Does Medicare accept the CMS 1500 claim form?
Who can use the CMS 1500 form to bill to Medicare?
Is CMS 1500 only for Medicare?
What is a CMS 1500 form how is it used for billing?
How do I submit a medical claim to Medicare?
Can I submit a claim directly to Medicare?
What does Medicare allowed mean?
When a provider does not accept assignment from Medicare the most that can be charged to the patient is ____ percent of the Medicare approved amount?
What plan provides both Medicare and Medicaid coverage to certain eligible beneficiaries?
What is the difference between a Superbill and CMS 1500?
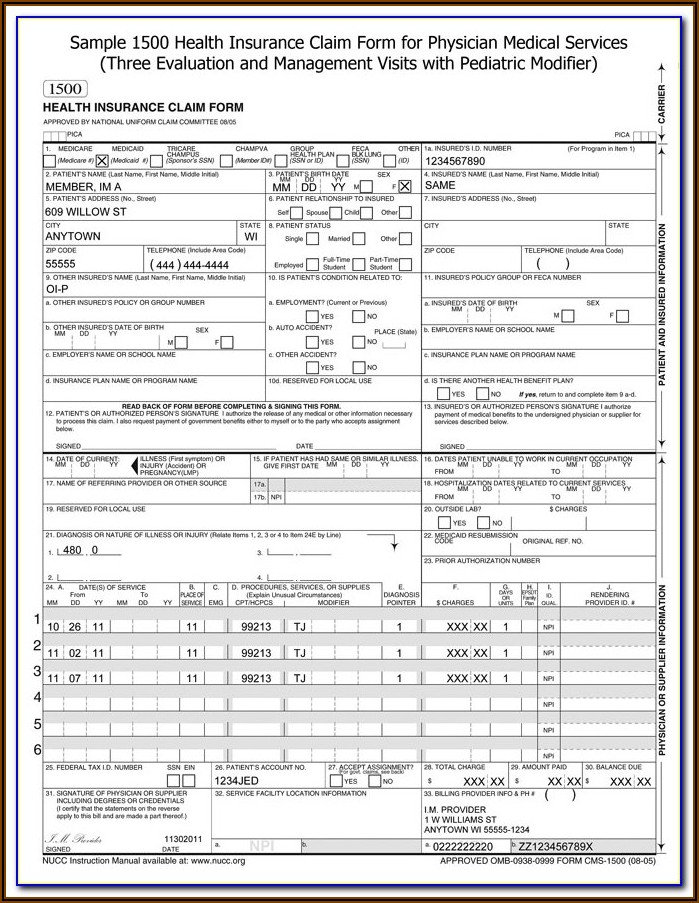
What information is needed to fill out a CMS 1500 claim form?
- The type of insurance and the insured's ID number.
- The patient's full name.
- The patient's date of birth.
- The insured's full name, if applicable.
- The patient's address.
What does an insurance claim do?
What is Medicare claim processing manual?
The Medicare Claims Processing Manual (Internet-Only Manual [IOM] Pub. 100-04) includes instructions on claim submission. Chapter 1 includes general billing requirements for various health care professionals and suppliers. Other chapters offer claims submission information specific to a health care professional or supplier type. Once in IOM Pub. 100-04, look for a chapter(s) applicable to your health care professional or supplier type and then search within the chapter for claims submission guidelines. For example, Chapter 20 is the Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS).
What is MSP in Medicare?
MSP provisions apply to situations when Medicare isn’t the patient’s primary health insurance coverage.MSP provisions ensure Medicare doesn’t pay for services and items that pertain to other health insurance or coverage that’s primarily responsible for paying. For more information, refer to the Medicare Secondary Payer
What is the 837P?
The 837P is the standard format used by health care professionals and suppliers to transmit health care claims electronically. The Form CMS-1500 is the standard claim form to bill MACs when a paper claim is allowed.
What is the 10th revision of the ICd 10?
The International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM),is used to code diagnostic information on claims. Visit the Centers for Disease Control and Prevention website to access ICD-10-CM codes electronically or you may purchase hard copy code books from code book publishers.
What is the Administrative Simplification Compliance Act?
The Administrative Simplification Compliance Act (ASCA) mandates the submission of electronic claims to Medicare unless a supplier meets certain "exceptions" described within the law. View exceptions on the Administrative Simplification Compliance Act Self Assessment webpage.
