If you’re among the 7.5 million people in the Qualified Medicare Beneficiary (QMB) Program, doctors, suppliers, and other providers should not bill you for services and items covered by Medicare, including deductibles, coinsurance, and copayments. If a provider asks you to pay, that’s against the law.
What is a Medicare a deductible?
A deductible is the amount you must pay out of pocket before the benefits of the health insurance policy begin to pay. Medicare copayments and coinsurance can be broken down by each part of Original Medicare (Part A and Part B).
What is the Medicare Part B deductible for doctors?
You must meet this deductible before Medicare pays for any Part B services. Unlike the Part A deductible, Part B only requires you to pay one deductible per year, no matter how often you see the doctor. After your Part B deductible is met, you typically pay 20 percent of the Medicare-approved amount for most doctor services.
What happens if my insurance company doesn't pay Medicare?
If the insurance company doesn't pay the Claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should've made. How Medicare coordinates with other coverage.
Can a doctor Bill you for something that is not covered?
If you’re among the 7.5 million people in the Qualified Medicare Beneficiary (QMB) Program , doctors, suppliers, and other providers should not bill you for services and items covered by Medicare, including deductibles, coinsurance, and copayments. If a provider asks you to pay, that’s against the law.
Who pays Medicare deductible?
Medicaid may pay your Medicare deductibles and coinsurance. Employer coverage over 20 employees: If your employer has 20 or more employees, the employer group health plan usually is the primary insurance and Medicare is the secondary insurance. Your group health plan may pay your Medicare deductibles.
Who would not be covered under Medicare?
Some of the items and services Medicare doesn't cover include:Long-Term Care. ... Most dental care.Eye exams related to prescribing glasses.Dentures.Cosmetic surgery.Acupuncture.Hearing aids and exams for fitting them.Routine foot care.
How does Medicare deductible get paid?
Typically, you'll pay a 20% coinsurance once you reach your Part B deductible. This coinsurance gets attached to every item or service Part B covers for the rest of the calendar year. In this instance, you'd be responsible for 20% of the bill under Part B. Medicare would then cover the other 80%.
Can a doctor collect Medicare deductible upfront?
Yes, we could collect the payment but it has to be refunded promptly if you are collecting excess payment or collected incorrectly.
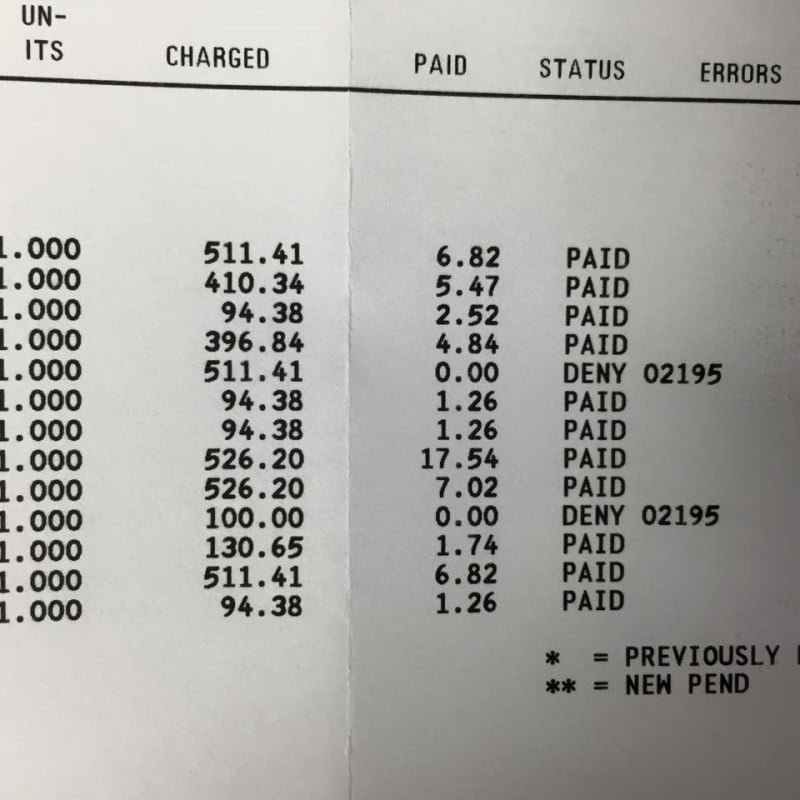
Why would Medicare deny a claim?
