CMS expressly prohibits providers from using the Advance Beneficiary Notice (ABN) or similar notices for Medicare Advantage members. Therefore, the Member Consent for Financial Responsibility for Unreferred/Non-covered Services form shall not be used for Medicare Advantage members.
Can a Medicare provider issue an ABN to a patient?
Medicare does not allow for a provider to issue an ABN to their patients as a matter of routine. The provider has to make reasonable steps to determine if a service or item will most likely be denied.
Should My Medicare patients sign an advance beneficiary notice?
Yes! When applicable, your Medicare patients should always sign an Advance Beneficiary Notice (form CMS-R-131). An ABN is not used for commercial insurance companies. What Is An ABN? An ABN is a Medicare waiver of liability that providers are required to give a Medicare patient for services provided that may not be covered or considered
What is a Medicare advanced beneficiary note of non-coverage (ABN)?
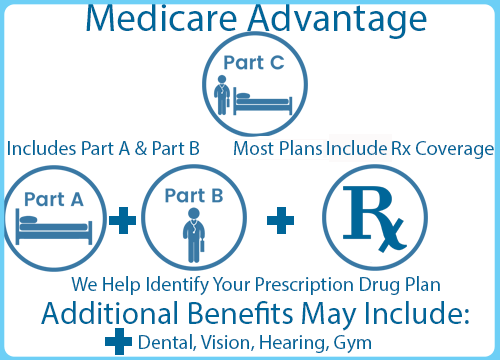
That is when a Medicare Advanced Beneficiary Note of Non-coverage (ABN) Form CMS-R-131 can come in handy. This form is used for people on traditional Medicare (Part A and Part B) but not for people on Medicare Advantage plans (Part C). The ABN may help you win a Medicare appeal and avoid unnecessary billing.

Can you use an ABN for Medicare Advantage plans?
The Original Medicare program uses ABNs — sometimes called “waivers.” But you can't use them for patients in Aetna® Medicare Advantage plans, since the Centers for Medicare & Medicaid Services (CMS) prohibits them.
Why would a Medicare patient be asked to sign an Advance beneficiary Notice of Non Coverage?
The Advance Beneficiary Notice helps patients decide whether to get the item or service Medicare may not cover and accept financial responsibility. If you don't provide the patient with required written notices, Medicare may hold you financially liable if they deny payment.
Does a patient have to sign an ABN?
An ABN is an informed consent document that informs the patient they may be financially liable for the costs should their insurance carrier deny the claim. The ABN must be completed and signed by the patient BEFORE you provide services or items that are not covered by insurance.
When should an ABN not be issued?
If the provider does not have a reasonable belief that the service or item that is normally payable will be denied than an ABN is prohibited from being issued. Other circumstances were you are prohibited from issuing an ABN include: To make a beneficiary liable for Medically Unlikely Edit (MUE) denials.
Do Medicare patients have to sign an ABN?
The ABN must be given to the patient prior to any provided service or procedure. If there is no signed ABN then you cannot bill the patient and it must be written off if denied by Medicare.
What happens if a patient refuses to sign an ABN?
If you refuse to sign, one of two actions will take place: Mayo Clinic may decide not to provide the items or services. A second person will witness your refusal to sign the agreement, and you will receive the items or services.
Who is not eligible for an ABN?
Not everyone is entitled to an ABN. To be entitled to an ABN you must be carrying on a business in Australia. This means that you must have started trading or have undertaken business-like activities towards the commencement of trading.
Is an ABN required when Medicare is secondary?
You may also use the ABN as an optional (voluntary) notice to alert beneficiaries of their financial liability prior to providing care that Medicare never covers. ABN issuance is not required to bill a beneficiary for an item or service that is not a Medicare benefit and never covered.
What is an ABN form and under what circumstances should one be given to a Medicare patient?
The Advance Beneficiary Notice of Noncoverage (ABN), Form CMS-R-131, is issued by providers (including independent laboratories, home health agencies, and hospices), physicians, practitioners, and suppliers to Original Medicare (fee for service - FFS) beneficiaries in situations where Medicare payment is expected to be ...
What is not a mandatory reason for issuing an ABN?
[14] Hospice providers are not required to issue an ABN unless they administer services billable to hospice, and (a) the beneficiary is not determined to be terminally ill, (b) separately billed specific items are not medically necessary, or (c) the level of hospice care for terminal illness and/or related conditions ...
Is an ABN form only for Medicare?
The ABN, or Advance Beneficiary Notice, is a form that is intended for only for Medicare beneficiaries – not Medicare advantage plans or Medicare part C, just true Medicare.
Can an ABN be signed electronically?
Can we show our Medicare patients an electronic version of an advance beneficiary notice (ABN), when needed, and capture their signature digitally? A. Yes, Medicare allows the use of electronic ABNs.
Does Your Medicare Patient Need to Sign An Advance Beneficiary Notice (ABN) Cms-R-131?
Yes! When applicable, your Medicare patients should always sign an Advance Beneficiary Notice (form CMS-R-131). An ABN is not used for commercial i...
Abns Also Protect Your Patient
An ABN notifies Medicare that the patient acknowledges that certain procedures were provided. 1. It also gives the patient the opportunity to accep...
Modifiers Required When Billing With An ABN
Any procedures provided that require an ABN must be submitted with one of the following Medicare modifiers: 1. GA Modifier: Waiver of Liability Sta...
What is an ABN in Medicare?
An ABN is a Medicare waiver of liability that providers are required to give a Medicare patient for services provided that may not be covered or considered. medically necessary. An ABN is used when service (s) provided may not be reimbursed by Medicare. If the healthcare provider believes that Medicare will not pay for some or all ...
What happens if you don't sign an ABN?
