Additionally, many over-the-counter medications are excluded as a part of Medicare Part D regulations, so medical therapies that may include B12 are also generally not covered if they are not a part of your drug plan’s formulary, or list of covered drugs. Although Medicare does not cover B12 shots under Part D, seniors may still be able to receive access to these injections at little or no cost under a plan utilization management program.
Full Answer
Does Medicare cover vitamin B12 injections?
Medicare Part D prescription drug plans expressly excludes coverage for vitamins - although some Medicare plans do cover "excluded" drugs such as B-12 vitamin injections as "Bonus" or Supplemental drugs. However, in specific cases - or for specific conditions, Medicare will cover the administration of Vitamin B-12 injections.
Does Aetna pay for vitamin B12 shots?
Still, there are a host of health problems that don’t go away with minimum vitamin B12 shots; constant fatigue, brain fog, and depression can continue if you’re not getting enough vitamin B12 from your healthcare provider. Aetna will pay for vitamin B12 injections if you suffer from:
How much do vitamin B12 shots cost?
While vitamin B12 shots can be expensive, costing upwards of $25 a pop, there are alternative methods of vitamin B12 supplementation that are available online and over the counter (OTC). Many are cheaper, gentler, and more convenient than vitamin B12 shots, and just as likely to get absorbed into your bloodstream.
Do you need a nurse to get a B12 shot?
Even if you’re approved, you may not be getting the right dosage to relieve some of the ailments that come with even mild vitamin B12 deficiency. Intramuscular vitamin B12 shots require the services of a licensed nurse, and to get your fill, your best bet is to apply for coverage from your medical insurance plan.
Is cyanocobalamin injection covered by Medicare?
No. In general, Medicare prescription drug plans (Part D) do not cover this drug.
Is B12 shots covered by insurance?
If you have been formally admitted into a hospital, reside in a skilled nursing facility, or hospice and your physician orders a B12 shot as medically necessary treatment, Part A (hospital insurance) may help cover the costs.
How much does it cost to get a B12 shot?
How much does it cost to get a b12 shot? The cost of a B12 shot can vary based on your insurance. Typically, they cost about $50-80.
How much does a B12 shot cost without insurance?
The cost for Vitamin B12 injectable solution (1000 mcg/mL) is around $90 for a supply of 25 milliliters, depending on the pharmacy you visit. Prices are for cash paying customers only and are not valid with insurance plans.
How do I bill Medicare for B12 injections?
Coding a B12 injection 90782 would be correct for a patient with private insurance. However, for patients covered by Medicare, code G0351 would be the injection code for 2005. J3420, “Injection, vitamin B12 cyanocobalamin, up to 1,000mcg,” is the HCPCS code for reporting physician provision of the medication.
Is B12 test covered by Medicare?
The Centers for Medicare & Medicaid Services also do not provide coverage for routine testing for vitamin B12 deficiency. There is agreement within the literature that serum vitamin B12 testing should be used to diagnose vitamin B12 deficiency in symptomatic and high-risk populations.
Can I get a B12 injection at a pharmacy?
So long as you haven't had a B12 injection in the past 28 days and aren't scheduled to have one in the next 28 days you can purchase a voucher for a B12 injection at your nearest participating pharmacy.
How long do B12 injections last?
If your vitamin B12 deficiency is not caused by a lack of vitamin B12 in your diet, you'll usually need to have an injection of hydroxocobalamin every 2 to 3 months for the rest of your life.
How soon do you feel less tired after a B12 injection?
Key facts. Hydroxocabalamin starts to work straight away. However, it may take a few days or weeks before your symptoms start to improve and you feel better. At first, you may need to have the injection a few times a week to boost your levels of vitamin B12.
What diagnosis covers a B12 injection?
ICD-10-CM codes T50. 995A, T50. 995D, and T50. 995S apply to administration of Vitamin B12 as adjunct to Alimta®....Group 1.CodeDescriptionD51.8Other vitamin B12 deficiency anemiasD51.9Vitamin B12 deficiency anemia, unspecifiedD52.0Dietary folate deficiency anemiaD52.1Drug-induced folate deficiency anemia37 more rows
Why do you need a prescription for B12 injections?
If you are allergic to cobalamin, cobalt or any ingredients in vitamin B-12 shots, inform your doctor before the vitamin is prescribed. Your doctor most likely will avoid prescribing vitamin B-12 shots to prevent a severe life-threatening allergic reaction.
Can I give myself B12 shots?
The easiest site when self-administering an IM injection is the middle third of the vastus lateralis muscle of the thigh. Other options include the deltoid muscle of the upper arm and the dorsogluteal site on the bottom. This maybe useful if you have a carer or a family member willing to administer your injection.
How much does a B12 shot cost?
While vitamin B12 shots can be expensive, costing upwards of $25 a pop, there are alternative methods of vitamin B12 supplementation that are available online and over the counter (OTC). Many are cheaper, gentler, and more convenient than vitamin B12 shots, and just as likely to get absorbed into your bloodstream.
