When should I use Medicare adjustment claims?
Use when the original claim shows Medicare on the secondary payer line and now the adjustment claim shows Medicare on the primary payer line. Use when there is a change to the revenue codes, HCPCS code, RUG code, or HIPPS code.
Will Medicare pay for my diagnosis codes?
Any tests ordered must also be linked to the diagnosis code. This information is then directed to your insurance company, Medicare included, so your healthcare provider gets paid for their service. If your healthcare provider does not pick the right diagnosis code, it is possible your insurance plan will not pay for the care you received.
What is a place of service code in healthcare?
Place of Service Codes Place of Service Codes are two-digit codes placed on health care professional claims to indicate the setting in which a service was provided. The Centers for Medicare & Medicaid Services (CMS) maintain POS codes used throughout the health care industry.
When to use a condition code for Medicare claims?
Use when canceling a claim to correct the Medicare ID or provider number. Condition code only applicable on a xx8 type of bill. D6: Use when canceling a claim for reasons other than the Medicare ID or provider number. Use when canceling a claim to repay a payment. Condition code only applicable to a xx8 type of bill. D1
Who determines medical coding?
the American Medical Association (AMA)This code set is published and maintained by the American Medical Association (AMA). These codes are copyrighted by the AMA and are updated annually. CPT codes are five-digit numeric codes that are divided into three categories.
Who audits the coding of Medicare patient records?
One of the primary tasks of the SMRCs is to conduct nationwide medical review as directed by CMS. SMRCs will evaluate medical records and related documents to determine whether Medicare claims were billed in compliance with coverage, coding, payment and billing guidelines.
Who process Medicare claims?
Office of Medicare Hearings and Appeals (OMHA) - The Office of Medicare Hearings and Appeals is responsible for level 3 of the Medicare claims appeal process and certain Medicare entitlement appeals and Part B premium appeals.
What person assigns revenue codes to the medical record?
Note: The Medical "Biller" is the person who enters these codes. This code is used for accounting purposes to distribute revenue to appropriate location. This code is an internally assigned unique number identifying each item listed.
What is a coding auditor?
What Is a Coding Auditor? A coding auditor reviews and evaluates medical coding to ensure the accuracy of patient records and billing.
Who in the medical practice is ultimately responsible for proper documentation and correct coding?
Ultimately, the physician is responsible for proper documentation and correct coding. Possible consequences of inaccurate coding and incorrect billing are denied claims/reduced payments, prison sentences, and/or fines.
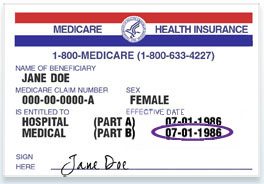
How do providers submit claims to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
What is a CMS contractor?
The Centers for Medicare & Medicaid Services (CMS) employs contractors to provide a wide range of services and makes data available to these contractors as needed to support their assigned work. A CMS Data Use Agreement (DUA) is used to create a traceable record of what data is being accessed by each CMS contractor.
What does a Zone Program Integrity Contractor do?
The Zone Program Integrity Contractor (ZPIC) is an entity established in the United States by the Centers for Medicare & Medicaid Services (CMS) to combat fraud, waste and abuse in the Medicare program.
Who is responsible department for ensuring compliance with billing and coding policies?
The Office Staff These are vital parts of the medical billing process and can results in systemic mistakes in the coding and billing process if done wrong.
What is the difference between and insurance billing specialist and a medical coder?
Billers work with patients. Medical coders work behind the scenes in collaboration with physicians, billers and other staff. Medical billers must communicate with patients.
What is the difference between and insurance billing specialist and a medical coder if any?
Medical coding involves extracting billable information from the medical record and clinical documentation, while medical billing uses those codes to create insurance claims and bills for patients.
What is a place of service code?
Place of Service Codes are two-digit codes placed on health care professional claims to indicate the setting in which a service was provided. The Centers for Medicare & Medicaid Services (CMS) maintain POS codes used throughout the health care industry.
What is HIPAA standard?
HIPAA directed the Secretary of HHS to adopt national standards for electronic transactions. These standard transactions require all health plans and providers to use standard code sets to populate data elements in each transaction.
What happens if a claim is incomplete?
If a claim is submitted with incomplete or invalid information, it may be returned to the submitter as unprocessable. See Chapter 1 for definitions and instructions concerning the handling of incomplete or invalid claims.
Can a physician choose a primary specialty code?
Physicians are allowed to choose a primary and a secondary specialty code. If the A/B MAC (B) and DME MAC provider file can accommodate only one specialty code, the A/B MAC (B) or DME MAC assigns the code that corresponds to the greater amount of allowed charges. For example, if the practice is 50 percent ophthalmology and 50 percent otolaryngology, the A/B MAC (B)/DME MAC compares the total allowed charges for the previous year for ophthalmology and otolaryngology services. They assign the code that corresponds to the greater amount of the allowed charges.
When did CMS standardize reason codes?
In 2015 CMS began to standardize the reason codes and statements for certain services. As a result, providers experience more continuity and claim denials are easier to understand.
What does CMS review?
CMS contractors medically review some claims (and prior authorizations) to ensure that payment is billed (or authorization requested) only for services that meet all Medicare rules.
What happens if your doctor doesn't pick the right diagnosis code?
If your doctor does not pick the right diagnosis code, it is possible your insurance plan will not pay for the care you received. That leaves you paying not only a copay or coinsurance for the test or visit but the full dollar amount.
Why is it important to standardize diagnosis codes?
Standardizing diagnosis codes improves the ability to track health initiatives, monitor health trends, and respond to health threats. 1. The World Health Organization released ICD-10 in 1999. The United States, however, was slow to adopt the most recent codes and did not transition from ICD-9 to ICD-10 until October 2015.
How many ICD-10 codes are there for rhinitis?
Allergic rhinitis (a runny nose from allergies) has at least six different codes from which to choose, pneumonia 20 codes, asthma 15 codes, influenza 5 codes, sinusitis 21 codes, and sore throat 7 codes. 5 Those are the easy ones.
Can ICD-10 codes be changed?
It is possible they have used the wrong ICD-10 code. Your doctor may be able to change the diagnosis code to one that gives you the coverage you need. If ICD-10 coding is not the reason for the billing issue, you may need to make an appeal with your insurance company.