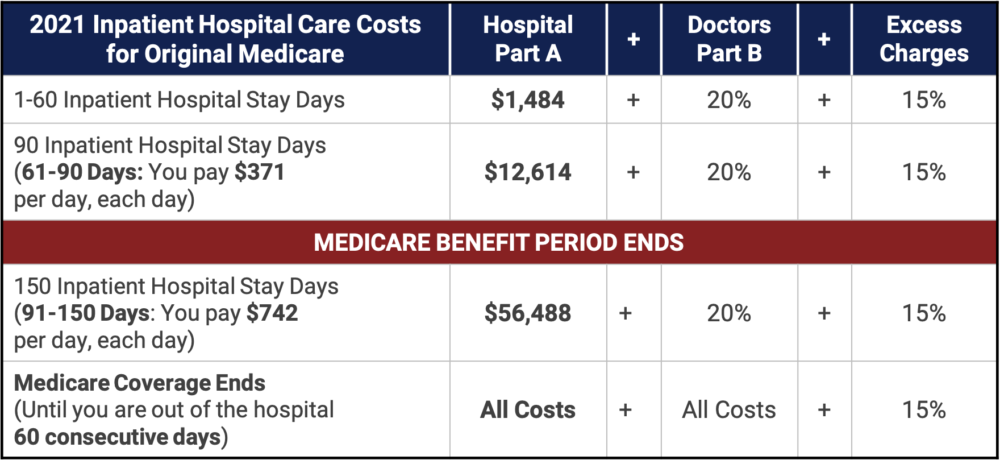
The extent to which Medicare covers the costs of inpatient care depends on the length of the person’s stay in the healthcare facility. Also, Medicare only begins to pay for inpatient treatment once a person has paid a deductible. In addition, after day 60 of a hospital stay, a daily coinsurance applies.
Will Medicare pay for mental health services?
If this happens, you may have to pay some or all of the costs. Ask questions so you understand why your doctor is recommending certain services and whether Medicare will pay for them. Inpatient mental health care in a psychiatric hospital is limited to 190 days in a lifetime. covers your doctors’ services you get while you’re in a hospital.
Does Medicare cover 100% of hospital costs?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
What part of Medicare pays for hospitalization?
Medicare Part A hospital insuranceMedicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
Does Medicare supplement pay hospital deductible?
You can buy private Medicare Supplement insurance to cover Medicare's out-of-pocket expenses, including the hospital deductible. However, if you're in a Medicare Advantage Plan, you can only purchase a Medicare Supplement plan if your Medicare Advantage plan coverage is ending.
Does Medicare pay for hospital stays?
Medicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual's reserve days. Medicare provides 60 lifetime reserve days.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
What is the maximum out of pocket for Medicare?
Out-of-pocket limit. In 2021, the Medicare Advantage out-of-pocket limit is set at $7,550. This means plans can set limits below this amount but cannot ask you to pay more than that out of pocket.
What does Medicare supplement plan a cover?
Medicare Supplement insurance Plan A covers 100% of four things: Medicare Part A coinsurance payments for inpatient hospital care up to an additional 365 days after Medicare benefits are used up. Medicare Part B copayment or coinsurance expenses. The first 3 pints of blood used in a medical procedure.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
What is the 3 day rule for Medicare?
The 3-day rule requires the patient have a medically necessary 3-consecutive-day inpatient hospital stay. The 3-consecutive-day count doesn't include the discharge day or pre-admission time spent in the Emergency Room (ER) or outpatient observation.
Do all hospitals accept Medicare?
Not all hospitals accept Medicare, but luckily, the vast majority of hospitals do. Generally, the hospitals that do not accept Medicare are Veterans Affairs and active military hospitals (they operate with VA and military benefits instead), though there are a few other exceptions nationwide.
What happens when your Medicare runs out?
For days 21–100, Medicare pays all but a daily coinsurance for covered services. You pay a daily coinsurance. For days beyond 100, Medicare pays nothing. You pay the full cost for covered services.
When a patient uses Medicare as their primary insurance company, is the hospital required to choose appropriate and accurate diagnoses that
When a patient uses Medicare as their primary insurance company, the hospital is required to choose appropriate and accurate diagnoses that apply to the patient so that they can bill for the associated care.
What is Medicare insurance?
Medicare insurance is one of the most popular options for those who qualify, and the number of people using this insurance continues to grow as life expectancy continues to increase. Medicare policies come available with many different parts, including Part A, Part B, Part C, and Part D.
How long do you have to pay coinsurance for hospital?
As far as out-of-pocket costs, you will be responsible for paying your deductible, coinsurance payments if your hospital stay is beyond 60 days, and for any care that is not deemed medically necessary. However, the remainder of the costs will be covered by your Medicare plan.
Does Medicare pay flat rate?