Does Cigna have enough B12?
Their mission is to prevent death from pernicious anemia, and they do that reasonably well…. Still, there are a host of health problems that don’t go away with minimum vitamin B12 shots; constant fatigue, ...
Does B12 cause muscle pain?
But no mention is made of vitamin B12 supplements in relation to symptoms of fatigue, muscle pain, anxiety, depression, or dizziness that occur when vitamin B12 levels are even marginally low, in people who are not diagnosed with anemia.
Does Aetna pay for B12 injections?
Aetna will pay for vitamin B12 injections if you suffer from: Diagnosed pernicious anemia, or other types of anemia. Gastrointestinal disorders linked with lack of intrinsic factor, vitamin B12 malabsorption or gastrointestinal surgeries.
Does B12 go away?
Still, there are a host of health problems that don’t go away with minimum vitamin B12 shots; constant fatigue, brain fog, and depression can continue if you’re not getting enough vitamin B12 from your healthcare provider.
Can B12 deficiency cause neuropathy?
Neuropathy (nerve damage) from alcoholism, pernicious anemia, or posterolateral sclerosis. Dementia caused by vitamin B12 deficiency. Elevated homocysteine levels caused by homocysteinuria. Also, if you have vitamin B12 deficiency caused by medications such as metformin for diabetes, then you may be able to get your insurance to pay ...
Does Medicare cover vitamin B12?
Still, Medicare Part D follows the same criteria for vitamin B12 shots as the Aetna plan. Unless you can present proof that you suffer from one of the approved medical conditions as mentioned above, you may not get coverage for vitamin B12, even if you are suffering from extreme fatigue, sluggish thinking, mood problems, ...
What is the post deductible stage?
After your deductible has been satisfied, you will enter the Post-Deductible (also called Initial Coverage) stage, where you pay your copay and your plan covers the rest of the drug cost. In the Donut Hole (also called the Coverage Gap) stage, there is a temporary limit to what Medicare will cover for your drug.
Does Medicare cover prescription drugs?
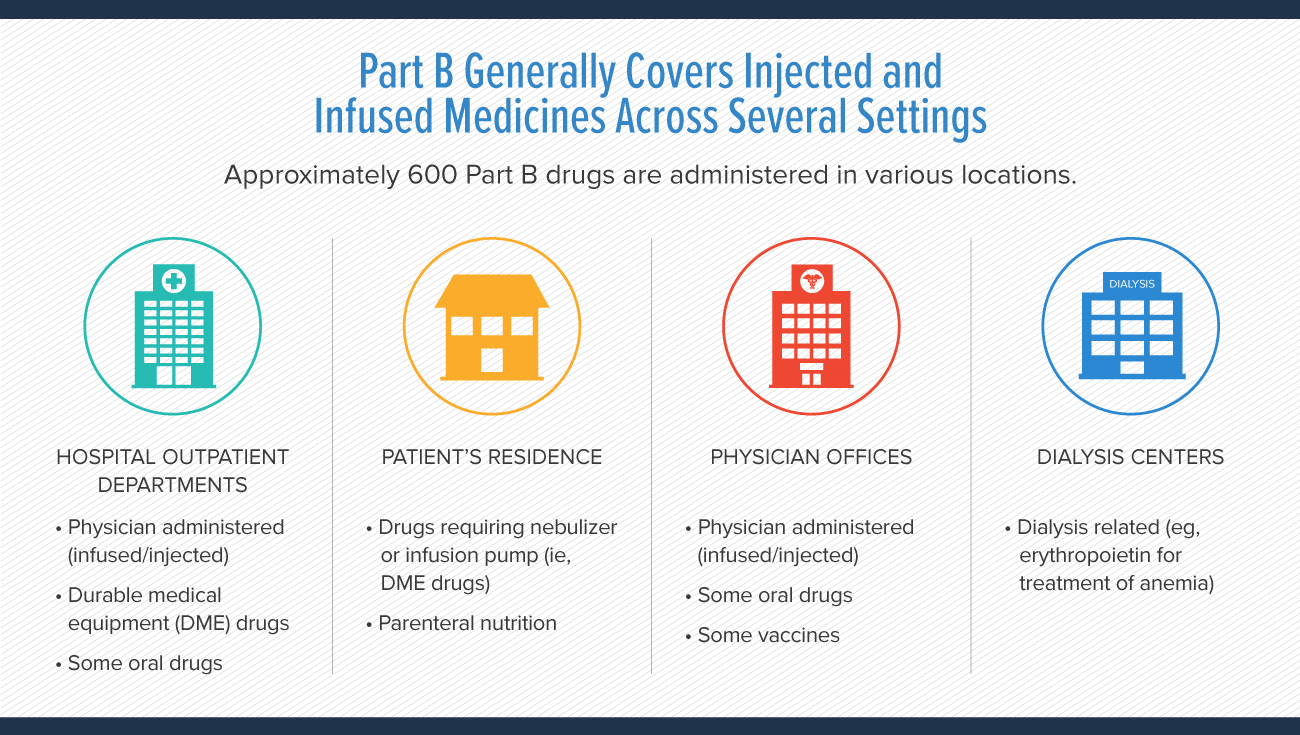
No. In general, Medicare prescription drug plans (Part D) do not cover this drug. Be sure to contact your specific plan to verify coverage information. A limited set of drugs administered in a doctor's office or hospital outpatient setting may be covered under Medical Insurance (Part B).