A claim that is denied contains information that was complete and valid enough to process the claim but was not paid or applied to the beneficiary's deductible and coinsurance because of Medicare policies or issues with the information that was provided.
Can we bill Medicare patients for non covered services?
Under Medicare rules, it may be possible for a physician to bill the patient for services that Medicare does not cover. If a patient requests a service that Medicare does not consider medically reasonable and necessary, the payer's website should be checked for coverage information on the service.
Does Medicare cover deductible from primary insurance?
“Medicare pays secondary to other insurance (including paying in the deductible) in situations where the other insurance is primary to Medicare.
How do you pay the Medicare Part B deductible?
3:045:04How Do You Pay the Part B Deductible? - YouTubeYouTubeStart of suggested clipEnd of suggested clipItself you just pay the first 233. Dollars of your first part me medical care in that year. ThisMoreItself you just pay the first 233. Dollars of your first part me medical care in that year. This means you pay that deductible to a medical provider.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
Do deductibles have to be paid upfront?
A health insurance deductible is a specified amount or capped limit you must pay first before your insurance will begin paying your medical costs. For example, if you have a $1000 deductible, you must first pay $1000 out of pocket before your insurance will cover any of the expenses from a medical visit.
How do I know if my Medicare deductible has been met?
Deductibles for Original Medicare You can find out if you've met your Medicare Part A or Part B deductible for the year at MyMedicare.gov.
How do you collect a patient's deductible?
6 tips for collecting co-pays and deductibles from patientsAssign the responsibility to office staff.Consider the patient experience.Avoid open-ended questions.Ask for immediate payment.Offer payment options.Maintain open communication.
What is the Medicare Deductible for 2022?
A deductible refers to the amount of money you must pay out of pocket for covered healthcare services before your health insurance plan starts to p...
Does Original Medicare Have Deductibles?
Original Medicare is composed of Medicare Part A and Medicare Part B. Both parts of Original Medicare have deductibles you will have to pay out of...
Do You Have to Pay a Deductible with Medicare?
You’ve probably heard the one about death and taxes. If you have Original Medicare, you can add deductibles to that list.
Key Takeaways
Parts A and B of Original Medicare have deductibles you must meet before Medicare will pay for healthcare.
What is the Medicare Deductible for 2022?
A deductible refers to the amount of money you must pay out of pocket for covered healthcare services before your health insurance plan starts to pay. A deductible can be based upon a calendar year, upon a plan year or — as is unique to Medicare Part A — upon a benefit period.
Does Original Medicare Have Deductibles?
Original Medicare is composed of Medicare Part A and Medicare Part B. Both parts of Original Medicare have deductibles you will have to pay out of pocket before your plan starts to pay for your healthcare.
Medicare Advantage (Part C) Deductibles
Medicare Advantage (Part C) is an alternative type of Medicare plan that is purchased through a private insurer. Not every Part C plan is available throughout the country. Your state, county and zip code will determine which plans are available for you to choose from in your area.
Medicare Part D Deductibles
Medicare Part D is prescription drug coverage. People are often surprised to learn that Part D is not included in Original Medicare. This is understandable since prescription medications are very often integral to health.
Medicare Supplement Plan Deductible Coverage
Medicare Supplement Insurance is also known as Medigap. Medigap is supplemental insurance sold by private insurers. It is designed to fill in the cost “gaps” for people who have Original Medicare.
Do You Have to Pay a Deductible with Medicare?
You’ve probably heard the one about death and taxes. If you have Original Medicare, you can add deductibles to that list.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What happens when there is more than one payer?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) to pay. In some rare cases, there may also be a third payer.
Does Medicare pay for group health insurance?
Medicare will pay based on what the group health plan paid, what the group health plan allowed, and what the doctor or health care provider charged on the claim. You'll have to pay any costs Medicare or the group health plan doesn't cover.
