Full Answer
Did mutual of Omaha delay or wrongfully deny my claim?
If Mutual of Omaha delayed or wrongfully denied your disability insurance claim, the disability insurance lawyers and ERISA attorneys at DarrasLaw can help. We hold disability insurance companies accountable and ensure that policyholders are paid what they deserve.
Did mutual of Omaha pay out every insurance claim in 2016?
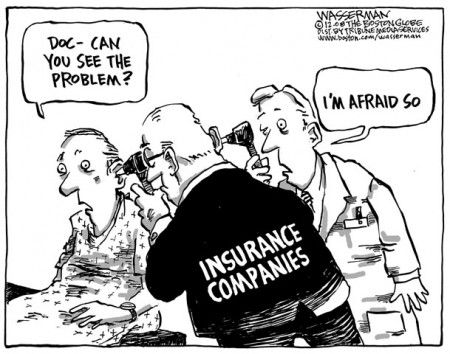
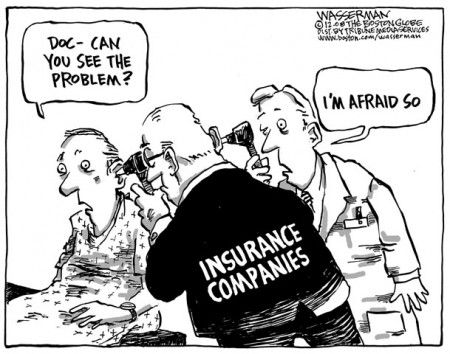
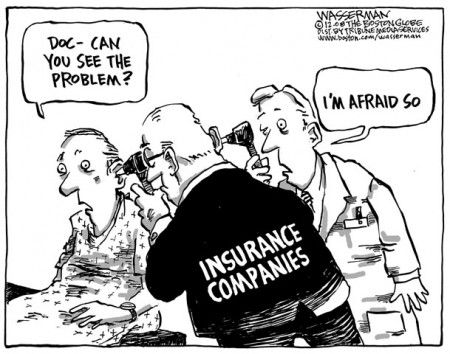
Mutual of Omaha did not earn a net income of $356.6 million in 2016 by gladly paying out every insurance claim. Mutual of Omaha may have wrongfully delayed or denied some policyholders’ claims for short-term (STD) or long-term (LTD) disability insurance benefits.
Did mutual of Omaha deny Egan’s claim?
Egan purchased an individual disability insurance policy with Mutual of Omaha; he later filed a disability claim under his policy. Mutual of Omaha denied Egan’s claim, stating that Mutual of Omaha’s own claims manager for Egan’s policy deemed the claim fraudulent. Egan brought suit against Mutual for bad faith and unfair dealing.
Can I receive disability insurance coverage through mutual of Omaha?
currently disabled, pregnant, awaiting a pending surgery, or recuperating from an illness, then you might be eligible to receive disability insurance coverage through Mutual of Omaha. Huge disability insurance carriers understand that they can often increase profits by denying legitimate claims or giving policyholders the runaround.
See more
Why can you be denied Medicare?
Medicare's reasons for denial can include: Medicare does not deem the service medically necessary. A person has a Medicare Advantage plan, and they used a healthcare provider outside of the plan network. The Medicare Part D prescription drug plan's formulary does not include the medication.
Can I be denied a Medicare Supplement plan?
For the most part, Medicare Supplement policies are guaranteed renewal. This means as long as you pay the monthly premium, you cannot be denied coverage once you enroll in a plan, regardless of any health conditions that may arise.
What is the rating for Mutual of Omaha health insurance?
In 2020, this small portion of the business with its 2,500 policies was sold to Essence Healthcare. Mutual of Omaha is a financially strong company and is rated A+ (Superior) by AM Best. This means you can feel confident that the company will be able to pay claims.
Is Mutual of Omaha the same as Medicare?
Unlike many Medigap insurers, Mutual of Omaha doesn't sell Medicare Advantage or other health insurance plans. The company specializes in insurance meant to complement your main health insurance, such as Medicare Supplement Insurance, life insurance and long-term care insurance.
Can I be turned down for Medicare Part D?
To disenroll from a Medicare drug plan during Open Enrollment, you can do one of these: Call us at 1-800 MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Mail or fax a signed written notice to the plan telling them you want to disenroll.
When can someone enroll in a Medicare Supplement without the chance for denial premium increase or exclusions due to pre-existing conditions?
six monthsEnrollment Periods for Medicare Supplement Insurance Plans You have six months to sign up for a plan. Insurance companies cannot deny coverage or charge more for a pre-existing condition during your open enrollment period.
