Who Runs Medicare and Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Who really pays for Medicaid?
The Centers for Medicare & Medicaid Services (CMS) is the federal agency that runs the Medicare Program. CMS is a branch of the. Department Of Health And Human Services (Hhs) The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, and the Children’s Health Insurance …
Is Medicaid and Medicare the same thing?
The Centers for Medicare and Medicaid Services (CMS) provides health coverage to more than 100 million people through Medicare, Medicaid, the Children’s Health Insurance Program, and the Health Insurance Marketplace. The CMS seeks to strengthen and modernize the Nation’s health care system, to provide access to high quality care and improved health at lower costs.
What's the difference between Medicare and Medicaid?
Medicare is a federal program. It is basically the same everywhere in the United States and is run by the Centers for Medicare & Medicaid Services, an agency of the federal government. For more information regarding Medicare and its components, please go to http://www.medicare.gov. Medicaid. Medicaid is an assistance program.
Who administers funds for Medicare?
The federal government runs the Medicare program. Each state runs its own Medicaid program. That’s why Medicare is basically the same all over the country, but Medicaid programs differ from state to state. The Centers for Medicare and Medicaid Services, part of the federal government, runs the Medicare program.
See more
Mar 10, 2022 · The program is run by the federal Centers for Medicare & Medicaid Services (CMS). Medicare is a fee-for-service health plan. This means that every treatment, procedure, test, and doctor visit has its own price tag and is paid for separately.
Who oversees Medicare and Medicaid payments?
Is Medicare funded by the federal government?
What is the largest third party payer?
Who controls Medicare?
Who is the head of Medicare?
Who is the largest payer for healthcare in the US?
Who is the largest health insurer in the US?
Is Medicare a third-party payer?
Who Gets Medicare vs Medicaid?
Elderly and disabled people get Medicare; poor people get Medicaid. If you’re both elderly and poor or disabled and poor, you can potentially get b...
Who Runs Medicare vs Medicaid?
The federal government runs the Medicare Program. Each state runs its own Medicaid program. That’s why Medicare is basically the same all over the...
How Do Program Designs Differ For Medicare vs Medicaid?
Medicare is an insurance program while Medicaid is a social welfare program.Medicare recipients get Medicare because they paid for it through payro...
How Are Medicare and Medicaid Options Different?
The Medicare program is designed to give Medicare recipients multiple coverage options. Medicare is composed of several different sub-parts, each o...
Where Do Medicare and Medicaid Get Their Money?
Medicare is funded in part by the Medicare payroll tax, in part by Medicare recipients’ premiums, and in part by general federal taxes. The Medicar...
How Do Medicare and Medicaid Benefits differ?
Medicare and Medicaid don’t necessarily cover the same healthcare services. For example, Medicare doesn’t pay for long-term custodial care like per...
Is Medicare a federal program?
Small monthly premiums are required for non-hospital coverage. Medicare is a federal program. It is basically the same everywhere in the United States and is run by the Centers for Medicare & Medicaid Services, an agency of the federal government.
What is Medicare insurance?
Medicare. Medicare is an insurance program. Medical bills are paid from trust funds which those covered have paid into. It serves people over 65 primarily, whatever their income; and serves younger disabled people and dialysis patients. Patients pay part of costs through deductibles for hospital and other costs.
How is Medicare funded?
Medicare is funded: In part by the Medicare payroll tax (part of the Federal Insurance Contributions Act or FICA) In part by Medicare recipients’ premiums. In part by general federal taxes. The Medicare payroll taxes and premiums go into the Medicare Trust Fund.
What is the difference between medicaid and medicare?
Essentially, Medicare is for people who are over age 65 or have a disability, while Medicaid is for people with low incomes. Some people are eligible for both .
How long do you have to be on Social Security to qualify for Medicare?
In most cases, you have to receive Social Security disability benefits for two years before you become eligible for Medicare (but there are exceptions for people with end-stage renal disease and amyotrophic lateral sclerosis). 2 . You’re eligible for Medicare if: You’re at least 65 years old.
How old do you have to be to get Medicare?
You’re eligible for Medicare if: You’re at least 65 years old. AND you or your spouse paid Medicare payroll taxes for at least 10 years. Whether you're rich or poor doesn't matter; if you paid your payroll taxes and you're old enough, you'll get Medicare. In that case, you'll get Medicare Part A for free.
How much is Medicare Part B?
For most people, Medicare Part B premiums are $148.50 a month (in 2021 rates). However, you'll pay higher premiums for Medicare Part B and Part D if your income is higher than $87,000 per year for a single person, or $174,000 per year for a married couple. 3 .
