How does Medicare pay for DME?
Medicare pays for different kinds of DME in different ways. Depending on the type of equipment: You may need to rent the equipment. You may need to buy the equipment. You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare.
Where does JCJC process Medicare DME claims?
JC processes FFS Medicare DME claims for Alabama, Arkansas, Colorado, Florida, Georgia, Louisiana, Mississippi, New Mexico, North Carolina, Oklahoma, Puerto Rico, South Carolina, Tennessee, Texas, U.S. Virgin Islands, Virginia and West Virginia Total Number of Fee-for-Service Beneficiaries: 13,476,262 (as of 9/30/2020)
Does Medicare cover durable medical equipment (DME)?
Durable medical equipment (DME) coverage. Medicare Part B (Medical Insurance) covers Medically necessary DME if your doctor prescribes it for use in your home. DME that Medicare covers includes, but isn't limited to: Blood sugar meters. Blood sugar test strips.
What does DME mean in health care?
Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine. DME if your doctor prescribes it for use in your home. DME that Medicare covers includes, but isn't limited to:
What company processes Medicare claims?
MACs are multi-state, regional contractors responsible for administering both Medicare Part A and Medicare Part B claims. MACs perform many activities including: Process Medicare FFS claims.
What does Medicare administrative contractors do?
Medicare Part B Services. Medicare Administrative Contractors (MACs) regionally manage policy and payment related to reimbursement and act as the fiscal intermediary for Medicare. MACs manage provider claims for payment and establish regional policy guidelines, called Local Coverage Determinations (LCDs).
Who is Dmerc?
DMERCs were the Durable Medical Equipment Regional Carriers. The name change occurred in 2007. Durable Medical Equipment Medicare Administrative Contractors is the current name of the Durable Medical Equipment Regional Carriers. Prior to the DME MAC label, they were also called Medicare A/B contractors.
What is a DME Medicare claim?
covers. medically necessary. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine. DME if your doctor prescribes it for use in your home.
What is the difference between RAC and MAC?
MAC audits are powerful and intrusive procedures that have the potential to lead to serious federal charges for healthcare entities. A Recovery Audit Contractor (“RAC”) reviews claims and identifies overpayments from Medicare so that CMS and other auditors are able to prevent improper payments in the future.
What does a Zone Program Integrity Contractor do?
Zone Program Integrity Contractors (“ZPICs”) are charged with the responsibility of investigating alleged instances of fraud, waste, or abuse by health care providers.
How do I submit a DME claim to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
What does CGS mean in Medicare?
CGS Medicare stands for a Celerian Group Company. The company provides a variety of services for Medicare beneficiaries, healthcare providers, and medical equipment suppliers.
What is the DME MAC?
A Durable Medical Equipment Medicare Administrative Contractor (DME MAC) is a private insurance company that has a contract with Medicare to process durable medical equipment (DME) claims.
Where are Dmepos claims submitted to?
supply patients with durable medical equipment (DME) (e.g., canes, crutches); DMEPOS claims are submitted to DME Medicare administrative contractors (MACs) who are awarded contracts by CMS; each DME MAC covers a specific geographic region of the country and is responsible for processing DMEPOS claims for its specific ...
How do I bill for DME?
Billing for Durable medical equipment servicesVerify the Necessity of the Durable Medical Equipment. ... Credentialing. ... Make sure you have checked the patient's benefits and eligibility for the particular DME or Durable Medical Equipment. ... Make sure you understand the difference between billing out of network and in network.
What place of service is used for DME?
Normally, the correct place of service for DME would be 12 (home).
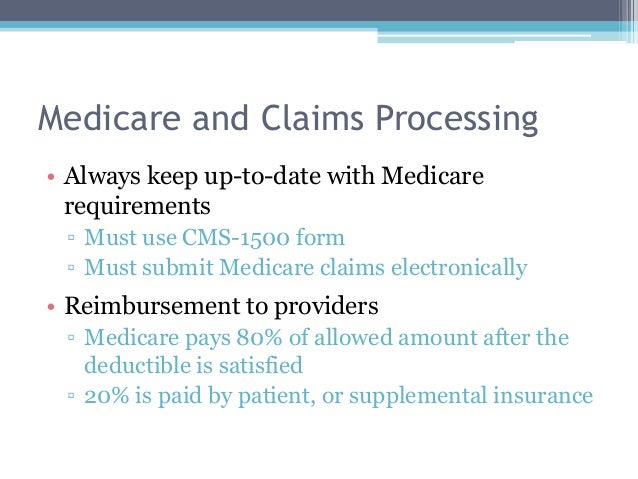
What percentage of Medicare payment does a supplier pay for assignment?
