LCDs A liquid-crystal display (LCD) is a flat-panel display or other electronic visual display that uses the light-modulating properties of liquid crystals. Liquid crystals do not emit light directly.Liquid-crystal display
Full Answer
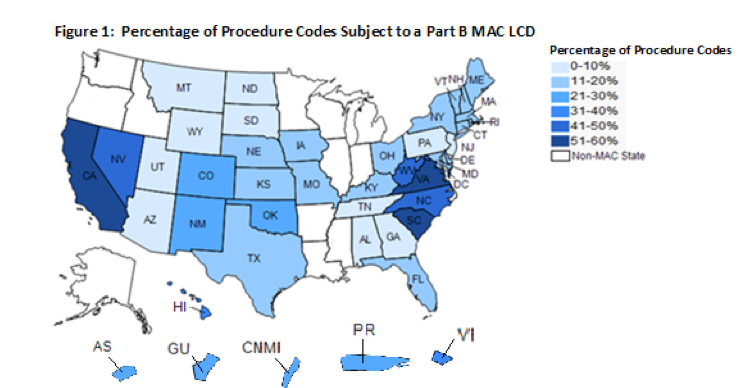
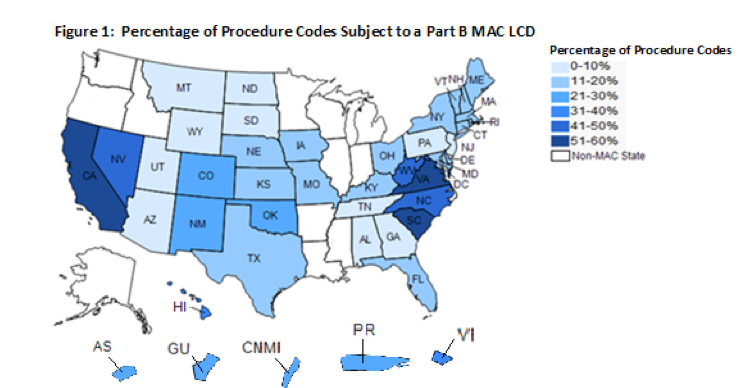
What is an LCD in Medicare?
LCDs are decisions made by a Medicare Administrative Contractor (MAC) whether to cover a particular item or service in a MAC’s jurisdiction (region) in accordance with section 1862 (a) (1) (A) of the Social Security Act. MACs are Medicare contractors that develop LCDs and process Medicare claims.
Why is my LCD not covered by insurance?
It also may include a denial notice that explains that an LCD doesn’t cover a certain item or service. This is because that item or service isn’t considered reasonable and necessary for the diagnosis or treatment of illness or injury, or to improve the function of a malformed part of the body. Where do I file an LCD challenge?
What is an LCD (local coverage determination)?
What is an LCD? Local coverage determinations (LCDS) are defined in Section 1869 (f) (2) (B) of the Social Security Act (the Act).
What is the difference between LCD and NCD?
When a contractor or fiscal intermediary makes a ruling as to whether a service or item can be reimbursed, it is known as a local coverage determination (LCD). When CMS makes a decision in response to a direct request as to whether a service or item may be covered, it’s known as a national coverage determination (NCD).
Why does LCD not cover service?
This is because that item or service isn’t considered reasonable and necessary for the diagnosis or treatment of illness or injury, or to improve the function of a malformed part of the body.
What is part A of a LCD?
You can challenge an LCD if both of these apply: Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. , or both.
When can I file an LCD challenge?
If you haven’t gotten the item or service, you must file your request within 6 months of the date of the treating doctor's written statement that you need to get that item or service.
What is MAC in Medicare?
MACs are Medicare contractors that develop LCDs and process Medicare claims. The MAC’s decision is based on whether the service or item is considered reasonable and necessary.
What is a local coverage determination?
What’s a "Local Coverage Determination" (LCD)? LCDs are decisions made by a Medicare Administrative Contractor (MAC) whether to cover a particular item or service in a MAC’s jurisdiction (region) in accordance with section 1862 (a) (1) (A) of the Social Security Act. MACs are Medicare contractors that develop LCDs and process Medicare claims.
What is a written statement on a LCD?
A written statement from the doctor treating you explaining that you need the item or service. The statement should include any clinical or scientific information that supports why the LCD should be revised or no longer used.
What is Medicare Part B?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. , or both. You need the item (s) or service (s) determined not covered by the LCD.
What is a LCD for Medicare?
Secondly, what is a LCD for Medicare? A local coverage determination (LCD) is a decision made by a Medicare Administrative Contractor (MAC) on whether a particular service or item is reasonable and necessary, and therefore covered by Medicare within the specific region that the MAC oversees.
What is an LCD code?
What are LCD codes? An LCD is a determination by a Medicare Administrative Contractor (MAC) whether to cover a particular service on a MAC -wide, basis.
What is LCD in healthcare?
LCDs are developed to deny coverage or limit coverage of a service to specific conditions or frequencies. We will consider medically reasonable and necessary services for payment in the absence of an LCD, billing, and coding article, NCD, or CMS manual instruction limiting coverage.
What happens if a Medicare patient denies a service?
If a service denies, you and the patient have a right to request a redetermination of the denial.
What is the KX modifier?
The KX modifier is to be used for diagnostic procedures only.
How many levels can a provider do per region?
The correct clarification is a provider can do one-two levels per region, per session, and is stated correctly in the LCD.
Does Medicare require pre-certification?
Traditional Medicare does not provide pre-certification or prior authorization except for certain hospital outpatient department (OPD) services and specific ambulance services. For more information on prior authorization for specific ambulance services, please refer to Prior Authorization of Repetitive, Scheduled Non-Emergent Ambulance Transport.
What is LCD in Medicare?
* An LCD is a decision by a Medicare contractor whether to cover a particular item or service. LCDs contain “reasonable and necessary” information and are administrative and educational tools to assist you in submitting correct claims for payment.#N#* LCDs are located in the Medical Policy Center on the Highmark Medicare Services website.
How to search for LCDs?
In addition, you can search for LCDs by diagnosis code on the CMS website. The Medicare coverage database external link allows you to search for LCDs in a variety of ways including keywords, “L number,” CPT/HCPCS procedure codes, and ICD-10 diagnosis codes. Search the Medicare coverage database external link. For more information, please review the Finding First Coast LCDs and related coverage information — how-to guide.
How to find an LCD on First Coast?
The quickest way is to use the MCD quick find. You will need the L CD ID (“L” number to use the quick find feature; if you do not have the LCD ID but you do have the procedure code, you can use First Coast’s fee schedule lookup to find an LCD if one exists for that service. Complete the fee lookup form and if an LCD exists a link to it will be displayed beneath the fee results.
What is the National Coverage Determinations Manual?
* The National Coverage Determinations Manual describes whether specific medical items, services, treatment procedures, or technologies can be paid for under Medicare. All decisions that items, services, etc. are not covered are based on §1862 (a) (1) of the Act (the “not reasonable and necessary” exclusion) unless otherwise specifically noted.#N#* NCDs are located on the CMS website.