What makes a person eligible for Medicare Part B?
Does everyone automatically get Medicare Part B?
Is Medicare Part B based on income?
Can you get denied for Medicare Part B?
Are you automatically enrolled in Medicare Part A when you turn 65?
How do you pay for Medicare Part B if you are not collecting Social Security?
What is deducted from your monthly Social Security check?
Are Medicare Part B premiums going up in 2021?
What is the Medicare Part B deductible for 2021?
The standard monthly premium for Medicare Part B enrollees will be $170.10 for 2022, an increase of $21.60 from $148.50 in 2021. The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.Nov 12, 2021
Why did I get denied for Medicare?
What happens if I opt out of Medicare Part B?
Do I need Medicare Part D if I don't take any drugs?
Do you have to pay Part A and Part B?
Also enroll in or already have Part B. To keep premium Part A, the person must continue to pay all monthly premiums and stay enrolled in Part B. This means that the person must pay both the premiums for Part B and premium Part A timely to keep this coverage. Premium Part A coverage begins prospectively, based on the enrollment period ...
What is Medicare Part A?
Medicare Part A counts as minimum essential coverage and satisfies the law that requires people to have health coverage. For additional information about minimum essential coverage (MEC) for people with Medicare, go to our Medicare & Marketplace page.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
What is MEC in Medicare?
Medicare and Minimum Essential Coverage (MEC) Medicare Part A counts as minimum essential coverage and satisfies the law that requires people to have health coverage. For additional information about minimum essential coverage (MEC) for people with Medicare, go to our Medicare & Marketplace page.
How long does Part A coverage last?
If the application is filed more than 6 months after turning age 65, Part A coverage will be retroactive for 6 months. NOTE: For an individual whose 65th birthday is on the first day of the month, Part A coverage begins on the first day of the month preceding their birth month.
When does Part A start?
NOTE: For an individual whose 65th birthday is on the first day of the month, Part A coverage begins on the first day of the month preceding their birth month. For example, if an individual's birthday is on December 1, Part A begins on November 1.
How old do you have to be to get Medicare Part B?
Age is the most common way that a person qualifies for Medicare Part B. A person becomes eligible if they are: 65 years old. a United States citizen. an immigrant lawfully admitted for permanent residence in the United States without a break for 5 years before a person applies for Medicare enrollment.
What is Medicare Part A?
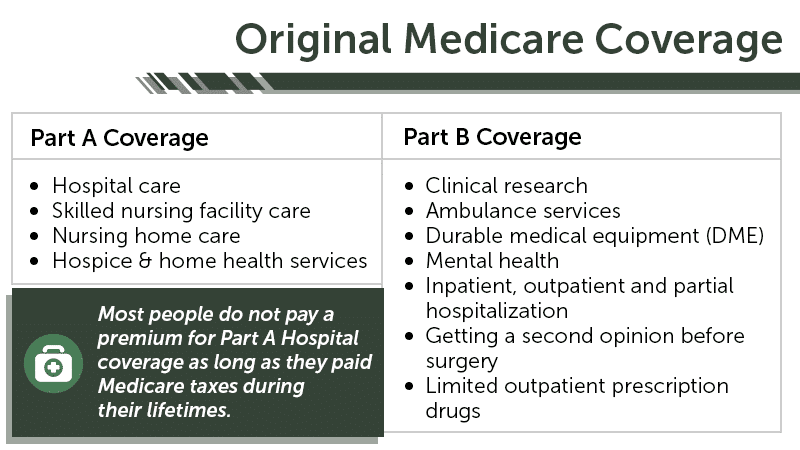
Medicare Part A covers hospital-related costs, such as those for a hospital stay or admission to a rehabilitation or skilled nursing facility when a person is recovering from surgery, illness, or injury.
How to apply for medicare online?
A person can enroll with Medicare by: 1 visiting a local Social Security office 2 calling the Social Security Administration at 800-772-1213 (TTY: 800-325-0778) 3 applying online at the Social Security Administration’s website
What is a SEP for Medicare?
When a person stops working, and their employer’s insurance no longer covers them, they can usually qualify for a Special Enrollment Period (SEP) where they can sign up for Medicare Part B.
When does the IEP start?
The IEP is the 7-month period that begins 3 months before a person turns 65 years old. If a person does not enroll with Medicare Part B during their IEP, they may be required to wait until the General Enrollment Period (GEP), from January 1 to March 31.
