Can Medicare refuse to cover a drug?
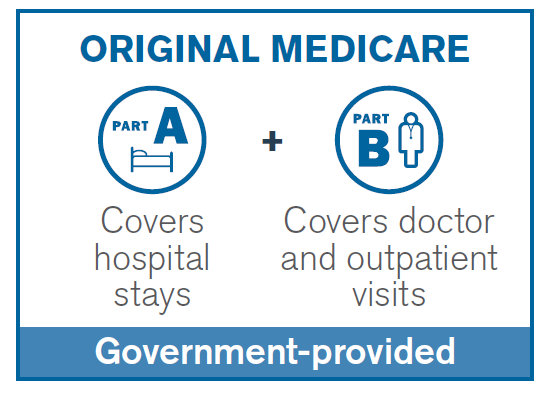
Plans cannot cover drugs that are not approved by the FDA. For example, dessciated thyroid is an unapproved drug and a Part D plan cannot cover it. If Medicare Part A, hospital insurance, or Part B, medical insurance, covers a medication, a Part D drug plan cannot.
Why do some insurances not cover certain medications?
When your insurance company won't cover a medicine, it may be because the medicine is not on the insurance plan's "formulary," or list of medicines covered by the plan. Below are tips to help you gain access to the medicine that is best suited for your health needs.
What if my prescription is not covered?
If you have a prescription that is not covered, talk to your doctor about other options. Your plan may cover a generic or lower cost option. Remember, generic versions have the same key ingredients and work just as well as their brand-name equivalents.
Why would an insurance company not cover a prescription?
Your health insurance plan's Pharmacy & Therapeutics Committee might exclude a drug from its drug formulary a few common reasons: The health plan wants you to use a different drug in that same therapeutic class. The drug is available over-the-counter. The drug hasn't been approved by the U.S. FDA or is experimental.
When a drug is not on a patient's insurance formulary What will the prescriber have to do to get the medication paid for by the insurance?
If you need a drug that is not on your health plan's formulary, you must get your plan's approval or pay for the drug yourself. Your doctor should ask the plan for approval.
What happens when the claim for a medication is rejected by the insurance company?
First-Level Appeal—This is the first step in the process. You or your doctor contact your insurance company and request that they reconsider the denial. Your doctor may also request to speak with the medical reviewer of the insurance plan as part of a “peer-to-peer insurance review” in order to challenge the decision.
Can insurance deny prescriptions?
An insurance company may deny payment for a prescription, even when it was ordered by a licensed physician. This may be because they believe they do not have enough evidence to support the need for the medication.
What is stand alone prescription drug plans?
A PDP is often referred to as a “stand-alone prescription drug plan” because it is separate prescription drug coverage that Medicare beneficiaries can purchase – through private insurers – usually to supplement Original Medicare.
Can I use GoodRx with insurance?
Keep in mind that you cannot use GoodRx and insurance at the same time. However, you can use GoodRx instead of insurance or government-funded programs, such as Medicare or Medicaid, to pay for your prescription medications. GoodRx is not insurance.
Who is eligible to use Express Scripts?
Who can use our pharmacy? Express Scripts® Pharmacy is available to those with pharmacy benefits from Express Scripts and other participating pharmacy benefit managers. In the future, non-members will be able to use the pharmacy.
How do I get a prior authorization for medication?
How Does Prior Authorization Work?Call your physician and ensure they have received a call from the pharmacy.Ask the physician (or his staff) how long it will take them to fill out the necessary forms.Call your insurance company and see if they need you to fill out any forms.More items...•