
Full Answer
When to choose Original Medicare vs. Medicare Advantage?
You may want to choose between Original Medicare and Medicare Advantage for financial reasons, but you may also want to consider access to certain healthcare services. The important thing is to understand the differences between each type of Medicare before you commit yourself to a plan for the coming year.
Does Medicare Advantage cost less than traditional Medicare?
UnitedHealth Group, for example, discovered that Medicare Advantage costs beneficiaries 40 percent less than traditional Medicare does.
Is Medicare Advantage really to your advantage?
Overwhelming majorities of Medicare beneficiaries in both traditional Medicare and Medicare Advantage were satisfied with their care. The researchers discovered that the Advantage plans didn't substantially improve beneficiaries' health care experiences compared to traditional Medicare, but did offer somewhat more care management.
When will Medicare sequestration end?
Update: President Biden today signed into law legislation that would eliminate the 2% across-the-board cut to all Medicare payments, known as sequestration, until the end of 2021. The legislation also makes several technical changes to the rural health clinic provisions that were included in the Consolidated Appropriations Act, 2021.
Does sequestration apply to Medicare Advantage?
The payment reduction, referred to as sequestration, is applied to the Net Capitation Payment (NCP) made to the plans, including MAOs. Therefore, Medicare rates and fee schedules remain unaffected by sequestration.
Why does Medicare have sequestration?
The sequestration is required by the Budget Control Act that was signed into law in August 2011. It was originally intended as an incentive for the so-called Super Committee convened that year to design an alternative package to achieve $1.2 trillion in budget savings. How will Medicare physician payments be affected?
What does Medicare sequestration apply to?
Q: How long is the 2% reduction to Medicare fee-for-service claim payments in effect? A: The sequestration order covers all payments for services with dates of service or dates of discharge (or a start date for rental equipment or multi-day supplies) on or after April 1, 2013.
What is Medicare sequester adjustment?
According to the Congressional Research Service, sequestration is a reduction in federal spending by a certain percentage. As this applies to Medicare, the reduction in federal spending means providers receive less payment for services, specifically by two percent.
Is Medicare still taking sequestration?
117-7), and the Protecting Medicare and American Farmers from Sequester Cuts Act (P.L. 117-71) also suspended the sequestration of Medicare from May 2020 through March 2022. P.L. 117-7 also limited the Medicare reductions to 1% during April 2022 through June of 2022.
What does sequestration mean in insurance?
(Update March 19, 2013) "Sequestration" is a process of automatic, largely across-the-board spending reductions under which budgetary resources are permanently canceled to enforce certain budget policy goals.
What are Medicare sequestration payments?
Medicare claims with dates-of-service or dates-of-discharge on or after April 1, 2013, incur a 2% reduction in Medicare payment. These are known as Medicare Sequestration Payment Reductions.
Is sequestration still in effect in 2021?
Jun. 3, 2021 Update: Congress has passed legislation that continued the moratorium on sequestration. As a result, CMS has extended the moratorium on sequestration until December 31, 2021.
How is sequestration calculated?
We normally would pay 80% of the approved amount after the deductible is met, which is $40.00 ($50.00 x 80% = $40.00). The patient is responsible for the remaining 20% coinsurance amount of $10.00 ($50.00 – $40.00 = $10.00).
How much is the sequestration adjustment?
Medicare FFS Claims: 2% Payment Adjustment (Sequestration) Changes. The Protecting Medicare and American Farmers from Sequester Cuts Act impacts payments for all Medicare Fee-for-Service (FFS) claims: No payment adjustment through March 31, 2022. 1% payment adjustment April 1 – June 30, 2022.
How long is sequestration supposed to last?
Sequestration usually lasts for about 5-10 years. A sequestration order will last on your credit report for a period of 5 years, or until the rehabilitation order is granted. The rehabilitation order will appear on the credit report for a further 5 years.
The Final Payment Amount is Reduced, Not the Payment Rates
In an April 17, 2014 letter to the American Hospital Association, the Centers for Medicare & Medicaid Services (CMS) clarified the application of the sequestration by Medicare Advantage Organizations (MAO) to reduce payments to providers.
Understanding the Origins of the Discrepancy
The Budget Control Act of 2011 mandated across-the-board budget cuts in federal spending. Congress set the implementation of sequester for March 1, 2013. On that date, President Obama issued a sequestration order to apply to federal agencies, including the Centers for Medicare & Medicaid Services.
