This is because Medicare supplement insurance helps to cover the costs that original Medicare does not, such as deductibles, coinsurance, and copayments. When one has original Medicare and MediGap, original Medicare is the primary payer, meaning that original Medicare pays the portion of the bills for which it owes first.
Full Answer
Is Medicare supplemental insurance worth buying?
To help answer it for yourself, it would be wise to compare Medicare Supplement plans to the other two options available to you: Doing nothing, and sticking with Original Medicare, and; Medicare Advantage plans; If you can afford the monthly premiums, Medicare Supplement plans may very well be worth the price. This is because it can limit, or eliminate, your out-of-pocket medical costs.
What is the best and cheapest Medicare supplement insurance?
The Medicare Supplement Plan N is best for the following people:
- People looking for complete coverage at a modest monthly rate
- Those who don’t mind paying a minor fee at the time of service
- People who are not subject to Part B excess charges
Why every senior should have a Medicare supplement plan?
Why Every Senior Should Have a Medicare Supplement Plan Medicare supplement plans are largely considered to be essential for seniors who wish to avoid costly expenses that could put a dent into their retirement savings. There are many reasons as to why every senior should have a Medicare supplement plan.
What are the top 5 Medicare supplement plans?
- Plan G
- Plan N
- Plan A
- Plan F
- High Deductible Plan F
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
What is the purpose of Medicare supplemental insurance?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Copayments. Coinsurance.
What are the advantages and disadvantages of Medicare supplement plans?
Medicare Advantage offers many benefits to original Medicare, including convenient coverage, multiple plan options, and long-term savings. There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling.
What is the difference between Medicare and Medicare supplement?
When you buy a Medicare Supplement insurance plan, you are still enrolled in Original Medicare, Part A and Part B. Medicare pays for your health-care bills primarily, while the Medigap plan simply covers certain cost-sharing expenses required by Medicare, such as copayments or deductibles.
Is there a Medicare supplement that covers everything?
Medicare Supplement insurance Plan F offers more coverage than any other Medicare Supplement insurance plan. It usually covers everything that Plan G covers as well as: The Medicare Part B deductible at 100% (the Part B deductible is $203 in 2021).
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
What are the disadvantages of a Medicare supplement plan?
Medicare Advantage Plans do have a yearly limit on your out-of-pocket costs for medical services, called the maximum out-of-pocket (MOOP). Once you reach this limit, you'll pay nothing for covered services.
What are two disadvantages of Medicare?
You might not be able to choose when to be admitted. Medicare doesn't include ambulance service costs. Medicare won't cover you for private patient hospital costs, such as theatre fees and accommodation. It won't cover you for medical and hospital costs you incur in another country.
What is the downside to Medigap?
Some disadvantages of Medigap plans include: Higher monthly premiums. Having to navigate the different types of plans. No prescription coverage (which you can purchase through Plan D)
Can I switch from Medicare Advantage to Medicare supplement?
Once you've left your Medicare Advantage plan and enrolled in Original Medicare, you are generally eligible to apply for a Medicare Supplement insurance plan. Note, however, that in most cases, when you switch from Medicare Advantage to Original Medicare, you lose your “guaranteed-issue” rights for Medigap.
What is the average cost of supplemental insurance for Medicare?
In 2020, the average premium for Medicare supplemental insurance, or Medigap, was approximately $150 per month or $1,800 per year, according to Senior Market Sales, a full-service insurance organization. Several factors impact Medigap costs, including your age and where you live.
Is Medicare Advantage more expensive than Medicare?
Clearly, the average total premium for Medicare Advantage (including prescription coverage and Part B) is less than the average total premium for Original Medicare plus Medigap plus Part D, although this has to be considered in conjunction with the fact that an enrollee with Original Medicare + Medigap will generally ...
Medicare Supplement Plans Help Pay Medicare Part A and Part B Costs
Original Medicare, the health coverage you can get when you turn 65 or have a qualifying disability, consists of Medicare Part A and Part B. Part A...
Ten Advantages of Medicare Supplement Plans
1. Large medical bill protectionLet’s say you regularly need to purchase Medicare-covered, but costly, medical supplies. Under Medicare Part B, 80...