Is Medicare a social welfare program?
Medicare is an insurance program while Medicaid is a social welfare program. Medicare recipients get Medicare because they paid for it through payroll taxes while they were working, and through monthly premiums once they’re enrolled.
What is Medicare program?
The Medicare program is designed to give Medicare recipients multiple coverage options. It's composed of several different sub-parts, each of which provides insurance for a different type of healthcare service.
Does each state have its own Medicaid program?
While Congress and the Centers for Medicare and Medicaid Services (CMS) set out the general rules under which Medicaid operates , each state runs its own program. Under certain circumstances, an applicant may be denied coverage. As a result, the eligibility rules differ significantly from state to state, although all states must follow the same basic framework.
Is Medicaid a federal program?
Medicaid is a program that is not solely funded at the federal level. States provide up to half of the funding for Medicaid. In some states, counties also contribute funds. Unlike Medicare, Medicaid is a means-tested, needs-based social welfare or social protection program rather than a social insurance program.
What is Medicaid eligibility?
Medicaid eligibility policies are very complicated. In general, a person's Medicaid eligibility is linked to their eligibility for Aid to Families with Dependent Children (AFDC), which provides aid to children whose families have low or no income, and to the Supplemental Security Income (SSI) program for the aged, blind and disabled. States are required under federal law to provide all AFDC and SSI recipients with Medicaid coverage. Because eligibility for AFDC and SSI essentially guarantees Medicaid coverage, examining eligibility/coverage differences per state in AFDC and SSI is an accurate way to assess Medicaid differences as well. SSI coverage is largely consistent by state, and requirements on how to qualify or what benefits are provided are standard. However AFDC has differing eligibility standards that depend on: 1 The Low-Income Wage Rate: State welfare programs base the level of assistance they provide on some concept of what is minimally necessary. 2 Perceived Incentive for Welfare Migration. Not only do social norms within the state affect its determination of AFDC payment levels, but regional norms will affect a state's perception of need as well.
What is the difference between medicaid and medicare?
The main difference between the two programs is that Medicaid covers healthcare costs for people with low incomes while Medicare provides health coverage for the elderly.
What is managed care in Medicaid?
Under managed care, Medicaid recipients are enrolled in a private health plan, which receives a fixed monthly premium from the state . The health plan is then responsible for providing for all or most of the recipient's healthcare needs. Today, all but a few states use managed care to provide coverage to a significant proportion of Medicaid enrollees. As of 2014, 26 states have contracts with managed care organizations (MCOs) to deliver long-term care for the elderly and individuals with disabilities. The states pay a monthly capitated rate per member to the MCOs, which in turn provide comprehensive care and accept the risk of managing total costs. Nationwide, roughly 80% of Medicaid enrollees are enrolled in managed care plans. Core eligibility groups of low-income families are most likely to be enrolled in managed care, while the "aged" and "disabled" eligibility groups more often remain in traditional " fee for service " Medicaid.
