In addition, MCOs can improve access to care for beneficiaries. Evidence suggests that, compared to state-run fee-for-service, managed care can reduce overall Medicaid Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…Medicaid
Full Answer
What are the advantages and disadvantages of managed care?
- Advantages of Managed Care Plans 1. Instant Solution to Health Care 2. Unites Families 3. Confirmed Care 4. Reduced Cost 5. Simplified Management of Prescription
- Disadvantages of Managed Care Plans 1. Loss of Privacy 2. Limited Care 3. Treated as Merchandise 4. Longer Wait Time 5. Forced Advocacy
- Conclusion
What are the issues in managed care?
managed care
- History of managed care. The origins of managed care in the United States can be traced to the late 19th century, when a small number of physicians in several U.S. ...
- Defining managed care. ...
- Managed care organizations. ...
- Advantages and drawbacks. ...
What are the pros and cons of managed care plans?
Managed Care pros and cons The pros of managed care are since the patient is limited to a specific caregiver the premium is lower. The patient only pays a monthly payment and a co-payment. The cons of managed care are that the patients are not allowed to see the doctor of their choice unless the doctor is in their network.
What is the purpose of managed care?
What is the purpose of managed care? Its main purpose is to better serve plan members by focusing on prevention and care management, which helps produce better patient outcomes and healthier lives. Managed care also helps control costs so you can save money.

Why is managed care important?
Its main purpose is to better serve plan members by focusing on prevention and care management, which helps produce better patient outcomes and healthier lives. Managed care also helps control costs so you can save money.
What are some advantages of managed care?
What Are the Advantages of Managed Care?It lowers the costs of health care for those who have access. ... People can seek out care from within their network. ... Information moves rapidly within a network. ... It keeps families together. ... There is a certain guarantee of care within the network.More items...•
Is managed care the same as Medicare?
Managed care plans are also referred to as Medicare Part C (Medicare Advantage) plans. These plans cover everything original Medicare does, and they often cover additional services as well. For example, original Medicare doesn't cover routine dental care, but many managed care plans do.
What is the goal of managed care?
Managed care is any method of organizing health care providers to achieve the dual goals of controlling health care costs and managing quality of care.
What are the four goals of managed care?
Purchasers with vision can use managed care arrangements to achieve specific goals: improve access to care, enhance the quality of care, better manage the cost of care, increase the effectiveness of care, and facilitate prevention initiatives.
Is managed care effective?
While much research has been conducted on whether managed care delivery systems result in better outcomes than traditional fee for service (FFS), there is no definitive conclusion as to whether managed care improves or worsens access to or quality of care for beneficiaries.
What do you mean by managed care?
uncountable noun. Managed care is a method of controlling the cost of medical care by fixing a doctor's fees and limiting a patient's choice of doctors and hospitals. [US]
Does managed care work within the Medicare system?
The HMO premiums might be covered in full by Medicare or might require additional payments by enrollees and/or employers. It is also important to understand the context in which enrollment in Medicare HMOs occurs. The Medicare program has two arrangements for contracting with HMOs, cost- and risk-based contracts.
Is Medicare a managed care plan?
Medicare is a national health insurance program for seniors or those with disabilities. Medicare Advantage is Medicare's managed care program. If you join Medicare Advantage, you get all your care through an HMO or PPO that has a contract with Medicare.
What are the most significant impacts of managed care for patients?
Conclusions: Many physicians surveyed believe managed care has significant negative effects on the physician-patient relationship, the ability to carry out ethical obligations, and on quality of patient care. These results have implications for health care system reform efforts.
What is managed care what are some of the benefits of managed care what are some of the disadvantages?
Benefits of managed care include patients having multiple options for coverage and paying lower costs for prescription drugs. Disadvantages include restrictions on where patients can get services and issues with finding referrals.
What is Medicare managed care?
A Medicare managed care plan is a type of Medicare Advantage plan. Learn what managed care plans are and how they could be a good fit for you. A Medicare managed care plan is one type of Medicare Advantage plan. The term “managed care plan” generally refers to HMO (health maintenance organization), PPO (preferred provider organization) ...
What is managed care network?
The networks of managed care plans often include pharmacies, which can help make ordering and filling prescriptions faster and easier for everyone involved . There’s less uncertainty about a beneficiary’s costs for care in a managed care plan, provided they stay within the assigned network for qualified services.
What is a HMO plan?
Health maintenance organization (HMO) In a Medicare HMO plan, you use a primary care physician to coordinate your care, and you receive services from a network of health care providers that partner with your plan. Preferred provider organization (PPO)
What are the different types of Medicare plans?