What is covered by Medicare Part B?
Medicare Part B covers three important vaccines as part of its preventive care benefits. Covered vaccines include the following: Flu vaccine: Annual vaccine given in one shot before or during flu season, usually November through April. Pneumonia vaccine: One-time vaccine given in two shots at least one year apart.
What is part B of the rabies shot?
Part B also covers vaccines you may need if you’re exposed to a harmful virus or bacteria by accident. You might need a tetanus shot, for example, if you step on a rusty nail. Or you may need rabies shots if you’re bitten by a stray dog.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
What is Medicare Part D?
Medicare Part D covers all commercially available vaccines needed to prevent illness. You can get Part D coverage through a stand-alone Medicare prescription drug plan (Part D) or a Medicare Advantage plan (Part C) that includes drug coverage. Vaccines covered by Part D include the following:
Is Part D covered by Part B?
Other vaccines covered: Vaccines that are "reasonable and necessary" to prevent illness and are not covered by Part B. Part D may also cover vaccines you may need if you are traveling internationally. Talk with your doctor about your travel plans and ask what vaccines are recommended.
Do you pay for a hepatitis B shot?
You pay nothing for vaccines covered by Part B – flu, pneumonia and Hepatitis B – as long as your provider accepts Medicare. Your cost for vaccines covered by Part D will depend on your specific plan. You may pay a copay or coinsurance, but it will depend on your plan and the provider.
What Parts of Medicare Cover Cortisone Injections?
Original Medicare (Medicare Parts A and B) and Medicare Advantage plans (Medicare Part C) provide limited coverage for cortisone injections.
How Much Does a Cortisone Shot Usually Cost?
The Medicare cost of a single cortisone shot can range from $25 to $300 or even more. Several factors influence the price of the injection, including:
How Often Will Medicare Pay for Cortisone Injections?
Although cortisone injections are incredibly beneficial, and the effects may last for several months, repeated injections can lead to further loss of cartilage. Doctors typically recommend a maximum of three injections annually.
Does Medicare Cover PRP Knee Injections?
Platelet-rich plasma (PRP) injections are another treatment option for post-surgery pain and chronic conditions like osteoporosis.
Does Private Insurance Cover Cortisone Injections?
Private insurance companies may offer more generous coverage for cortisone shots than Medicare with many policies covering medically necessary injections in hospitals and clinics. Insured patients may have out-of-pocket expenses as low as $10.
Medicare May Help With Pain-Relieving Injections
If a doctor suggests that cortisone injections could improve your wellbeing by relieving pain and inflammation, Medicare may cover some of the cost.
Does Medicare Pay for Knee Injections?
Whether Medicare pays for knee injections depends on what type of injection your doctor recommends, how severe your symptoms are and what other treatments have already been used to address them. For any type of knee injection, the doctor, hospital or clinic administering the injection must participate in Medicare for your plan to cover the expense.
What Is the Best Injection for Knees?
The best injection for knee osteoarthritis depends on the nature and severity of your symptoms and your overall health profile. Your doctor can recommend the right knee injection for your specific needs. Three types of injections are commonly used to treat osteoarthritis.
Does Medicare Cover Cortisone Knee Injections?
Injectable medications administered by a medical professional on an outpatient basis fall under Medicare Part B coverage. Generally, Medicare covers cortisone or corticosteroid injections for knee arthritis when a participating doctor deems that they're medically necessary.
How Often Does Medicare Pay for Cortisone Knee Injections?
Overuse of corticosteroid injections can lead to cartilage damage. As a result, doctors typically recommend no more than three cortisone shots per year. Medicare typically covers the cost of corticosteroid injections given on this dosing schedule.
Does Medicare Cover PRP Injections?
As of October 2021, Medicare doesn't cover PRP injections for any condition. In the ruling regarding the therapy, Medicare states that while early studies into the benefits of the shots for the management of osteoarthritis are promising, more research is required to prove their effectiveness.
Does Medicare Part B Cover Hyaluronic Acid Injections?
Medicare Part B may cover hyaluronic acid injections for the knee if you have symptoms of knee pain or stiffness that interfere with one or more daily living tasks like sleeping comfortably or standing for long periods of time. In addition, prior to coverage, your doctor must:
How Often Does Medicare Pay for Hyaluronic Acid Injections?
Medicare usually requires that you wait at least six months between hyaluronic acid injections. Your arthritis pain or stiffness must return for you to qualify for repeat injections.