Who should receive the notice? Only individuals eligible for Medicare Part D have to receive the notice. However, most employers send the notice to all participants since they may not always know if someone is eligible for Part D (for example, a dependent who may be eligible because of disability).
Full Answer
What is the deadline for Medicare Part D?
Aug 05, 2021 · Only individuals eligible for Medicare Part D have to receive the notice. However, most employers send the notice to all participants since they may not always know if someone is eligible for Part D (for example, a dependent who may be eligible because of disability).
What are the rules of Medicare Part D?
Aug 25, 2020 · Medicare Part D Notice. The Medicare Modernization Act requires all employers to provide written notice to Medicare-eligible individuals to notify those individuals on whether their plan provides prescription drug coverage that is “creditable,” or “as good as,” Medicare Part D coverage. This allows individuals to make an informed decision about whether to remain on an …
Who is eligible for Medicare Part D?
Oct 07, 2020 · In order for CMS to have an official record of an employer’s or union’s status as creditable or non-creditable, employers must disclose that status both to their Medicare Part D eligible employees as well as the CMS. Employers should work with their group health plan sponsors to send this notice, and it must be done by October 15 th.
What are the requirements for Medicare Part D?
Sep 01, 2020 · As a general rule, a single Medicare Part D notice may be provided to the covered Medicare beneficiary and all of his or her Medicare eligible dependent(s). However, if a plan sponsor knows that any Medicare-eligible spouse or dependent lives at a different address, it must send a separate notice to the Medicare-eligible spouse or dependent at that address.

What is Medicare Part D notice?
Medicare Part D Notice. The Medicare Modernization Act requires all employers to provide written notice to Medicare-eligible individuals to notify those individuals on whether their plan provides prescription drug coverage that is “creditable,” or “as good as,” Medica re Part D coverage. This allows individuals to make an informed decision about ...
When do employers have to distribute Medicare Part D?
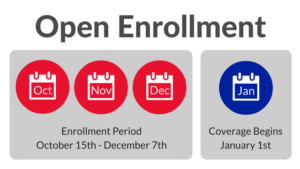
Employers must distribute the Medicare Part D Notice to plan participants annually prior to October 15th.
When is Medicare Part D non-creditable?
Employers should ensure their Medicare Part D Creditable or Non-Creditable Disclosure Notice has been distributed to all plan participants prior to October 15th. Employers who have already distributed the Notice do not need to distribute it again.
When is Medicare Part D notice?
Medicare Part D Notices – An Overview for Employers. Employers and their group health plan sponsors will want to mark October 15, 2020 on their calendars. This is the deadline for plan sponsors to disclose to individuals who are eligible for Medicare Part D and to the Centers for Medicare and Medicaid Services ...
What is a Part D notice?
Part D Notices, or notices of “Creditable Coverage,” are simply an official document given to an employee from their employer (or union) that states whether their prescription drug coverage plan is equal to or better than the prescription drug coverage provided through Medicare. The purposes of these notices is to help beneficiaries of the plan make the best decision for their prescription health coverage moving forward.
What is CMS notice?
The Centers for Medicare and Medicaid Services (CMS) provide sample notices that employers should consider using. Employers should work with their group health plan sponsors to ensure that these notices are delivered at the right time – which might end up being more frequently than you think.
What is creditable coverage?
What Exactly Does “Creditable Coverage” Mean, and How Is It Related to Medicare Part D? “Creditable Coverage” is a term that involves two simple words, but most people have a hard time understanding what exactly it means in the world of Medicare.
What is a Medicare Part D notice?
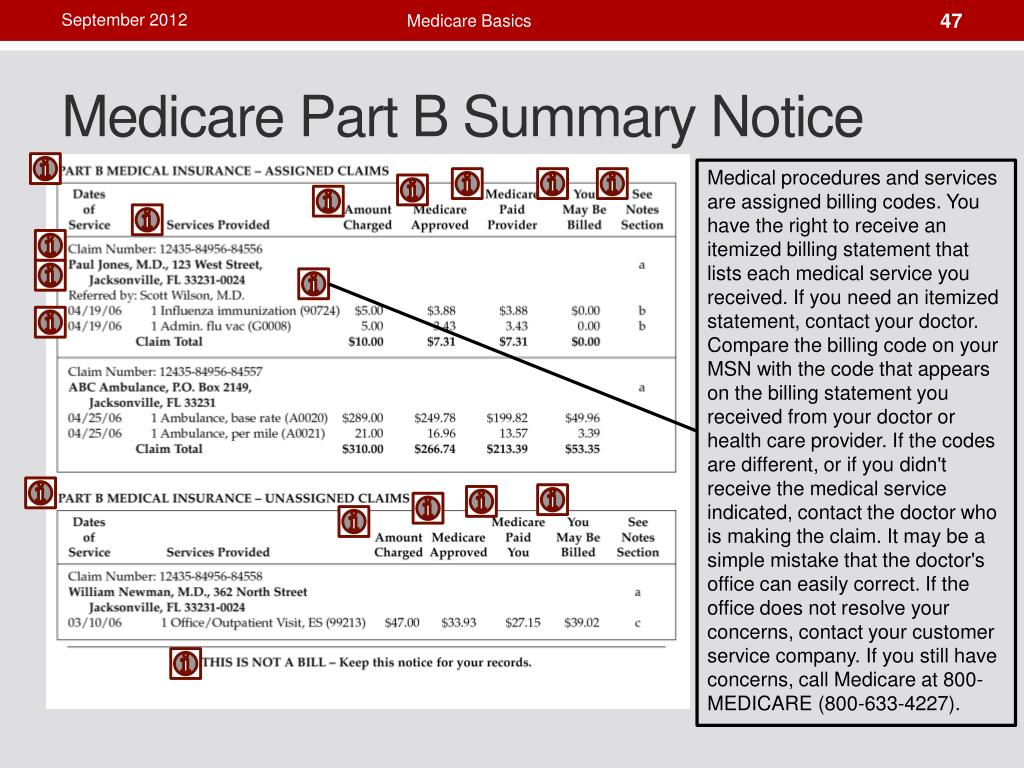
The Medicare Part D notice is utilized to inform individuals about the plan’s prescription drug coverage status for the next calendar year. A “Medicare Part D eligible individual” is an individual who: is entitled to Medicare Part A and/or enrolled in Part B as of the effective date of coverage under a Part D plan; and.
Who is eligible for Medicare Part D?
Medicare Part D eligible individuals could include active employees, disabled employees, COBRA participants, retirees, as well as their covered spouses and dependents. Because employers do not generally know the Medicare eligibility status of dependents, distributing the notice to all employees who are eligible to participate in ...
What is creditable coverage?
Creditable coverage is prescription drug coverage that is actuarially equal to or greater than the prescription drug coverage provided under Medicare Part D – Medicare’s voluntary prescription drug program. Knowing a prescription drug plan’s creditable status is crucial to an individual’s decision of whether to enroll in a Medicare Part D ...
When does Medicare enroll?
In order for Medicare-eligible individuals to make informed and timely enrollment decisions, group health plan sponsors must disclose the status (creditable or non-creditable) of the plan’s prescription drug coverage prior to the start of annual Medicare enrollment which begins October 15 each year.
Is Medicare coverage creditable?
This approach ensures that Medicare-eligible individuals are notified in a timely fashion that their prescription drug coverage for the next calendar year is creditable or non-creditable.