Types of Medicare managed care plans 1 Health maintenance organization (HMO)#N#In a Medicare HMO plan, you use a primary care physician to coordinate your care, and you receive services from a network of health care providers that partner with your plan. 2 Preferred provider organization (PPO)#N#In a Medicare PPO plan, you may or may not use a primary care physician, and you are typically not required to get a referral to see a specialist. You’ll have a network of providers from which to choose .You will generally can receive at least some coverage when receiving care outside of the network of providers, though your health care services may cost more than if you received them from a provider within your plan network. 3 Point of service (POS)#N#You can use a primary care physician in a Point of Service plan, as you would with an HMO plan. But as with a PPO plan, you can go outside of the plan network and still receive some coverage for services, though you may pay higher out-of-pocket costs than if you selected an in-network provider.
How to contact Medicare Advantage?
For more information about managed care plans or other types of Medicare Advantage plans, including plan benefits, eligibility, enrollment and availability, contact a licensed insurance agent by calling. 1-800-557-6059. 1-800-557-6059 TTY Users: 711 24 hours a day, 7 days a week.
Why do you see a primary care physician?
Seeing a primary care physician allows patients to build a rapport with their doctor, and the doctor gets to know the patient’s health history firsthand . When a patient is referred to a specialist, there is communication between the primary care physician and the specialist regarding the patient’s health and treatment.
Why are patient records transferred?
A patient’s medical records are typically transferred between providers in the network for increased communication. The increased coordination allows primary care physicians and other providers within the network to make more informed decisions regarding a beneficiary’s care.
Why is managed care important?
Managed care also helps control costs so you can save money .
What is Medicare Advantage?
Medicare Advantage (Part C) is personal insurance from private companies that’s approved by Medicare. Plan types that are available run the gamut — from HMO to PPO to POS — and include coverage for preventive healthcare, routine and major care, prescription drug coverage, even emergency coverage when traveling outside Nevada.
What is an HMO plan?
HMO: lower monthly premiums, comprehensive benefits. With an HMO plan, a primary care physician (PCP) typically must be selected. The PCP is responsible for coordinating all the members’ healthcare — a referral is often required before seeing a specialist or another physician.
What happens to managed care companies?
In return, managed care companies provide their patients with all necessary care , including all-important care coordination. These firms are at risk for costs, so if they can manage expenses, they may keep the extra payment as profit but if their costs of care exceed the Medicare payment, they will lose money.
How many seniors were in Medicare Advantage in 2012?
In 2012, about 13 million seniors participated in Medicare Advantage (MA) managed care plans—about 27 percent of the Medicare population and twice as many as were enrolled just seven years ago. This rapid shift to managed care by seniors may be just a first step towards a fundamental change in the way Medicare is delivered and financed.
What is MA plan?
MA plan have enormous potential to better coordinate care for seniors and others with chronic disease. Someday, they may also become the basis for a system that integrates medical care with long-term supports and services. For now, MA plans in all their forms remain a work in process.
Does Medicare pay MA plans?
In October, it reported 127 plans had 4 or 5 star ratings. For now, MA plans do not necessarily save Medicare money.
Is MA less likely to have outpatient surgery?
A December, 2012 study for the journal Health Affairs found that MA patients were one-quarter to one-third less likely to visit hospital emergency departments, likely to spend less time in the hospital, and less likely to receive outpatient surgery. On the other hand, rates of doctor visits were about the same as in fee-for-service Medicare.
Is MA getting higher Medicare subsidies?
In fact, for several years MA plans have been getting higher Medicare subsidies than fee for service providers. The 2010 health law will gradually reduce the level of these subsidies and plans will have to find ways to provide high quality care for less money—the challenge that fee for service Medicare providers already face.
What is Medicare akin to?
Medicare is akin to a home insurance program wherein a large portion of the insureds need repairs during the year; as people age, their bodies and minds wear out, immune systems are compromised, and organs need replacements. Continuing the analogy, the Medicare population is a group of homeowners whose houses will burn down each year.
When did Medicare start a DRG?
In 1980 , Medicare developed the diagnosis-related group (DRG), the bundling of multiple services typically required to treat a common diagnosis into a single pre-negotiated payment, which was quickly adopted and applied by private health plans in their hospital payment arrangements.
What percentage of Medicare enrollees are white?
7. Generational, Racial, and Gender Conflict. According to research by the Kaiser Family Foundation, the typical Medicare enrollee is likely to be white (78% of the covered population), female (56% due to longevity), and between the ages of 75 and 84.
How much did Medicare cost in 2012?
According to the budget estimates issued by the Congressional Budget Office on March 13, 2012, Medicare outlays in excess of receipts could total nearly $486 billion in 2012, and will more than double by 2022 under existing law and trends.
Why does home insurance increase?
Every year, premiums would increase due to the rising costs of replacement materials and labor. In such an environment, no one could afford the costs of home insurance. Casualty insurance companies reduce the risk and the cost of premiums for home owners by expanding the population of the insured properties.
How many elderly people are without health insurance?