This type of payment system is approved by the hospitals and allows Medicare to pay a simple flat rate depending on the specific medical issues a patient presents with and the care they require. In addition, In some cases, Medicare may provide increased or decreased payment to some hospitals based on a few factors.
Does Medicare cover inpatient care?
If you receive care as an inpatient in a hospital, Medicare Part A will help to provide coverage for care. Part A Medicare coverage is responsible for all inpatient care , which may include surgeries and their recovery, hospital stays due to illness or injury, certain tests and procedures, and more. As far as out-of-pocket costs, you will be ...
What is covered by Medicare before a hospital stay?
This coverage includes: general nursing care. a semi-private room. hospital equipment and services. meals. medication that is part of inpatient hospital treatment.
What is Medicare Part A?
Medicare Part A. Out-of-pocket expenses. Length of stay. Eligible facilities. Reducing costs. Summary. Medicare is the federal health insurance program for adults aged 65 and older, as well as for some younger people. Medicare pays for inpatient hospital stays of a certain length. Medicare covers the first 60 days of a hospital stay after ...
What is the best Medicare plan?
We may use a few terms in this piece that can be helpful to understand when selecting the best insurance plan: 1 Deductible: This is an annual amount that a person must spend out of pocket within a certain time period before an insurer starts to fund their treatments. 2 Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%. 3 Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
How much does Medicare pay for skilled nursing in 2020?
Others, who may have long-term cognitive or physical conditions, require ongoing supervision and care. Medicare Part A coverage for care at a skilled nursing facility in 2020 involves: Day 1–20: The patient spends $0 per benefit period after meeting the deductible. Days 21–100: The patient pays $176 per day.
How much is the deductible for Medicare 2020?
This amount changes each year. For 2020, the Medicare Part A deductible is $1,408 for each benefit period.
How long does Medicare cover hospital stays?
Medicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual’s reserve days. Medicare provides 60 lifetime reserve days. The reserve days provide coverage after 90 days, but coinsurance costs still apply.
How long does a psychiatric hospital stay in Medicare?
Medicare provides the same fee structure for general hospital care and psychiatric hospital care, with one exception: It limits the coverage of inpatient psychiatric hospital care to 190 days in a lifetime.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is a health care provider?
Tell your doctor and other. health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. about any changes in your insurance or coverage when you get care.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What does Medicare cover inpatient?
What Inpatient Hospital Costs Does Medicare Cover? As an inpatient at a hospital, your Medicare Part A coverage includes the following: Semi-private rooms. Meals. General nursing. Inpatient treatment drugs. Care as part of a qualifying clinical research study. Other hospital services and supplies.
What is Medicare Supplement Insurance?
Medicare Supplement Insurance plan (Medigap) helps pay for out-of-pocket costs associated with a hospital stay. All Medigap plans offer coverage for the following hospital benefits: Medicare Part A coinsurance and hospital costs. First three pints of blood if needed for a transfusion. Part A hospice care coinsurance or copayment.
What is Medicare Part A?
Medicare Part A covers inpatient hospital stays, as well as skilled nursing care, hospice care and limited home health services. Medicare beneficiaries can expect to meet a deductible before Part A starts paying its share of benefits. A Medicare Supplement (Medigap) plan can help pay for your hospital stays, including costs such as Medicare ...
When will Medicare plan F and C be available?
Important: Plan F and Plan C are not available to beneficiaries who became eligible for Medicare on or after January 1, 2020. Call today to speak with a licensed insurance agent who can help you compare Medigap plans that are available where you live.
Does Medicare Part A cover hospice?
Some Medigap plans may also include coverage for: Coinsurance for skilled nursing facility stay. Medicare Part A deductible. With 10 standardized Medigap plans to choose from in most states, you can find one that meets your needs.
Who pays payroll taxes?
Payroll taxes paid by most employees, employers, and people who are self-employed. Other sources, like these: Income taxes paid on Social Security benefits. Interest earned on the trust fund investments. Medicare Part A premiums from people who aren't eligible for premium-free Part A.
How many people did Medicare cover in 2017?
programs offered by each state. In 2017, Medicare covered over 58 million people. Total expenditures in 2017 were $705.9 billion. This money comes from the Medicare Trust Funds.
What is the CMS?
The Centers for Medicare & Medicaid Services ( CMS) is the federal agency that runs the Medicare Program. CMS is a branch of the. Department Of Health And Human Services (Hhs) The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, ...
What is Medicare Part B?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. and. Medicare Drug Coverage (Part D) Optional benefits for prescription drugs available to all people with Medicare for an additional charge.
What is covered by Part A?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents.
Does Medicare cover home health?
Medicare only covers home health care on a limited basis as ordered by your doctor. , and. hospice. A special way of caring for people who are terminally ill. Hospice care involves a team-oriented approach that addresses the medical, physical, social, emotional, and spiritual needs of the patient.