
But why is Medicare so resistant to reimbursement for telemedicine? There are two main reasons for this: 1. Congress believes that telemedicine would raise costs. According to the Congressional Budget Office and its analysts, encouraging the use of telemedicine could increase Medicare expenses.
Full Answer
How to qualify for Medicare telehealth reimbursement?
in order to be reimbursed for live-video telehealth, the patient must be located in a non-metropolitan statistical area (msa) or a rural health professional shortage area (hspa), although cms did add some exceptions to their geographic requirement (based on statute) in 2019 for acute stroke and end stage renal disease (esrd) related visits, and …
How to get reimbursed for telemedicine?
This might include things like:
- Virtual check-ins with a patient after they are discharged from the hospital
- Outpatient follow up care
- Determining the risk of infection
- Counseling services
- Instructing patients on self-performed rehab exercises
Does Medicare reimburse for telehealth?
Medicare does not reimburse for the use of mobile communication devices to deliver care to patients. Geographic limitations With the exception of the Medicare Chronic Care Management Program, Medicare places certain restrictions on where patients can be located when receiving telehealth services.
Does Medicaid reimburse for telehealth in my state?
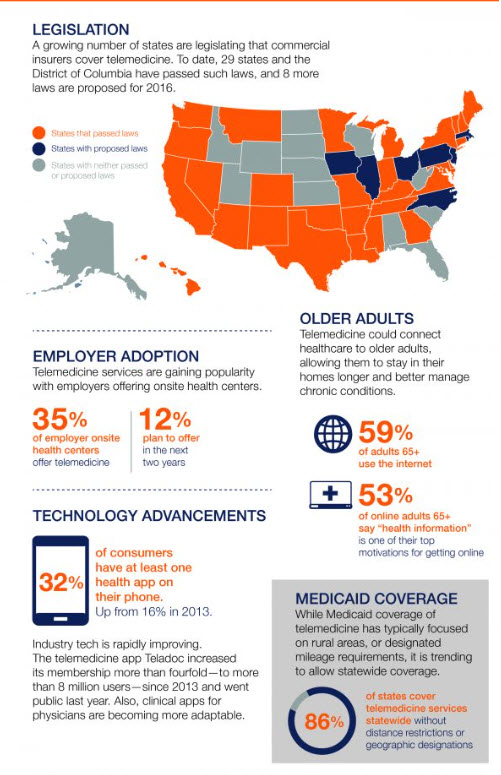
States continue to refine their telehealth reimbursement policies with regard to Medicaid and private payer laws. Medicaid policies include those with some type of reimbursement for telehealth but the scope of these policies varies among states. All states and District of Columbia reimburse for live video services in their Medicaid program.
What would the Medicare Payment Advisory Commission report on?
Additionally, if passed, the Act would require that the Medicare Payment Advisory Commission report on information relating to the access of Medicare beneficiaries to telehealth services at home.
What is telebehavioral health?
Telebehavioral health is where the action is — and has been for decades. Let’s first consider the medical example of Carlos, a 60-year-old who has developed a sore on his left big toe. If that sore is an early warning sign of diabetes, it can lead to many complications, including amputation and non-ambulatory.
Can telehealth be waived?
The Secretary of Health and Human Services would have the authority to waive telehealth restrictions. Telehealth restrictions would be waived during public health emergencies.
Why do employers purchase health plans that are designed to cost less?
The point is that employers typically purchase health plans that are designed to cost less because they offer benefits for the short term. Many US-based insurance companies are thus, in essence, disincentivized from intervening in a problem in its early phase.
Is Medicare telehealth a part of the future?
Medicare Telehealth: Paving the Future for Expanding Telehealth Practices. For those considering a hybrid or full-time, exclusive telehealth future, TBHI has been suggesting that almost a year centering one’s future telehealth efforts on serving Medicare telehealth beneficiaries has been well advised.
Is telehealth legal in rural areas?
Current legislation only approves telehealth services for patients living in certain rural areas. At the same time, those in urban and suburban populations are not given the same flexibility and are instead excluded from accessing virtual care. This creates a serious inequity in access to healthcare.
Is Medicare continuing to expand telehealth?
As described in the July 2020 TBHI article entitled, Waiting to Exhale about Telehealth after COVID-19, Medicare started announcing last summer that it intends to continue its telehealth expansion. Private insurers, on the other hand, started announcing rollout experiments in a variety of states.
When will Medicare start paying for telehealth?
Effective for services starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Medicare will make payment for Medicare telehealth services furnished to patients in broader circumstances.
What services does Medicare provide through telehealth?
Medicare beneficiaries will be able to receive a specific set of services through telehealth including evaluation and management visits ( common office visits), mental health counseling and preventive health screenings.
What is telehealth for Medicare?
Under President Trump’s leadership, the Centers for Medicare & Medicaid Services (CMS) has broadened access to Medicare telehealth services so that beneficiaries can receive a wider range of services from their doctors without having to travel to a healthcare facility. These policy changes build on the regulatory flexibilities granted under the President’s emergency declaration. CMS is expanding this benefit on a temporary and emergency basis under the 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act. The benefits are part of the broader effort by CMS and the White House Task Force to ensure that all Americans – particularly those at high-risk of complications from the virus that causes the disease COVID-19 – are aware of easy-to-use, accessible benefits that can help keep them healthy while helping to contain the community spread of this virus.