Today, as a result of the amendment of Social Security in 1965 to create Medicare, less than 1% of elderly Americans are without health insurance or access to medical treatment in their declining years.
What is rationing care?
Rationing Care. Specifically, care can be rationed in the last months of life to palliative treatment. Currently, 12% of Medicare patients account for 69% of all Medicare expenses, usually in the last six months of life.
Why do patients have insufficient access to health care providers?
Patients have insufficient access to health care providers and lack of coordination and continuity of care, mainly because of low payment rates ; despite this, states and the federal government face rapid growth in total program costs.
What is CMS in healthcare?
In the case of Medicaid managed care, the Centers for Medicare and Medicaid Services (CMS) is charged with approving rates states pay to MCOs based on an actuary's certification that the rates meet the appropriate requirements. Of course, actuarial soundness is much easier to define in theory than to evaluate in practice.
What is a compromise between Medicaid and MCO?
A compromise between the two extremes involves risk-sharing, in which the Medicaid program and the MCO share the risk of variation in utilization outside a specified “risk corridor.”.
What do actuaries need to know about health care?
Actuaries must develop statistical estimates of patients' utilization of health care services, based on a variety of information including demographic and diagnostic information on the relevant population and assumptions or forecasts of how these factors may change over time.
What are the benefits of MCOs?
These additional services can significantly benefit patients. In addition, MCOs can improve access to care for beneficiaries.
What is setting specific per patient monthly rates?
Setting specific per-patient monthly rates transfers the risk of statistical variation in health care needs from the state and the federal governments to the MCOs. While this is a benefit for the governments, it is a downside for the MCOs. As a result, MCOs must require rates that take into account, and compensate for, ...
Does Medicaid Managed Care have a positive impact on health outcomes?
Conclusion. Medicaid managed care has the potential to significantly improve access to health care and health outcomes for the Medicaid population . It may also have the potential to reduce program costs.
What are the aspects of Medicaid managed care?
Aspects of Medicaid managed care that may affect access to and quality of care. Economic incentives. Under the FFS model, the state pays providers directly for each covered service received by a Medicaid enrollee.
Why is it so difficult to evaluate the quality of managed care?
Quality is a somewhat subjective concept and can be evaluated using both process measures (e.g., if certain protocols were correctly followed) or outcomes (e.g., if treatments resulted in positive results).
What is capitation rate in managed care?
Under managed care, the state pays a managed care plan a capitation rate—a fixed dollar amount per member per month —to cover a defined set of services for each person enrolled in the plan. In turn, the plan pays providers for all of the Medicaid services an enrollee may require that are included in the plan’s contract with the state.
What is covered benefits contract?
Covered benefits. Contracts between the state and MCOs identify which state plan services are the responsibility of the MCO, which (if any) remain covered by the state, and which (if any) are provided by other vendors or through other delivery systems.
How long is Medicaid data reported?
In addition, data are only reported for individuals who are continuously enrolled for 12 months, so they may not be representative of the entire Medicaid managed care population.
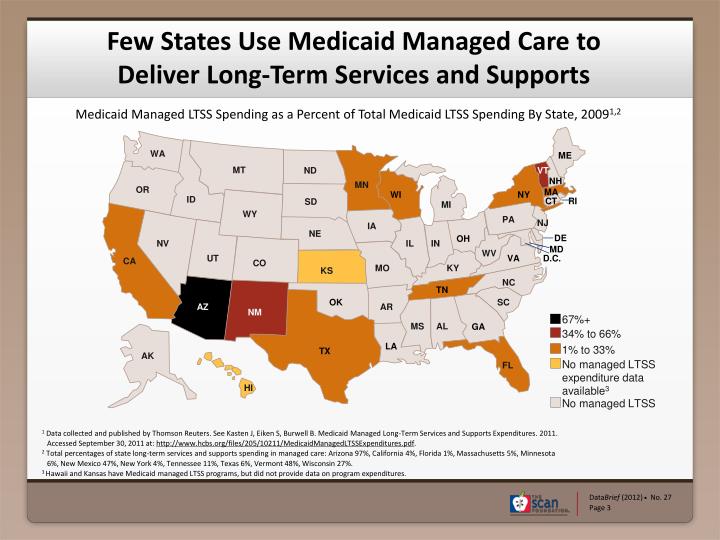
Why are long term services carved out of Medicaid?
In some cases, benefits that are unique to Medicaid and have not been traditionally delivered through managed care, such as long term services and supports or non-emergency transportation are carved out of the capitated benefit package in order to maintain access to these services.
How long does it take for a diabetic to be readmitted to Medicaid?
The researchers concluded that children with Type 1 diabetes enrolled in Medicaid managed care plans were less likely to be readmitted within 90 days of discharge, possibly indicating greater access to services that helped them prevent readmissions ( Healy-Collier et al. 2016 ).