If your supplier accepts Assignment you pay 20% of the Medicare-approved amount, and the Part B Deductible applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment:
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. you pay 20% of the. Medicare-Approved Amount.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
What happens if you live in an area that's been declared a disaster or emergency?
If you live in an area that's been declared a disaster or emergency, the usual rules for your medical care may change for a short time. Learn more about how to replace lost or damaged equipment in a disaster or emergency .
Does Medicare cover DME equipment?
You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare.
DME MAC Jurisdiction D - DME Facts
JD processes FFS Medicare DME claims for Alaska, American Samoa, Arizona, California, Guam, Hawaii, Idaho, Iowa, Kansas, Missouri, Montana, Nebraska, Nevada, North Dakota, Northern Mariana Islands, Oregon, South Dakota, Utah, Washington and Wyoming
Who were the former contractors in this jurisdiction?
Learn about the former contractors in this jurisdiction at Archives: DME MAC Jurisdiction D.
What is the CPM code for DME?
The CPM devices (HCPCS code E0935) are classified as items requiring frequent and substantial servicing and are covered as DME as follows (see the Medicare National Coverage Determinations Manual.):
How long do DME MACs pay rental fees?
For these items of DME, A/B MACs (HHH) and DME MACs pay the fee schedule amounts on a monthly rental basis not to exceed a period of continuous use of 15 months. In the tenth month of rental, the beneficiary is given a purchase option (see §30.5.2). If the purchase option is exercised, A/B MACs (HHH) and DME MACs continue to pay rental fees not to exceed a period of continuous use of 13 months and ownership of the equipment passes to the beneficiary. If the purchase option is not exercised, A/B MACs (HHH) and DME MACs continue to pay rental fees until the 15 month cap is reached and ownership of the equipment remains with the supplier (see §30.5.4). In the case of electric wheelchairs only, the beneficiary must be given a purchase option at the time the equipment is first provided (see §30.5.3).
How to determine liability to a provider other than an HHA?
To determine patient liability to a provider other than an HHA (including nominal charge providers other than a HHA), A/B MACs (A) subtract any unmet deductible from the actual charge and multiply the remainder by 20 percent. The result, plus the unmet deductible is the patient's liability. Coinsurance is applied as applicable.
How to determine Part B payment to nominal charge?
To determine the Part B payment to a nominal charge HHA , A/B MACs (HHH) subtract any unmet Part B deductible from the fee schedule amount and multiply the remainder by
How to determine Part B payment?
To determine the Part B payment to a provider other than nominal charge provider, A/B MACs (A) and (HHH) subtract any unmet Part B deductible from the lower of the actual charge or the fee schedule amount for the item or service and multiply the remainder by
What is an enteral care kit?
Enteral care kits contain all the necessary supplies for the enteral patient using the syringe, gravity, or pump method of nutrient administration. Parenteral nutrition care kits and their components are considered all-inclusive items necessary to administer therapy during a monthly period.
What is PIM in Medicare?
Chapter 5, section 5.2.1 of the Medicare Program Integrity Manual (PIM) states that, in order for Medicare to make payment for an item of Durable Medical Equipment Prosthetic, and Orthotic Supplies (DMEPOS), the DMEPOS supplier must obtain a prescription from the
DME MAC Jurisdiction C - DME Facts
JC processes FFS Medicare DME claims for Alabama, Arkansas, Colorado, Florida, Georgia, Louisiana, Mississippi, New Mexico, North Carolina, Oklahoma, Puerto Rico, South Carolina, Tennessee, Texas, U.S. Virgin Islands, Virginia and West Virginia
Who were the former contractors in this jurisdiction?
Learn about the former contractors in this jurisdiction at Archives: DME MAC Jurisdiction C.
When did Medicare start charging for DME?