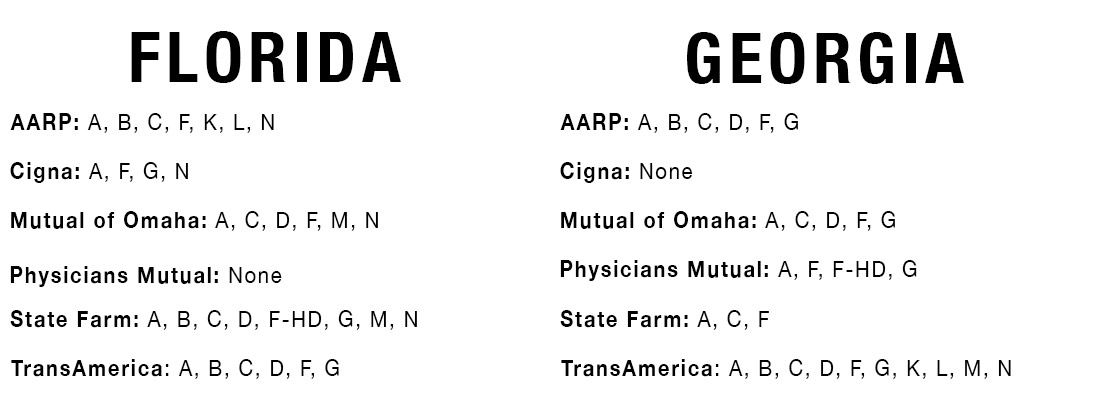
Medicare Supplement Plans by State
There are 10 standardized Medicare Supplement plans in 47 states sold by private insurers. These plans are named by letter (Plan A through Plan N;...
Medicare Supplement Plans and The Part B Premium
You need to keep your Original Medicare insurance and continue paying your Part B premium when you get a Medicare Supplement plan. Medicare Supplem...
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
Can you cancel a Medigap policy?
This means the insurance company can't cancel your Medigap policy as long as you pay the premium. Some Medigap policies sold in the past cover prescription drugs. But, Medigap policies sold after January 1, 2006 aren't allowed to include prescription drug coverage.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible.
What is Medicare Supplement Insurance?
Medicare Supplement insurance is meant to limit unpleasant surprises from healthcare costs. Your health at age 65 may be no indicator of what’s to come just a few years later. You could get sick and face medical bills that devastate years of planning and preparation. Combine this with the fixed income that so many seniors find themselves on, ...
How much does Medicare Supplement cover?
Choosing Medicare Supplement insurance can help. It can cover up to 100% of out-of-pocket costs, depending on the plan. One out of every three Original Medicare beneficiaries — over 13 million seniors — have chosen to do so. 1.
What is the deductible for hospitalization in 2020?
You are responsible for the balance (or coinsurance). In 2020, the Part A deductible for hospitalization is $1,408 per benefit period and the Part B annual deductible is $198. 3. Medicare Supplement insurance is designed to help cover these out-of-pocket deductibles and coinsurance.
How long is the open enrollment period for Medicare?
The Medigap Open Enrollment Period covers six months. It starts the month you are 65 or older and are enrolled in Medicare Part B. In this period, no insurer offering supplemental insurance in your state can deny you coverage or raise the premium because of medical conditions.
How many separate insurance plans are there?
Premiums for the same policy can vary between insurance companies. But, only the quoted price and the reputation of the insurer will vary. There are ten separate plans, labeled A through N. Two plans, C and F, are no longer offered to newly eligible beneficiaries.
Does Medicare Supplement cover all costs?
Original Medicare does not cover all costs. Medicare Supplement insurance, or Medigap, can cover what Medicare does not. Private insurance companies – vetted by the federal government – offer it to help manage out-of-pocket expenses. These policies do not add coverage.
Can you renew a Medigap policy?
You can renew your Medigap policy as long as you pay the premium. The insurer cannot use your health problems to cancel your policy or raise your premium.
Why Do I Need Supplement Insurance with Medicare?
Original Medicare Parts A & B don’t cover all medical benefits necessary for seniors, such as prescription medication and vision and dental care.
What Are The Gaps in Original Medicare?
As you may well know by this point, it is impossible to ignore the existing gaps in Original Medicare coverage. For a federal program that has so many coverage policies, there are two main forms of coverage where it usually fails to provide benefits.
Deciding On Whether You Need Supplemental Insurance
Now that we have covered all that there is to know about Medigap and Medicare, it is important you utilize this information in order to make an informed decision about your Medicare coverage. If you would like more information on either Medigap, Medicare Advantage, or Part D plans, give us a call.
What Is Medicare Advantage?