Is Mutual of Omaha a good Medicare provider?
The company has been involved with Medicare since it was first introduced, and was selected to administer Original Medicare (Part A and Part B) in 1966. With such an impressive track record, it's no surprise that Mutual of Omaha's reputation as a Medicare plan provider is among the best.
Does Mutual of Omaha pick up Medicare deductible?
Mutual of Omaha has you covered It's a great option to add to your existing Medicare Part A and B plans, as Medicare supplement insurance helps cover some out-of-pocket costs that Part A and Part B may leave you with. These include expenses like copays, coinsurance, and deductibles.
Is Mutual of Omaha a good company?
The ratings agency AM Best gives Mutual of Omaha an A+ for financial stability, which is the second-highest rating and means the company has a “superior” ability to take care of its contractual insurance obligations, like paying claims.
Does Mutual of Omaha follow Medicare guidelines?
Mutual of Omaha has been providing Medicare Supplement insurance since Medicare started in 1966 – more than 52 years ago. You can count on us for a great Medicare plan, and for the support you need to choose your perfect coverage.
What is the highest rated Medicare Supplement company?
Best Medicare Supplement Insurance Companies of 2022Best Overall: Mutual of Omaha.Best User Experience: Humana.Best Set Plans and Coverage: AARP.Best Medigap Coverage Information: Aetna.Best Discounts for Multiple Policyholders: Cigna.
Does Mutual of Omaha plan g cover Medicare deductible?
Medicare Part A Deductible Medigap Plan G from Mutual of Omaha will cover the full cost of this deductible, no matter how many benefit periods you experience in a single year. This can potentially save you a lot of money if you're hospitalized even just once in a year, much less if you're hospitalized several times.
What happens if Mutual of Omaha denies your claim?
If Mutual of Omaha denied your claim, the statute of limitations clock is running for your appeal and/or lawsuit. You must act quickly, or you will risk running out of time to appeal or sue on your disability insurance denial—possibly foreclosing your ability to receive benefits for your claim permanently.
What was the reason for Radecki v. Mutual of Omaha?
Radecki sued Mutual of Omaha for bad faith and breach of contract, and a jury ultimately decided the case. The jury returned a verdict in favor of Radecki on the breach of contract cause of action and awarded Radecki damages equal to 24 months of disability benefits. An appeals court later upheld the judgment.
How much did Mutual of Omaha make in 2016?
Mutual of Omaha did not earn a net income of $356.6 million in 2016 by gladly paying out every insurance claim. Mutual of Omaha may have wrongfully delayed or denied some policyholders’ claims for short-term (STD) or long-term (LTD) disability insurance benefits. If you are between the ages of 18 and 61; you work at least 30 hours per week;
Why was Tadeusz Radecki denied?
Mutual of Omaha denied Radecki’s claim, because it disputed whether he became totally disabled while covered by the policy.
How long does Mutual of Omaha last?
Maximum monthly base benefit is $12,000 to $15,000. Elimination period—from 30 to 365 days. Benefit period—from 2 to 10 years, or to age 67. A level premium rate until age 67.
Does Mutual of Omaha offer disability?
Mutual of Omaha generally offers both total and partial disability income benefits in its base policy. Mutual of Omaha generally provides the following short-term disability insurance: A monthly benefit, based on a portion of your current income. Maximum monthly base benefit is generally $5,000. Elimination period—ranges from 0 to 90 days.
Do insurance companies win when the insured fails?
Insurance companies win when the insured fails or can’t fight back. Over the years, DarrasLaw’s clients have fought back and won against every major disability insurance company. Mutual of Omaha, like all major disability insurance companies has an obligation to act in good faith when you present a claim for disability.
What to do if your Mutual of Omaha life insurance claim is denied?
If your Mutual of Omaha life insurance claim was denied you need to speak to us at the Center for Life Insurance Disputes. We get more denied life insurance claims paid than any other firm. Over $60 million recovered for our clients and no down payment is ever required.
Does Mutual of Omaha pay death claims?
Mutual of Omaha doesn’t want to pay death claims if they don’t have to. You need hard evidence and you need to know what to do with it if you’re going to get a denied life insurance claim paid.
What is the phone number for Mutual of Omaha?
If you have any questions, please contact Mutual of Omaha Rx at 855-864-6797. Customer Service is available 24 hours a day, 7 days a week. TTY users should call 800-716-3231. Attention. You are about to leave the Mutual of Omaha Rx plan site.
What is the phone number for Medicare appeals?
Clinical and Administrative Appeals. Use this contact information if you need to file an appeal if your coverage review is denied. Call toll free 844-374-7377, Monday through Friday, 8 a.m. - 8 p.m. TTY users: call 800-716-3231. Mutual of Omaha Rx. Attn: Medicare Appeals.