What is OCR in Noridian?
Noridian uses optical character recognition (OCR) to process paper CMS-1500 claim forms. OCR is a means of inputting text into a computer. It involves scanning a paper document to create a digital image of the text and then using software to store knowledge about that digital image. With OCR, it is very important suppliers follow proper paper claim ...
What is OCR scanning?
It involves scanning a paper document to create a digital image of the text and then using software to store knowledge about that digital image. With OCR, it is very important suppliers follow proper paper claim submission guidelines.
Is Noridian handwritten?
To ensure timely and accurate processing of claims, Noridian recommends claims be typed, not handwritten.
What is OCR in computer?
OCR is a means of inputting text into a computer. It involves scanning a paper document to create a digital image of the text and then using software to store knowledge about that digital image. With OCR, it is very important suppliers follow proper paper claim submission guidelines.
What does "yes" mean in Medicare?
Check "Yes" or "No" to indicate whether employment, autoliability, or other accident involvement applies to one or more of the services listed in block 24. A "yes" answer indicates there may be other insurance primary to Medicare. This is an important field. This is the place to indicate that a good faith effort has.
What is invalid claim?
INVALID CLAIMS. 1) An invalid claim is one that has illogical or incorrect information on it. 2) An example would be a claim in which the patient's sex does not correlate with the procedure (a hysterectomy and a male patient), or in which the provider number does not match the provider. name.
What is pending claim?
PENDING CLAIMS. 1) A pending claim (or suspended claim) is one that has been put on hold because either an error has. occurred, or there is a need for additional information. 2) Many times claims are pending when additional information is needed from the patient by the.
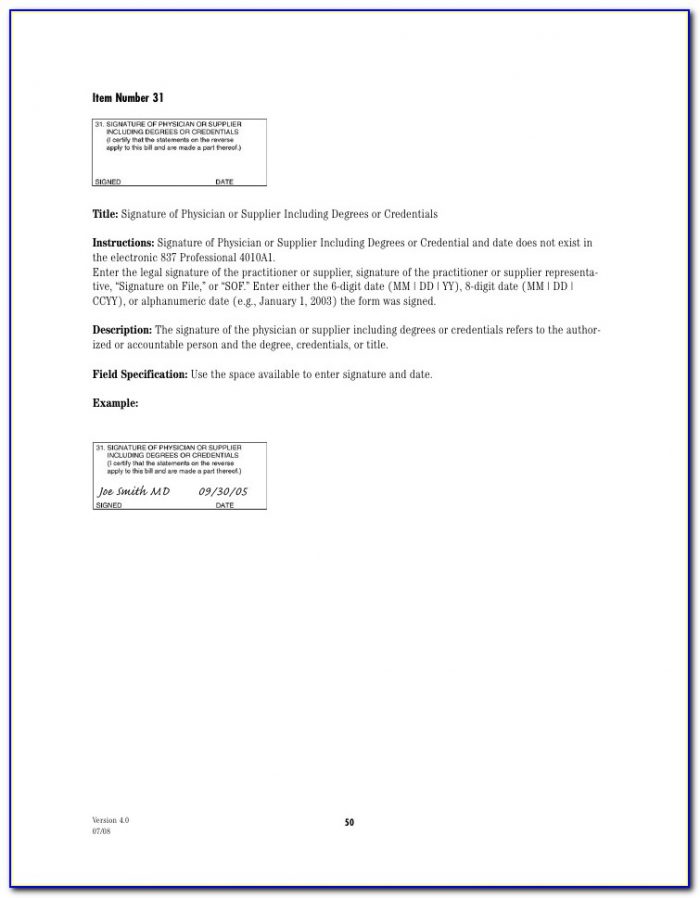
What is a signature on file?
A signature on file or a computer-generated signature can also be used. The patient's signature authorizes release of information necessary to process the claim. This signature authorizes payment of benefits to the provider or supplier. A signature on file is acceptable here.
What is audit trail?
2) Audit trails allow for the verification of where a claim was sent, and who processed the claim, so the status of the claim can be closely followed. 3) Audit trails also provide the information to create an insurance aging report, or other printable reports to help make the process of following up on claims easy.