There is no vaccine for hepatitis Inflammatory condition of the liver.Hepatitis
Full Answer
Does Medicare cover hepatitis C screenings?
If you’re at high risk for contracting hepatitis C — such as if you continue to use injectable drugs — Medicare will cover a yearly screening for hepatitis C. However, you must get the screening test from a medical provider who is enrolled in Medicare and accepts assignment.
How much does a hepatitis C screening test cost?
You pay nothing for the screening test if your doctor or other qualified health care provider accepts Assignment . Medicare will only cover Hepatitis C screening tests if your primary care doctor or other primary care provider orders them.
Will Medicare pay for hepatitis-C drugs?
But it's almost certain that potent new drugs for hep-C could cure him. However, the private insurer that handles his medication coverage for the federal Medicare program has twice refused to pay for the drugs his doctor has prescribed. Doctors are seeing more and more patients approaching the end-stage of hep-C infection.
Can a doctor prescribe medication to treat hepatitis C?
A doctor may also prescribe a medication to help with treatment. Medicare does not cover most of the prescriptions that are used to treat hepatitis C, except in special inpatient and outpatient situations.

How much does a Hep C blood test cost?
How much does a hepatitis C screening cost? Hepatitis C screening is covered by most insurance plans. You may have an out-of-pocket copay. If you don't have insurance, each blood test will cost around $100 or more.
Is hep C test covered?
A screening test is covered for adults at high risk for Hepatitis C Virus infection.
Does Medicare cover lab tests that are medically necessary?
You usually pay nothing for Medicare-covered clinical diagnostic laboratory tests. Diagnostic laboratory tests look for changes in your health and help your doctor diagnose or rule out a suspected illness or condition. Medicare also covers some preventive tests and screenings to help prevent or find a medical problem.
Does medical cover Hep C treatment?
Jerry Brown and state lawmakers have set aside $70 million in next year's budget — which starts July 1 — so that almost all Medi-Cal recipients with hepatitis C will become eligible for the medications, as long as they are at least 13 and have more than one year to live.
What tests are covered by Medicare?
Medicare Part B covers outpatient blood tests ordered by a physician with a medically necessary diagnosis based on Medicare coverage guidelines. Examples would be screening blood tests to diagnose or manage a condition. Medicare Advantage, or Part C, plans also cover blood tests.
What diagnosis code covers hepatitis panel?
ICD-10-CM Diagnosis Code B18 B18.
What blood tests are not covered by Medicare?
Medicare does not cover the costs of some tests done for cosmetic surgery, insurance testing, and several genetic tests. There are also limits on the number of times you can receive a Medicare rebate for some tests. Your private health insurance may pay for diagnostic tests done while you are a patient in hospital.
How often will Medicare pay for a CMP?
every 5 yearsBoth Original Medicare and Medicare Advantage cover a cholesterol screening test every 5 years. Coverage is 100%, which makes the test free of charge.
Does Medicare cover blood work at Labcorp?
Insured Patients Labcorp will file claims directly to Medicare, Medicaid, and many insurance companies and managed care plans. Before you have lab tests performed, please make sure: Your insurance information is up to date. Your insurance company accepts claims from Labcorp.
Does Medicare require hep C test?
Medicare covers a Hepatitis C screening test if your primary care doctor or other qualified health care provider orders one and you meet one or more of these conditions: You're at high risk because you use or have used illicit injection drugs.
How do people afford hep C treatment?
Funding Resources Available to Hep C PatientsPharmaceutical Programs. ... The American Liver Foundation (ALF) ... NeedyMeds. ... Help-4-Hep. ... The HealthWell Foundation. ... The Pharmaceutical Research and Manufacturers of America (PhRMA) ... The Patient Access Network (PAN) Foundation. ... The Patient Advocate Foundation.
Is hep C treatment free?
The cost of hep C treatment varies depending on the type of drug. However, an 8- to 12-week course can range from $54,000 to $95,000 (or higher). For example, the price of a 12-week course of Zepatier can be as much as $54,600, and a 12-week course of Harvoni can cost as much as $94,500.
How many people have hepatitis C?
According to the Centers for Disease Control and Prevention (CDC), an estimated 2.4 million people. Trusted Source.
How many medications are approved for hepatitis C?
The FDA has currently approved seven medications to treat hepatitis C. However, not all of these will appear on a plan’s Part D formulary. Often, only one medication appears on a plan’s list. As a result, your doctor may prescribe medications to you based on what your plan covers.
What is Medicare Part C?
Part C. Medicare Part C is also known as Medicare Advantage. This is a combination Medicare plan where a private insurance company provides your Medicare benefits. Medicare requires that all Advantage plans cover at least the same benefits as original Medicare (parts A and B).
What is a Medigap plan?
Medigap. Medigap, or Medicare supplement insurance, is a plan that helps you reduce out-of-pocket costs if you have original Medicare. While there are different plans available, they generally help pay for costs like coinsurance and premiums for parts A and B, as well as foreign travel emergency care and more.
How long do you have to take hepatitis C medication?