Section1834 of the Act requires the use of fee schedules under Medicare Part B for reimbursement of durable medical equipment (DME) and for prosthetic and orthotic devices, beginning January 1 1989. Payment is limited to the lower of the actual charge for the equipment or the fee established.
How long do you have to pay rental fees in DME?
For these items of DME, contractors pay the fee schedule amounts on a monthly rental basis not to exceed a period of continuous use of 15 months. In the tenth month of rental, the beneficiary is given a purchase option (see §30.5.2). If the purchase option is exercised, contractors continue to pay rental fees not to exceed a period of continuous use of 13 months and ownership of the equipment passes to the beneficiary. If the purchase option is not exercised, contractors continue to pay rental fees until the 15 month cap is reached and ownership of the equipment remains with the supplier (see §30.5.4). In the case of electric wheelchairs only, the beneficiary must be given a purchase option at the time the equipment is first provided (see §30.5.3).
How to complete CMS-382?
The beneficiary must complete Form CMS-382 to choose either Method I or Method II dialysis. Method I dialysis patients receive their home dialysis equipment and supplies from a dialysis facility. Method II patients choose to deal with a home dialysis supplier that is not a dialysis facility. Once a beneficiary has made a method selection choice, the beneficiary or dialysis facility submits the Form CMS-382 to the appropriate intermediary. The intermediary then processes information from the form to CWF. See Chapter 8 for instructions for completing the form.
What is an enteral care kit?
Enteral care kits contain all the necessary supplies for the enteral patient using the syringe, gravity, or pump method of nutrient administration. Parenteral nutrition care kits and their components are considered all-inclusive items necessary to administer therapy during a monthly period.
How long does a beneficiary have to change suppliers?
If the beneficiary changes suppliers during or after the 15-month rental period, this does not result in a new rental episode. For example, if the beneficiary changes suppliers after his 8th rental month, the new supplier is entitled to the monthly rental fee for seven additional months (15 - 8). The supplier that provides the item in the 15th month of the rental period is responsible for supplying the equipment and for maintenance and servicing after the 15-month period (see §40.2).
How long does a patient have to rent equipment?
patient rents an item of equipment for 12 months and is then institutionalized for 45 days. Upon his discharge from the institution, the patient resumes use of the equipment and is considered to be in his 13th month of rental (since the period of institutionalization is not counted) for purposes of calculating the 15-month rental period. Moreover, for the period he was institutionalized, no payment is made for the item of equipment. If the supplier desires, it may pick up the item of equipment during the patient's hospitalization but is required to return the item upon the patient's return home.
Do you need to submit additional documentation to a beneficiary?
There must be no requirement for suppliers to submit additional documentation to describe a beneficiary's medical condition and functional abilities when the supplier bills for a higher level of equipment than previously supplied.
What is Medicare DME audit?
Medicare DME claims audits help to ensure all claims submitted are accurate and correctly paid. If you receive an audit request, make sure you respond by the deadline, send all the requested documents, and begin reviewing the audited claim internally.
What is a DME billing company?
A DME billing company, like Medbill, can become an extension of your billing department and can provide you with numerous services from A/R to audit assistance to revenue cycle management.
What is outsourcing DME billing?
Outsourcing DME billing services can provide you access to DME billing specialists. Those specialists can process claims, check on claim status, stay current on all payor guidelines, and more. Outsourcing billing services can free up extra time to be sent on marketing or bringing in new business.
What is a DME billing specialist?
A DME billing specialist’s goal is to ensure all submitted claims are accurate and contain all the required paperwork to reduce the number of rejected claims. They have several responsibilities, including ensuring compliance with payors guidelines, checking and correcting HCPCS codes, submitting and following up on claims, and more.
Does DME change?
DME payor medical policies often change across the various product lines. Make sure to have a system in place to stay current on all changes before submitting a claim. Regularly checking the CMS’s website is an efficient way to keep up to date on all Medicare and Medicaid DME guidelines.
4 Steps on How to Bill DME Claims
The following steps will go through the typical DME billing process once a patient places an order to claim submission.
Learn More About Billing DME Claims
Many reliable resources are available to help you learn more about how to bill DME claims. Below are a few articles and websites that will help you with submitting claims.