CMS Says Payment Terms Are Determined by Contract
The CMS’s April 17th letter reiterates that sequestration does not alter the Medicare FFS fee schedule, as the American Hospital Association asserted.
What Should Providers and Plans Do Now?
CMS recommends that hospitals contact MAOs directly to address discrepancies in payments. Although this is sound business advice, providers and plans may still fail to see eye-to-eye on the application of sequestration to their payment arrangements.
How will sequestration affect Medicare and provider payments?
Under the sequestration order original Medicare provider payments will be cut by 2 percent beginning April 1, 2013, as part of the spending reductions required by the Budget Control Act of 2011.
How will the sequestration affect Medicare?
Sequestration generally applies to original Medicare Part A and Part B payments for services furnished beginning April 1, 2013 (the first day of the first month beginning after the date the sequestration order is issued).
How will sequestration affect Medicare low-income programs?
Low-income subsidies and additional subsidies for Medicare beneficiaries whose spending exceeds catastrophic levels in Prescription Drug Plans are exempt from sequestration.
How will sequestration affect Medicare overall?
Overall, sequestration means that bout 90% of original Medicare spending is limited to 2 percent in cuts, and 8 percent is completely exempt from sequestration.
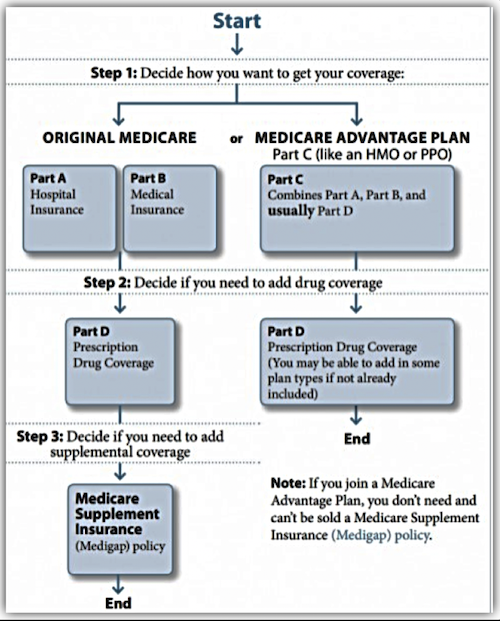
What is Medicare Advantage Plan?
A Medicare Advantage Plan is intended to be an all-in-one alternative to Original Medicare. These plans are offered by private insurance companies that contract with Medicare to provide Part A and Part B benefits, and sometimes Part D (prescriptions). Most plans cover benefits that Original Medicare doesn't offer, such as vision, hearing, ...
What is Medicare Part A?
Original Medicare. Original Medicare includes Part A (hospital insurance) and Part B (medical insurance). To help pay for things that aren't covered by Medicare, you can opt to buy supplemental insurance known as Medigap (or Medicare Supplement Insurance). These policies are offered by private insurers and cover things that Medicare doesn't, ...
What is the Cares Act?
On March 27, 2020, President Trump signed a $2 trillion coronavirus emergency stimulus package, called the CARES (Coronavirus Aid, Relief, and Economic Security) Act, into law. It expands Medicare's ability to cover treatment and services for those affected by COVID-19.
Can you sell a Medigap plan to a new beneficiary?
But as of Jan. 2, 2020, the two plans that cover deductibles—plans C and F— cannot be sold to new Medigap beneficiaries.
Do I have to sign up for Medicare if I am 65?
Coverage Choices for Medicare. If you're older than 65 (or turning 65 in the next three months) and not already getting benefits from Social Security, you have to sign up for Medicare Part A and Part B. It doesn't happen automatically.
Does Medicare cover vision?
Most plans cover benefits that Original Medicare doesn't offer, such as vision, hearing, and dental. You have to sign up for Medicare Part A and Part B before you can enroll in Medicare Advantage Plan.
Does Medicare automatically apply to Social Security?
It doesn't happen automatically. However, if you already get Social Security benefits, you'll get Medicare Part A and Part B automatically when you first become eligible (you don't need to sign up). 4. There are two main ways to get Medicare coverage: Original Medicare. A Medicare Advantage Plan.