What to do if your provider won't stop billing you?
If the medical provider won’t stop billing you, call Medicare at 1-800-MEDICARE (1-800-633-4227) . TTY users can call (877) 486-2048 . Medicare can confirm that you’re in the QMB Program. Medicare can also ask your provider to stop billing you, and refund any payments you’ve already made. 3.
Can you get a bill for QMB?
If you’re in the QMB Program and get a bill for charges Medicare covers: 1. Tell your provider or the debt collector that you're in the QMB Program and can’t be charged for Medicare deductibles, coinsurance, and copayments.
Is Medicare billed for QMB?
The Centers for Medicare & Medicaid Services (CMS) has heard from people with Medicare who report being billed for covered services, even though they’re in the QMB program.
What happens if you don't pay your deductible?
If you have to pay your deductible right now but you don’t have the money, your predicament is tougher. If you don’t come up with a way to pay, your care may be delayed or you might not be able to get the care you need. Here are some possible options.
How long does it take to pay a medical deductible?
You’ll still end up paying the entire $3,000 deductible before your health insurance begins to pay. But, with the cheaper treatment, you’ll spread that deductible over eight months rather than five months, making it easier to manage.
How much is the average deductible for health insurance?
The vast majority of employer-sponsored health plans require members to pay a deductible. Among these workers' plans, the average individual deductible was $1,655 in 2019.
What to do if you can't pay for chemo?
If you can't get you your next round of chemotherapy because you can’t pay your health insurance deductible, then it’s time to think about how to raise the funds. Start by considering selling off valuable but unnecessary things like your jewelry, bicycle, surfboard, iPod, or motor scooter.
Can you owe more than one deductible?
You may owe your deductible to more than one healthcare provider. For example, if you see the doctor and he or she orders blood tests, you’d owe part of your deductible to your doctor and part of it to the blood test lab. This means negotiating two payment plans, not one.
Does switching to a less expensive treatment make your deductible smaller?
While switching to a less expensive treatment option won’t make your deductible any smaller, the deductible will come due over a longer period of time and in smaller chunks. For example, if you have a $3,000 deductible and are getting a treatment costing $700 per month, switching to a treatment costing $400 per month will lower your monthly ...
Can a doctor waive a deductible?
While your doctor can’t waive or discount your deductible because that would violate the rules of your health plan, he or she may be willing to allow you to pay the deductible you owe over time. Be honest and explain your situation upfront to your doctor or hospital billing department.
What percentage of Medicare deductible is paid?
After your Part B deductible is met, you typically pay 20 percent of the Medicare-approved amount for most doctor services. This 20 percent is known as your Medicare Part B coinsurance (mentioned in the section above).
How much is the deductible for Medicare 2021?
If you became eligible for Medicare. + Read more. 1 Plans F and G offer high-deductible plans that each have an annual deductible of $2,370 in 2021. Once the annual deductible is met, the plan pays 100% of covered services for the rest of the year.
What is a copay in Medicare?
A copay is your share of a medical bill after the insurance provider has contributed its financial portion. Medicare copays (also called copayments) most often come in the form of a flat-fee and typically kick in after a deductible is met. A deductible is the amount you must pay out of pocket before the benefits of the health insurance policy begin ...
How much is Medicare coinsurance for days 91?
For hospital and mental health facility stays, the first 60 days require no Medicare coinsurance. Days 91 and beyond come with a $742 per day coinsurance for a total of 60 “lifetime reserve" days.
How much is Medicare Part B deductible for 2021?
The Medicare Part B deductible in 2021 is $203 per year. You must meet this deductible before Medicare pays for any Part B services. Unlike the Part A deductible, Part B only requires you to pay one deductible per year, no matter how often you see the doctor. After your Part B deductible is met, you typically pay 20 percent ...
How much is Medicare Part A 2021?
The Medicare Part A deductible in 2021 is $1,484 per benefit period. You must meet this deductible before Medicare pays for any Part A services in each benefit period. Medicare Part A benefit periods are based on how long you've been discharged from the hospital.
What is Medicare approved amount?