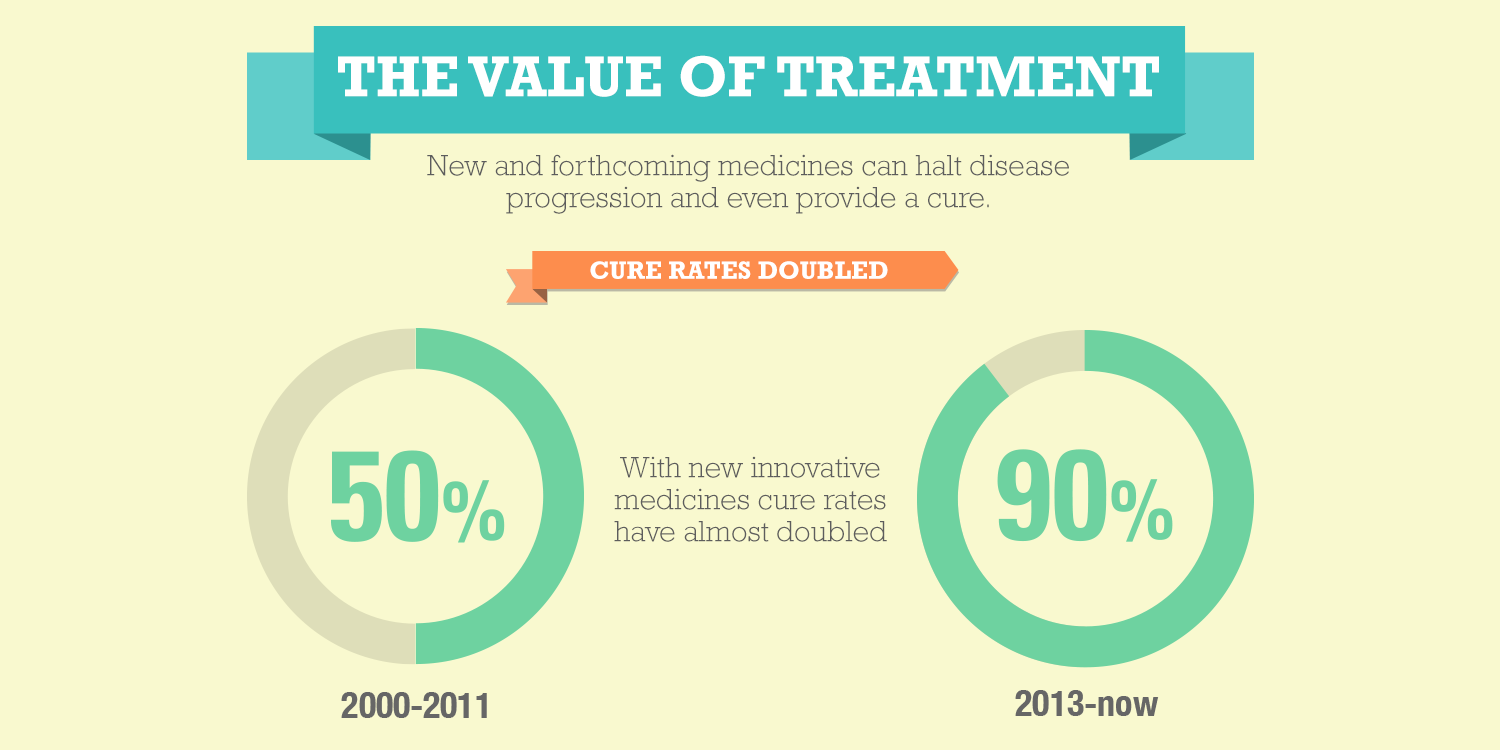
If your doctor diagnoses you with hepatitis C, they’ll usually recommend you take certain medications. You’ll typically take these for about 8 to 12 weeks. The treatment success rate is often high: In about 90 percent.
Does Medicare require a Part D plan?
Medicare requires that all individuals who are eligible for Medicare have a Part D plan or other creditable prescription drug coverage . These plans will usually have a formulary that separates drugs into different tiers based on cost.
Does Medicare cover hepatitis C?
Medicare will cover screenings and some medications to treat hepatitis C.
How many people have hepatitis C?
According to the Centers for Disease Control & Prevention (CDC), over 2 million people live with chronic Hepatitis C. Baby Boomers are five times more likely to contract Hepatitis C.
How long does it take to cure hepatitis C?
Current treatments include oral medication, sometimes called direct-acting antivirals. These medications can be taken for approximately 8-12 weeks with a 90% rate of curing Hepatitis C.
How long does it take for hepatitis C to develop?
Most cases of Hepatitis C develop into a longer and possibly lifelong condition.
Does insurance cover hepatitis C?
Compare plans before enrolling to make sure your insurance will cover the drugs you need to treat Hepatitis C.
Does Medicare cover hepatitis C screening?
Medicare will cover the cost of one screening for Hepatitis C if you meet the following criteria: You are high risk due to illicit injected drugs. You had a blood transfusion before 1992. You were born between 1945 and 1965. If you’re considered high risk, Medicare will cover yearly screenings.
What is hepatitis C?
Hepatitis C is a liver infection that stems from the hepatitis C virus. There are different forms of the virus. The most common form in the United States is type 1.
What is the treatment?
If you have been diagnosed with hepatitis C, it is important to talk to your healthcare provider about what your options are. Since it can vary, so can the treatment options. If your case is mild, you may have coverage under Medicare Part B with outpatient services.
What does Medicare cover?
First, Medicare will only cover Hepatitis C screening tests if your primary care doctor or other primary care provider orders them.
Medications
Medicare requires that all individuals who are eligible for Medicare have a Part D plan or other creditable prescription drug coverage. These plans will usually have a formulary that separates drugs into different tiers based on cost.