What is the number to call for Medicare?
Call toll free 800-413-1328, Monday through Friday, 8 a.m. - 6 p.m., Central. TTY users: call 800-716-3231. Mutual of Omaha Rx. Attn: Medicare Administrative Department.
Can you ask for drug coverage if it is not on the formulary?
You can ask us to cover your drug even if it is not on our formulary. Please note, if we grant your request to cover a drug that is not on our formulary, you may not ask us to provide a higher level of coverage for the drug. You can ask us to waive coverage restrictions or limits on your drug.
Can you ask Mutual of Omaha RX to make an exception to Medicare Part D?
As a member, you can ask Mutual of Omaha Rx to make an exception to our Medicare Part D coverage rules. There are several types of exceptions that you can ask us to make.
What is Medicare Supplement Insurance?
A: Medicare supplement insurance (Medigap) is a private form of medical insurance that covers some Medicare out-of-pocket costs. A policy can help pay for Medicare deductibles, co-payments, co-insurance and other costs.
What is Medicare for seniors?
A: Medicare is a federal health insurance program that provides affordable health care options for seniors 65 and older, disabled citizens, and those suffering from ESRD.
How many Medigap plans are there?
A: There are 10 different Medigap plans currently available for purchase in most states: Plans A, B, C, D, F, G, K, L, M and N. Each plan offers a different array of benefits. Insurance companies must offer the same benefits for each plan option. For example, one insurer’s Plan G will have the same benefits as another insurer’s Plan G. The only difference between the two companies’ policies is price.
What is the pricing structure of Medigap?
There are 3 types of pricing structures: attained-age pricing, community-rated pricing, and issue-age pricing. If your policy is attained-age, the premium will increase as you age.
Do insurance companies have the same benefits?
Insurance companies must offer the same benefits for each plan option. For example, one insurer’s Plan G will have the same benefits as another insurer’s Plan G. The only difference between the two companies’ policies is price.
Does your insurance premium increase as you age?
If your policy is attained-age, the premium will increase as you age. If your policy is issue-age, the premium will not increase as you age but can increase based on other factors. If your policy is community-rated, the premium can increase based on inflation.
Does Medigap cover prescription drugs?
A: Medigap policies do not provide prescription drug coverage. Medigap plans stopped providing prescription drug coverage in 2006. If you are enrolled in a Medigap policy, you can get prescription drug coverage through Medicare Part D.
Mutual of Omaha has you covered
Since 1909, we’ve existed as a Mutual company serving for the benefit and protection of our customers. Which means we don’t answer to Wall Street, we answer to you.
Ready to take the next step?
See what our customers are saying about us or get a quote from the products available in your state.
What is Medicare Part A?
Medicare Part A provides coverage for inpatient care, inpatient nursing care and inpatient services. Medicare Part B includes health care coverage for doctors’ services, outpatient care and preventative services. Plus, if your doctor accepts Medicare, you may be able to keep seeing them. You may even be able to enroll in Original Medicare ...
How long does it take to get Medicare Supplement insurance?
The OEP for Medicare Supplement Insurance is the 6-month period after the first month you’re 65 and have Medicare Part B health care coverage. If you apply during this window, your Medigap plan can’t deny you health care coverage.
What is pre-existing condition?
Pre-existing conditions are health conditions that you had before the start date of your new health care coverage. You have “guaranteed issue rights” with Medicare. This means all plans must cover you for pre-existing conditions as long as you enroll when you’re first eligible for Medicare. If you miss this initial enrollment period, your Medicare ...
When does Medicare enrollment start?
The General Enrollment Period is January 1 through March 31 every year. If you enroll during this timeframe, your coverage starts July 1 of that year. There are special enrollment periods (SEPs) for Medicare Part A and Part B, as well as for Medicare Advantage and Part D (prescription drug plan).
When is the open enrollment period for Medicare?
The open enrollment period is each year, from October 15 to December 7.
Can you enroll in Medicare Advantage if you have end stage renal disease?
You won’t be able to enroll in some Medicare Advantage plans if you have end-stage renal disease (ESRD). 2. If you do have a chronic, pre-existing condition like ESRD, you may be able to enroll in a Medicare Advantage Special Needs Plans (SNP). You may qualify if you have: Alcoholism. Drug addiction.
Can Medicare Part D be denied?
Medicare Part D plans can’t deny you coverage based on your medical history, or because of what prescription drugs you’re taking. However, Medicare Part D is not included in Original Medicare. You have to enroll separately.