Medicare Advantage (also known as Part C) plans are provided by private insurers and essentially replace Original Medicare as your primary insurance. They cover all Medicare-covered benefits and may also provide additional benefits like some dental, hearing, vision and fitness coverage.
What Are the Benefits of Medicare Advantage?
Medicare Advantage plans provide all the same benefits provided by Original Medicare, plus coverage for items and services not covered by Original Medicare, including some vision, some dental, hearing and wellness programs like gym memberships.
How Much Does Medicare Advantage Cost?
Many Medicare Advantage plans have a $0 premium, so be sure to explore your options. Baethke explains it like this: “If you enroll in a plan that does charge a premium, you must pay this fee every month in addition to your Medicare Part B premium, which is around $149 [or higher, depending on your income].”
What Is Medicare Supplement?
Medicare Supplement plans (commonly known as Medigap plans) are sold by private insurance companies to help fill the gaps of Original Medicare coverage.
What Are the Benefits of a Medicare Supplement Plan?
A Medicare Supplement plan makes your out-of-pocket costs more predictable and easier to budget.
How Much Does a Medicare Supplement Plan Cost?
The estimated average monthly premium (the amount you pay monthly) for a Medicare Supplement plan can range from $150 to around $200, depending on the state you live in and your insurer.
Sources
NORC at the University of Chicago. Innovative Approaches to Addressing Social Determinants of Health for Medicare Advantage Beneficiaries. Better Medical Alliance. Accessed 9/6/21.
What is Medicare Supplement?
Medicare supplement insurance policies help fill in the gaps left by Original Medicare health care insurance. For many people, Medicare Supplement, also known as Medigap, insurance helps them economically by paying some of the out-of-pocket costs associated with Original Medicare.
What percentage of Medicare supplement is paid?
After this is paid, your supplement policy pays your portion of the remaining cost. This is generally 20 percent. Some policies pay your deductibles The deductible is a set amount which you must pay before Medicare begins covering your health care costs.
How many people does Medicare Supplement cover?
Keep in mind that, just like Medicare, Medicare Supplement plans are individual insurance policies. They only cover one person per plan. If you want coverage for your spouse, you must purchase a separate plan.
How long does it take to get a Medigap plan?
When you turn 65 and enroll in Part B, you will have a 6-month Initial Enrollment Period to purchase any Medigap plan sold in your state. During this time, you have a “guaranteed issue right” to buy any plan available. They are required to accept you and cannot charge you more due to any pre-existing conditions.
How long does Medicare cover travel?
Each plan varies in what it covers, but all plans pay for Medicare Part A (hospital insurance) coinsurances for up to 365 days beyond the coverage that Medicare offers. Some of the plans cover a percentage of the cost for emergency health care while traveling abroad.
How old do you have to be to qualify for medicare?
To be eligible for Medicare, you must be at least 65 years old, a citizen of the United States or permanent legal resident for at least five consecutive years. Also, you, or your spouse, must have worked and paid federal taxes for at least ten years (or 40 quarters).
Does Medicare cover long term care?
Most plans do not cover long-term care, vision, dental, hearing care, or private nursing care. All Medicare Supplement insurance coverage comes with a monthly premium which you pay directly to your provider. How much you pay depends on which plan you have.
What is Medicare Supplement Plan?
Medicare Supplement plans are also offered by private insurance companies, and can help you pay out-of-pocket costs for services covered under Medicare Part A and Part B. Different Medicare Supplement plans pay for different portions of those costs, such as copayments, coinsurance, and deductibles. Medicare Supplement plan benefits are standardized ...
What is Medicare Advantage?
The Medicare Advantage (Medicare Part C) program gives you an alternative way to receive your Medicare Part A (hospital insurance) and Part B (medical insurance) benefits. The exception is hospice care, which continues to be covered by Part A. Offered by private insurance companies contracted with Medicare, Medicare Advantage plans often include ...
Which states have standardized Medicare Supplement plans?
Medicare Supplement plan benefits are standardized across most of the country. (Massachusetts, Minnesota, and Wisconsin each standardize Medicare Supplement plans differently.) Some Medicare Supplement plans may extend coverage to emergency care you receive while traveling outside the United States (80% of approved costs up to plan limits), ...
Does Medicare Supplement Plan include prescription drug coverage?
In situations such as these, your new Medicare Supplement plan won’t include prescription drug coverage—even if you had this coverage in your former Medicare Supplement plan (plans sold today don’t include prescription drug coverage). You may be able to enroll in a stand-alone Medicare Prescription Drug Plan if you leave your Medicare Advantage ...