How long does Medicare bill for evaluation?
Practitioners who may independently bill Medicare for evaluation and management visits (for instance, physicians and nurse practitioners) can bill the following codes: 99421: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 5–10 minutes.
How do patients communicate with their doctors?
Patients communicate with their doctors without going to the doctor’s office by using online patient portals. Individual services need to be initiated by the patient; however, practitioners may educate beneficiaries on the availability of the service prior to patient initiation.
Can Medicare beneficiaries visit their doctor from home?
This will help ensure Medicare beneficiaries, who are at a higher risk for COVID-19, are able to visit with their doctor from their home, without having to go to a doctor’s office or hospital which puts themselves and others at risk.
Does Medicare pay for virtual check ins?
In 2019, Medicare started making payment for brief communications or Virtual Check-Ins, which are short patient-initiated communications with a healthcare practitioner. Medicare Part B separately pays clinicians for E-visits, which are non-face-to-face patient-initiated communications through an online patient portal.
How much does Medicare pay for telehealth?
You pay 20% of the Medicare-approved amount for your doctor or other health care provider’s services, and the Part B Deductible applies. For most telehealth services, you'll pay the same amount that you would if you got the services in person.
What is telehealth in Medicare?
Medicare telehealth services include office visits, psychotherapy, consultations, and certain other medical or health services that are provided by a doctor or other health care provider who’s located elsewhere using interactive 2-way real-time audio and video technology.
What do you call Medicare if you suspect fraud?
If you suspect fraud, call 1-800-MEDICARE.
When can telehealth be used?
Due to the Coronavirus (COVID-19) Public Health Emergency, doctors and other health care providers can use telehealth services to treat COVID-19 (and for other medically reasonable purposes) from offices, hospitals, and places of residence (like homes, nursing homes, and assisted living facilities) as of March 6, 2020.
Does Medicare offer telehealth?
Starting in 2020, Medicare Advantage Plans may offer more telehealth benefits than Original Medicare. These benefits can be available in a variety of places, and you can use them at home instead of going to a health care facility. Check with your plan to see what additional telehealth benefits it may offer.
What are the changes to Medicare Telehealth?
The federal government announced a series of policy changes that broaden Medicare coverage for telehealth during the COVID-19 public health emergency. Some important changes to Medicare telehealth coverage and reimbursement during this period include: 1 Location: No geographic restrictions for patients or providers 2 Eligible providers: All health care providers who are eligible to bill Medicare can bill for telehealth services, including Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) 3 Eligible services: See this list of telehealth services from the Centers for Medicare & Medicaid Services 4 Cost-sharing: Providers can reduce or waive patient cost-sharing (copayments and deductibles) for telehealth visits 5 Licensing: Providers can furnish services outside their state of enrollment. For questions about new enrollment flexibilities, or to enroll for temporary billing privileges, use this list of Medicare Administrative Contractors (MACs) to call the hotline for your area 6 Modality: Some telehealth services only require a telephone
Can a provider furnish services outside of their state of enrollment?
Licensing: Providers can furnish services outside their state of enrollment. For questions about new enrollment flexibilities, or to enroll for temporary billing privileges, use this list of Medicare Administrative Contractors (MACs) to call the hotline for your area.
Does Medicare cover telehealth?
The federal government announced a series of policy changes that broaden Medicare coverage for telehealth during the COVID-19 public health emergency. Some important changes to Medicare telehealth coverage and reimbursement during this period include: Location: No geographic restrictions for patients or providers.
Is TBHI a legal or ethical organization?
They are not intended to malign any organization, company or individual. TBHI does not, and cannot offer legal, ethical, technical, medical or therapeuitc advice.
Do seniors get telehealth?
This legislation would increase access to mental health services for millions of seniors, while at the same time, help lessen the shortage of America’s mental health provider population currently serving seniors. While mental health counselors and marriage and family therapists have the training and education to be licensed to provide services to mental health clients, they are not currently eligible for Medicare telehealth reimbursement. Therefore, seniors seeking their services have to pay out of pocket if they elect to see a counselor or marriage and family therapist.
Can a marriage and family therapist be telehealthed?
While mental health counselors and marriage and family therapists have the training and education to be licensed to provide services to mental health clients, they are not currently eligible for Medicare telehealth reimbursement.
How long does it take to see a provider in person for telehealth?
Contrary to common sense, Medicare recipients were required to see a provider in person within six months of getting telehealth services.
What is the Telemental Health Care Access Act of 2021?
The Telemental Health Care Access Act of 2021 is another step in breaking down barriers to telehealth treatment that started with legislation called the SUPPORT for Patients and Communities Act in 2018; that act removed various requirements for substance use disorder ...
Is TBHI a legal or ethical organization?
They are not intended to malign any organization, company or individual. TBHI does not, and cannot offer legal, ethical, technical, medical or therapeuitc advice.