If there is no signed ABN then you cannot bill the patient and it must be written off if denied by Medicare.
What is an ABN for a primary care provider?
Examples of services that require an ABN include a visual field exam for an ophthalmologist, a pelvic exam for a primary care provider, or an echocardiogram. These exams should be covered as long as they ...
Why is Medicare ABN important?
The Medicare ABN becomes especially important when a screening test becomes diagnostic. Generally speaking, screening tests are used to look for disease in someone who does not have symptoms while diagnostic tests are performed when someone has symptoms or otherwise has an abnormal finding.
When you are liable to pay with a Medicare ABN, what is the ABN?
When You Are Liable to Pay with a Medicare ABN. At first glance, it may sound as if the Medicare ABN protects medical providers more than beneficiaries. After all, it is a tool to assure that they get paid. However, it is also a tool that can be used to protect you, the patient.
What is an ABN for Medicare?
The Medicare ABN is a form that your medical provider should ask you to sign whenever there is a question about Medicare coverage. If a service is never covered by Medicare, e.g., dentures, eyeglasses, or eyeglasses, an ABN is not appropriate. The form is indicated if Medicare might cover the service. 1 . For example, your doctor may want ...
What happens if a medical office fails to provide an ABN?
If a medical office or supplier fails to provide a Medicare ABN before providing an item or service, you will not be liable to pay if Medicare denies coverage. There are also a number of scenarios, however, where you will not be liable to pay for an item or service even if you did sign an ABN: 4 .
What happens if you don't sign an ABN?
Also, if an ABN is not signed, you cannot make an appeal to Medicare to cover it.
How long do you have to file an appeal for Medicare denial?
9 If you did sign an ABN, you may need to file an appeal with Medicare to get coverage. You must file your appeal within 120 days of the date you received the notice of denial from Medicare.
How to check if Medicare denied a test?
If Medicare denies coverage for certain items, tests, or procedures, you should first check to see if there was a billing error at the medical office. Changing the diagnostic or billing code can sometimes be enough to get coverage approved. 8 Next, you should check to see if you signed a Medicare ABN. Contact your doctor's office and ask for a copy. Make sure it is signed and dated before the service was provided.
What is an ABN in Medicare?
An advance beneficiary notice of noncoverage (ABN) lets you know when Medicare may not cover an item or service. You must respond to an ABN in one of three ways. If a claim has been denied for Medicare coverage, you have the right to appeal the decision.
What does it mean to sign an ABN?
By signing an ABN, you are agreeing to the fees that may come with the items and services you are receiving. You are also accepting responsibility to pay for the item or service, even if Medicare denies the claim and will not reimburse you.
What is an advance benefit notice for skilled nursing?
A skilled nursing facility may send you a Skilled Nursing Facility ABN if there is a chance that your care or a long-term stay in a facility will not be covered by Medicare Part A. This type of ABN may also be issued if your stay is considered custodial care.
What is an ABN?
What is an Advance Beneficiary Notice of Noncoverage (ABN)? An Advance Beneficiary Notice of Noncoverage (ABN) is a liability waiver form that is given when a healthcare provider or medical supply company thinks or knows Medicare will not cover something. An ABN will explain:
How long does it take to appeal a Medicare claim?
If your claim is denied by Medicare, you can file an appeal. Here are a few things you need to know: You must file the appeal within 120 days of receiving your Medicare summary notice, which will have your appeal information on it.
How long does it take to get a decision from Medicare?
Once you have filed an appeal, you should get a decision within 60 days of your request being received.
What to do if you receive an ABN?
If you have received an ABN, you must respond to confirm how you’d like to proceed. There are three different options to choose from: You want to continue receiving the items or services that may not be covered by your Medicare plan.
Questions, comments?
If you have questions or comments about this article please contact us . Comments that provide additional related information may be added here by our Editors.
Latest articles: (any category)
The Department of Justice is pursuing claims of healthcare fraud against Cigna Health-Spring Medicare Advantage plan based on how they used data from their 360 Program in 2012. A review of the allegations may help other payers avoid similar accusations.
What is an ABN in Medicare?
Most of us are familiar with the term ABN and have a general idea of when it should be used, but there are some important rules to remember when working with Medicare-Fee-For-Service patients. Not being adequately informed on these guidelines can lead to costly mistakes for your practice.
What does it mean when a provider is denied an ABN?
If the provider does not have a reasonable belief that the service or item that is normally payable will be denied than an ABN is prohibited from being issued.
What is a GA ABN?
GA – ABN was issued and signed by the beneficiary as required by Medicare (Beneficiary liable) GX – ABN was issued and signed by the beneficiary as voluntary (Beneficiary liable) GY – Indicates that the service is not a benefit of Medicare in any definition (Can be billed in combination with GX if patient signed an ABN. Beneficiary is liable.)
What is the 5 year rule for Medicare?
Note: The 5 year rule includes when an ABN is declined or refused. When the beneficiary signs the form and agrees to proceed with the service or item, you may seek payment from the patient. Keep in mind that if Medicare pays part or all of the service, a prompt refund to the beneficiary will be required. Changes of Mind.
Why is Medicare not paying for an item?
In addition, the reason for denial is because it is not medically reasonable and necessary.
What are the circumstances where you are prohibited from issuing an ABN?
Other circumstances were you are prohibited from issuing an ABN include: To make a beneficiary liable for Medically Unlikely Edit (MUE) denials. To make a beneficiary liable who is under great duress or in a medical emergency. To make a beneficiary liable for a code that was paid as part of a bundle service.
Can a beneficiary refuse to sign a corrected form?
A copy of the corrected form should be given to the beneficiary. In some cases the beneficiary may refuse to select an option or sign the form. If this occurs, the staff members will need to note the refusal to sign or select and list any witness present at the time of refusal.