Does Medicare Supplement work with Medicare Advantage?
If you keep your Medicare Supplement plan, you must keep paying your Medicare Supplement plan premium, but your Medicare Supplement plan won’t work with your Medicare Advantage plan. That is, the Medicare Supplement plan will not pay any of the deductibles, coinsurance, copayments or premium (if any) of your Medicare Advantage plan.
Can you visit any doctor with Medicare Supplement?
Most Medicare Supplement plans let you visit any doctor who accepts Medicare assignment. There’s one type of Medicare Supplement plan, called a Medicare SELECT plan, that might require you to use providers in the plan network.
Does Medicare have special needs?
The government-sponsored Medicare program does not have this protection. Some Medicare Advantage plans (called Medicare Special Needs Plans) are designed to help people with special health-care needs, such as diabetes or congestive heart disease.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is Medicare Advantage?
Medicare Advantage plans negotiate contracts with networks doctors, hospitals, and other healthcare providers. The agreements they reach can help to keep their costs lower. This means that you must adhere to their networks or face substantially higher out of pocket costs.
How are Medicare Advantage Plans structured?
How Medicare Advantage Plans Are Structured. Medicare Advantage replaces your Medicare Part A and Part B services. Most of the time it replaces your Part D as well. A Medicare Advantage plan combines them into one coverage with a private insurance company. This is what is known as Part C of Medicare.
How long does it take to get a Medigap plan?
This period starts six months before you enroll in Part B of Medicare and continues the six months after. Medicare Advantage and Part D allow a 3-month open enrollment before and after your date of first coverage under Part B. You will likely have to be underwritten to get a Medigap plan once you are out of your Open Enrollment period.
How long does Medicare lock you in?
If you enroll in a Medicare Advantage plan, Medicare locks you into that plan until December 31st. Medicare Advantage plans and Part D prescription drug plans have only one window of opportunity each year for you to enroll. It happens from October 15 through December 7 each year. During that time, you can change plans or go from MAPD to original Medicare with a Medicare Supplement plan (or vice versa). There are Special Enrollment periods such as if you move out of your network coverage area. You have an Initial Enrollment Period three months before and three months after you first enroll in Part B of Medicare. Other than that, you cannot change plans or move back to original Medicare.
What is a Medigap plan?
Under a Medigap plan, Medicare first pays its portion of the bill and then sends the remainder of the bills to your Medicare supplement company to pay their portion. This is done electronically through what is called the crossover system.
What are the different types of Medicare insurance?
There are two types of private plans that you can purchase that will help fill the gaps of Medicare – Medicare supplements (Medigap) or Medicare Advantage. These two plans are very different and it is imperative that you understand the differences.
How much does Medicare cover in 2021?
If you go with Medicare alone with no additional coverage, you will quickly learn that there are a lot of gaps that Medicare does not cover – a Part A deductible ($1,484 in 2021) that you must pay to the hospital to cover you for up to 60 days of hospital care.
Is United American Insurance endorsed by the government?
The purpose of this communication is the solicitation of insurance. United American Insurance Company is not connected with, endorsed by, or sponsored by the U.S. government, federal Medicare program, Social Security Administration, or the Department of Health and Human Services. Policies and benefits may vary by state and have some limitations and exclusions. Individual Medicare Supplement insurance policy forms MSA10, MSB10, MSC10, MSD10, MSF10, MSHDF10, MSG10, MSHDG, MSK06R, MSL06R, MSN10 and in WI, MC4810 and MC4810HD, MC4810HDG are available from our Company where state-approved. Some states require these plans be available to persons under age 65 eligible for Medicare due to disability or End Stage Renal disease (ESRD). You may be contacted by an agent or producer representing United American Insurance Company, PO Box 8080, McKinney, TX 75070-8080. OUTLINE OF COVERAGE PROVIDED UPON REQUEST.
Is United American a Medicare Supplement?
United American has been a prominent Medicare Supplement insurance provider since Medicare began in 1966. Additionally, we’ve been a long-standing participant in the task forces working on Medicare Supplement insurance policy recommendations for the National Association of Insurance Commissioners.
Does Medicare Supplement Insurance cover deductibles?
The purpose of Medicare Supplement Insurance is to cover the cost left by deductibles and coinsurance in Original Medicare, but as full Medicaid coverage should cover the majority of those costs, a Medicare Supplement Insurance policy isn’t necessary. 3.