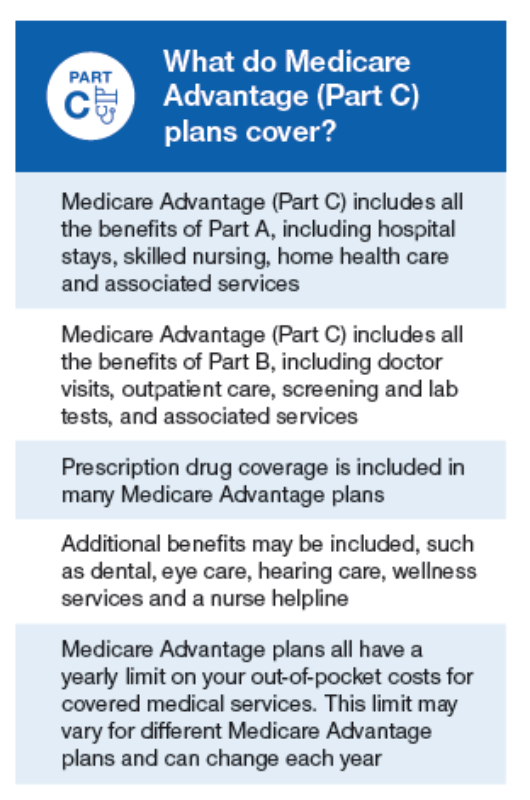
What is Part B?
Part B covers 2 types of services. Medically necessary services: Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice. Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best.
What are the factors that determine Medicare coverage?
Medicare coverage is based on 3 main factors 1 Federal and state laws. 2 National coverage decisions made by Medicare about whether something is covered. 3 Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
What is medically necessary?
Medically necessary services: Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice. Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best.
What is preventive care?
Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best. You pay nothing for most preventive services if you get the services from a health care provider who accepts. assignment.
What does Medicare Part B cover?
Medicare Part B helps cover medical services like doctors' services, outpatient care, and other medical services that Part A doesn't cover. Part B is optional. Part B helps pay for covered medical services and items when they are medically necessary. Part B also covers some preventive services like exams, lab tests, ...
What is Part B insurance?
Part B also covers some preventive services like exams, lab tests, and screening shots to help prevent, find, or manage a medical problem. Cost: If you have Part B, you pay a Part B premium each month. Most people will pay the standard premium amount.
How long can you delay Part B?
You can delay your Part B effective date up to three months if you enroll while you still have employer-sponsored coverage or within one month after that coverage ends. Otherwise, your Part B coverage will begin the month after you enroll.
What is a SEP for Medicare?
What is the Medicare Part B Special Enrollment Period (SEP)? The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse’s current job. You usually have 8 months from when employment ends to enroll in Part B. Coverage that isn’t through a current job – such as COBRA benefits, ...
Who is Josh Schultz?
Josh Schultz has a strong background in Medicare and the Affordable Care Act. He coordinated a Medicare ombudsman contract at the Medicare Rights Center in New York City, and represented clients in extensive Medicare claims and appeals.
Do you have to pay a premium for Medicare Part B?
Although most people have to pay a premium to be eligible to receive Medicare Part B benefits, there are programs that can help reduce or cover the cost depending on your circumstances. Enter your zip code above to receive private Medicare quotes for your state!
Is Medicare Part B free?
Medicare Part B is very rarely “free”, there are monthly premiums most people have to pay for their Medicare Part B coverage. There are several programs that can help to reduce the cost of your Medicare Part B premium and even cover the cost entirely.
What is a qualified Medicare beneficiary?
Qualified Medicare Beneficiary. The first program that can help reduce your costs is the Qualified Medicare Beneficiary (QMB). There are two requirements to be eligible for this program, which include the income limit and asset limit. If you meet both of these requirements and are eligible for the program, your state should pay your premiums, ...
What is QMB in Medicare?
The first program that can help reduce your costs is the Qualified Medicare Beneficiary (QMB). There are two requirements to be eligible for this program, which include the income limit and asset limit. If you meet both of these requirements and are eligible for the program, your state should pay your premiums, deductibles, ...
How much does Medicare Part B cost?
The standard premium amount for Medicare Part B is $144.60. You may pay a higher premium amount if your income is higher than $85,000 as an individual and $170,000 as a couple.
What is the asset limit for QMB?
In addition to the income limit, there is an asset limit you must meet in order to be eligible for the QMB program. The asset limit is approximately $7000 for an individual and $11,000 for a couple that is married.