How does Medicare pay for Advantage?
Medicare pays Advantage car riers based on a bidding process. The carriers submit their bid based on costs per enrollees for services covered under Original Medicare. These bids are compared to benchmark amounts and will vary from county to county.
Why don't I accept Medicare Advantage?
It really depends on who you ask. If you ask a doctor, they may tell you they don’t accept Medicare Advantage because the carriers make it a hassle to get paid. If you ask your neighbor why Medicare Advantage plans are bad, they may say they were unhappy with how much they had to pay out of pocket when using the benefits.
What is the worst Medicare Advantage plan?
Worst Medicare Advantage Plans. The worst plan for you depends on your needs. Those with a grocery list of doctors may find an HMO policy is a nightmare; however, someone with one doctor could overpay on a PPO policy. The worst plan for you is the plan you don’t analyze.
What happens if the bid is higher than the benchmark amount?
If the bid is higher than the benchmark amount, the enrollee will pay the difference in the form of monthly premiums. This is why some Medicare Advantage plans a free and others have a monthly premium.
Does Medicare Advantage have copays?
Unlike Original Medicare and Med igap, Medicare Advantage plans come with copays. You can expect to pay a copay for every doctor visit, test, and service you receive. Don’t confuse zero-dollar premiums with getting out of paying your Part B premium.
Do people leave Medicare Advantage?
Some healthy people live in prime Medicare Advantage areas, and they prefer to pay as they go; these feelings are justifiable. But at the same time, people do leave Medicare Advantage plans for good reasons.
Does Medicare Advantage have a smaller network?
Medicare Advantage also comes with a much smaller network of doctors compared to Original Medicare and Medigap. Always check your plan’s provider directory before you enroll to confirm ALL your doctors are in the plan’s network.
When did Obama sequester Medicare?
The American Taxpayer Relief Act of 2012 postponed sequestration for 2 months. As required by law, President Obama issued a sequestration order on March 1, 2013. For additional information, please refer to the Mandatory Payment Reductions in the Medicare Fee-for-Service (FFS) Program – “Sequestration”.
When did the 2% sequestration reduction end?
Yes, the 2% sequestration reduction applies to electronic health records and physician quality reporting system incentive payments for a reporting period that ended on or after April 1, 2013.
When will the Sequestration Act be extended?
Sequestration. Act to Prevent Across-the-Board Direct Spending Cuts, and for Other Purposes, signed into law on April 14, 2021, extends the suspension period to December 31, 2021. The Consolidated Appropriations Act, 2021, extended the suspension period to March 31, 2021. The Coronavirus Aid, Relief, and Economic Security (CARES) ...
What adjustments are required for sequestration?
Payment adjustments required under sequestration apply to all claims after determining the Medicare payment including application of the current fee schedule, coinsurance, any applicable deductible, and any applicable Medicare secondary payment adjustments.

The Final Payment Amount Is Reduced, Not The Payment Rates
- In an April 17, 2014 letter to the American Hospital Association, the Centers for Medicare & Medicaid Services (CMS) clarified the application of the sequestration by Medicare Advantage Organizations (MAO) to reduce payments to providers. The CMS letter was drafted in response to a request for clarification by the American Hospital Association, joi...
Understanding The Origins of The Discrepancy
- The Budget Control Act of 2011 mandated across-the-board budget cuts in federal spending. Congress set the implementation of sequester for March 1, 2013. On that date, President Obama issued a sequestration order to apply to federal agencies, including the Centers for Medicare & Medicaid Services. CMS issued a guidance letter the following May that referred providers and …
CMS Says Payment Terms Are Determined by Contract
- The CMS’s April 17th letter reiterates that sequestration does not alter the Medicare FFS fee schedule, as the American Hospital Association asserted. Yet, the CMS took a hands-off approach, stating, “We are prohibited from interfering in the payment arrangements between MAOs and contracted providers.” The federal agency directed MAOs and hospitals to refer to th…
What Should Providers and Plans Do Now?
- CMS recommends that hospitals contact MAOs directly to address discrepancies in payments. Although this is sound business advice, providers and plans may still fail to see eye-to-eye on the application of sequestration to their payment arrangements. MAOs and hospitals should carefully review their contracts, especially in regards to whether Medicare FFS rates are used as a bench…