How many states have not expanded Medicaid?
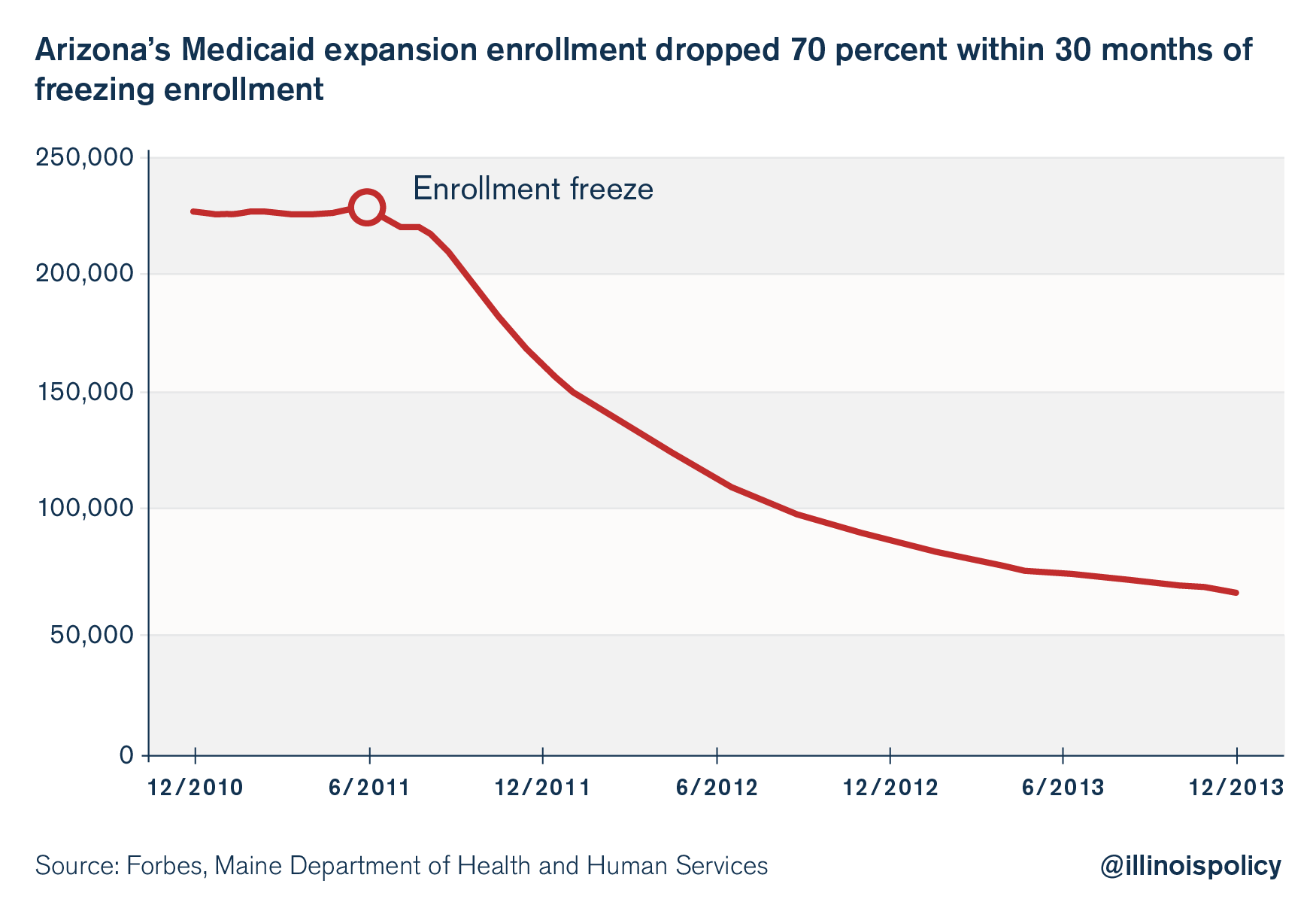
Of the 14 states with uninsured rates of 10% or greater, 11 had not expanded Medicaid. A July 2019 study by the National Bureau of Economic Research (NBER) indicated that states enacting Medicaid expansion exhibited statistically significant reductions in mortality rates.
Does Medicaid bundle with other programs?
States may bundle together the administration of Medicaid with other programs such as the Children's Health Insurance Program (CHIP), so the same organization that handles Medicaid in a state may also manage the additional programs. Separate programs may also exist in some localities that are funded by the states or their political subdivisions to provide health coverage for indigents and minors.
Is Medicare part of Medicaid?
Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance).
What is medicaid?
Medicaid is a joint federal and state program that: 1 Helps with medical costs for some people with limited income and resources 2 Offers benefits not normally covered by Medicare, like nursing home care and personal care services
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Does Medicare cover prescription drugs?
. Medicaid may still cover some drugs and other care that Medicare doesn’t cover.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
What is CAHPG in Medicaid?
The Children & Adults Health Programs Group (CAHPG) houses the Center’s children and adult-focused Medicaid work, including eligibility, enrollment and outreach activities, section 1115 demonstrations, and federal leadership of CHIP and BHP. CAHPG plays a leading role in working with states on the implementation of the Affordable Care Act’s Medicaid eligibility expansion to provide health coverage to low-income adults. The group leads CMCS’ efforts to improve the quality of health care provided through Medicaid and CHIP. CAHPG also manages the agency’s relationships with Indian tribes and tribal providers and coordinates policy development affecting the American Indian/Alaska Native community.
What is CMCS in healthcare?
The Center for Medicaid and CHIP Services (CMCS) is organized into seven groups that are responsible for the various components of policy development and operations for Medicaid, the Children’s Health Insurance Program (CHIP), and the Basic Health Program (BHP). CMCS also has an Innovation Accelerator Program ...
What is the FMG?
The Financial Management Group (FMG) is responsible for Medicaid and CHIP financing issues, including program oversight and operations, review and approval of states’ reimbursement rates, section 1115 waiver negotiations, and work with states on new financing initiatives such as payment and delivery system reform and efforts to improve access to care while lowering costs.
What is the Operations Services Group?
The Operations Services Group (OSG) manages internal operations including budget and acquisitions, human capital and other administrative processes within the Center for Medicaid and CHIP Services.