The Medicare-approved amount is the maximum amount that a doctor or other health care provider can be paid by Medicare. Some screenings and other preventive services covered by Part B do not require any Medicare copays or coinsurance.
What is deductible insurance?
A deductible is the amount the client pays out of pocket for eligible medical services before their insurance plan starts to pay toward their medical costs. You will still need to submit claims to the payer so that they can apply the services toward the client's deductible but that is as far as your responsibility goes.
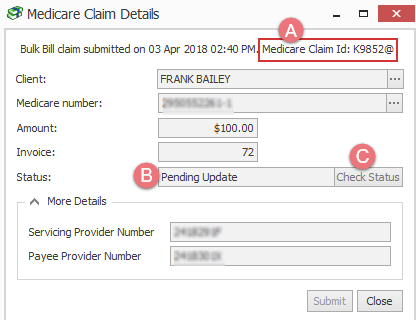
Does SimplePractice automatically record insurance payments?
Note: If you receive a payment report for a claim that was applied to the client's deductible, SimplePractice won't automatically record the $0 insurance payment.
Can you pay an out of network provider a full appointment fee?
Option 2: Since you're an out-of-network provider, you're not bound by a contracted or allowable amount by the payer and your clients pay you your full appointment fee when the deductible isn’t met.
When did Medicare start?
When Medicare began in 1966 , it was the primary payer for all claims except for those covered by Workers' Compensation, Federal Black Lung benefits, and Veteran’s Administration (VA) benefits.
Why is Medicare conditional?
Medicare makes this conditional payment so that the beneficiary won’t have to use his own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is made. Federal law takes precedence over state laws and private contracts.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
How long does ESRD last on Medicare?
Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD.
What age is Medicare?
Retiree Health Plans. Individual is age 65 or older and has an employer retirement plan: Medicare pays Primary, Retiree coverage pays secondary. 6. No-fault Insurance and Liability Insurance. Individual is entitled to Medicare and was in an accident or other situation where no-fault or liability insurance is involved.
Does GHP pay for Medicare?
GHP pays Primary, Medicare pays secondary. Individual is age 65 or older, is self-employed and covered by a GHP through current employment or spouse’s current employment AND the employer has 20 or more employees (or at least one employer is a multi-employer group that employs 20 or more individuals): GHP pays Primary, Medicare pays secondary.
Is GHP a disability?
Disability and Employer GHP: Individual is disabled, is covered by a GHP through his or her own current employment (or through a family member’s current employment) AND the employer has 100 or more employees (or at least one employer is a multi-employer group that employs 100 or more individuals) GHP pays Primary, Medicare pays secondary.
What is an ABN in Medicare?
reimbursed by Medicare and may be billed to the patient. An ABN must: (1) be in writing; (2) be obtained prior to the beneficiary receiving the. service; (3) clearly identify the particular service; (4) state that the provider believes.
Can Medicare patients be billed for services that are not covered?
Billing Medicare Patients for Services Which May Be Denied. Medicare patients may be billed for services that are clearly not covered. For example, routine physicals or screening tests such as total cholesterol are not covered when there is. no indication that the test is medically necessary. However, when a Medicare carrier is.
Can Medicare patients get waivers?
waivers for all Medicare patients are not allowed. Since both LMRPs as well as the new NCD for A1c include frequency limits, an ABN is. appropriate any time the possibility exists that the frequency of testing may be in excess of. stated policy.
Can Medicare deny payment?
However, when a Medicare carrier is. likely to deny payment because of medical necessity policy (either as stated in their written. Medical Review Policy or upon examination of individual claims) the patient must be. informed and consent to pay for the service before it is performed. Otherwise, the patient.
How much is 42.21 approved for Medicare?
You tell the billing department that Medicare approved 42.21 for the service them receiving the 80% of $33. You are paying the difference of 8.44 the balance Medicare says you owe. (or not if supplimental picks up then u say that). You tell them you are not paying more than Medicare approved.
Is 20% based on Medicare?
Explain that doctor is billing you more than approved amount. 20% is not based on the amount charged but the approved amount by Medicare. I think someone in the billing department has made a mistake. If the estate has no money, the bill can't be paid.
