The Centers for Medicare Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Centers for Medicare and Medicaid Services
The Centers for Medicare & Medicaid Services, previously known as the Health Care Financing Administration, is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state government…
How often are CMS star ratings updated?
CMS’s Overall Hospital Quality Star Rating on Hospital Compare was first displayed in July 2016, and we intend to update the rating twice per year, in July and December. CMS is committed to working with stakeholders in a transparent manner to evaluate and update the Overall Star Rating.
What are star ratings CMS?
Star ratings are compiled annually by the Centers for Medicare and Medicaid Services (CMS). The ratings are helpful for consumers and members to compare Medicare Advantage plans based on overall quality, value and performance. Each rating is based on a five-star scale — with one star meaning “poor” quality, ranging up to five stars for ...
What are the CMS star ratings?
Here's who you can contact if you have questions or want to give feedback:
- Patient Survey Stars & Home Health CAHPS: [email protected] or call 1-866-354-0985
- Quality of Patient Care Star Ratings: [email protected]
- All requests for formal review of Quality of Patient Care Star Ratings including requests to suppress data: [email protected].
What is CMS 5 star rating?
CMS’ Five Star Quality Rating System for Nursing Homes. CMS’ Five Star Quality Rating System for Nursing Homes is a consumer service that offers useful information to the public about the quality of care in the 15,800 nursing homes that participate in the Medicare or Medicaid programs.

Why are Medicare star ratings important?
Medicare star ratings are important because they give you an idea about which plans in your area have the highest satisfaction ratings. Star ratings only pertain to Medicare Advantage and Part D plans. For both types of coverage, the ratings provide a way to compare your plan options beyond their cost.
When was the Medicare star ratings system implemented?
2008The Centers for Medicare and Medicaid Services (CMS) first implemented the star rating system in 2008 as a way to help beneficiaries compare and select Medicare plans.
What is the Medicare star rating?
Medicare uses a Star Rating System to measure how well Medicare Advantage and Part D plans perform. Medicare scores how well plans perform in several categories, including quality of care and customer service. Ratings range from one to five stars, with five being the highest and one being the lowest.
What must all Medicare Advantage sponsors have in place in order to meet CMS compliance guidelines?
Medicare Advantage Plans Must Follow CMS Guidelines In the United States, according to federal law, Part C providers must provide their beneficiaries with all services and supplies that Original Medicare Parts A and B cover. They must also provide any additional benefits proclaimed in their Part C policy.
Who created Medicare Stars program?
CMSCMS created the Five-Star Quality Rating System to help consumers, their families, and caregivers compare nursing homes more easily and to help identify areas about which you may want to ask questions.
How do CMS star ratings work?
Plans are rated on a one-to-five scale, with one star representing poor performance and five stars representing excellent performance. Star Ratings are released annually and reflect the experiences of people enrolled in Medicare Advantage and Part D prescription drug plans.
What does CMS stars stand for?
The Centers for Medicare & Medicaid ServicesThe Centers for Medicare & Medicaid Services (CMS) uses a five-star quality rating system to measure the experiences Medicare beneficiaries have with their health plan and health care system — the Star Rating Program. Health plans are rated on a scale of 1 to 5 stars, with 5 being the highest.
Why are ratings in stars?
Learn about star ratings The greater the number of people leaving feedback, the more reliable a star rating is likely to be as an indicator of (perceived) quality - i.e. of popularity. Different ratings systems vary in the maximum number of stars that can be awarded.
What does CMS do with health plans that receive less than three stars for three years in a row?
On the other end of the scale, if CMS gives a plan fewer than three stars for three years in a row, that plan will be flagged as low-performing.
What are the negatives of a Medicare Advantage plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Does CMS regulate Medicare Advantage plans?
The Centers for Medicare & Medicaid Services (CMS) released a regulation that clarifies the payment of compensation to agents and brokers who enroll beneficiaries in Medicare Advantage and Prescription Drug Plans. Copies of the new regulations and related documents can be downloaded from below.
Does CMS require a compliance program?
The development and implementation of a compliance program is voluntary, but CMS believes that an effective compliance program is a cost-effective investment. It should be noted, however, that CMS is not specifically authorizing funding for any of the recommendations contained in this guidance.
Why do Medicare plans have star ratings?
The star rating system helps consumers identify the best Advantage plans. If a plan is low performing for several years, you have the right to know. Medicare considers the plan low when a plan gets less than three stars for three years in a row.Also, the ratings make it easier to identify the best Part D plans.
Why is Medicare star rating important?
Medicare star ratings are important because it gives you an idea on which plans have a higher satisfaction rating in your area. Also, star ratings have year-round enrollment opportunities. But, these ratings are only for comparison of Part D and Medicare Advantage plans. Either way, the ratings provide a way to consider your plan options ...
What is a star rating in Medicare?
What are Medicare Star Ratings? When Medicare reviews plan performances each year, they give the policies a star-rating. The five-star quality rating system measures the experience other beneficiaries had on the plan. Plans will get a rating between one and five. However, new plans may be too new to determine a rating.
How to compare Medicare plans?
How to Compare Plans Using the Medicare Star Rating System. When you look at your plan options online, you’ll notice ratings for each policy. Plans with higher ratings are policies that work well for past and current beneficiaries. Also, if you’re on the fence about two plans, seeing the score helps you determine the final choice.
What does it mean when your Medicare rating is lower?
Instead, a lower rating simply means that there may be better options available.
What does higher star rating mean?
Higher star ratings mean that a provider has either gone above and beyond the standard or that patient satisfaction is far greater for that provider compared to others.
Medicare Advantage Star Ratings
Medicare Advantage plans receive their overall star rating from the evaluation of five different categories:
Medicare Part D Star Ratings
Medicare prescription drug plans that are a part of a Medicare Advantage plan, or simply a stand-alone prescription drug plan, are evaluated on four categories, rather than five like Medicare Advantage plans are. Medicare prescription drug plans are evaluated on the following issues:
Importance Of Medicare Plan Star Ratings
If you compare Medicare Advantage plans or Medicare prescription drug plans and enroll in one that is four stars or higher, then you are receiving exceptional service via your Medicare plan.
Recap of Significant Changes to Star Ratings
There have been significant changes to the 2022 Star Ratings. There are additional changes anticipated for 2023 reflected below.
Implications for 2022 Star Ratings
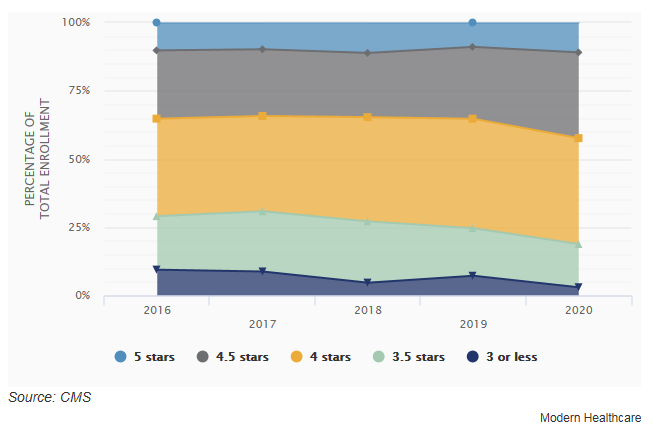
This is a historical high for the number of people enrolled in plans with 4-Stars.
