In order to be eligible for a Medicare Supplement
Medigap
Medigap refers to various private health insurance plans sold to supplement Medicare in the United States. Medigap insurance provides coverage for many of the co-pays and some of the co-insurance related to Medicare-covered hospital, skilled nursing facility, home health care, ambulance, durable medical equipment, and doctor charges. Medigap's name is derived from the notion that it exists to …
Full Answer
When does my Medicare coverage start?
Jan 01, 2022 · The date your coverage starts depends on which month you sign up during your Initial Enrollment Period. Coverage always starts on the first of the month. If you qualify for Premium-free Part A: Your Part A coverage starts the month you turn 65. (If your birthday is on the first of the month, coverage starts the month before you turn 65.)
How does Medicare supplement insurance work with Medicare?
Mar 11, 2022 · *While seniors may enroll in Medicare three months before they turn 65, the Medicare Supplement Open Enrollment Period does not begin until you are both 65 or older and enrolled in Medicare Part B. If you are enrolled in Medicare Part B on the date you turn 65, that is the day your Medicare Supplement Open Enrollment Period begins.
Are you eligible for a Medicare supplement plan?
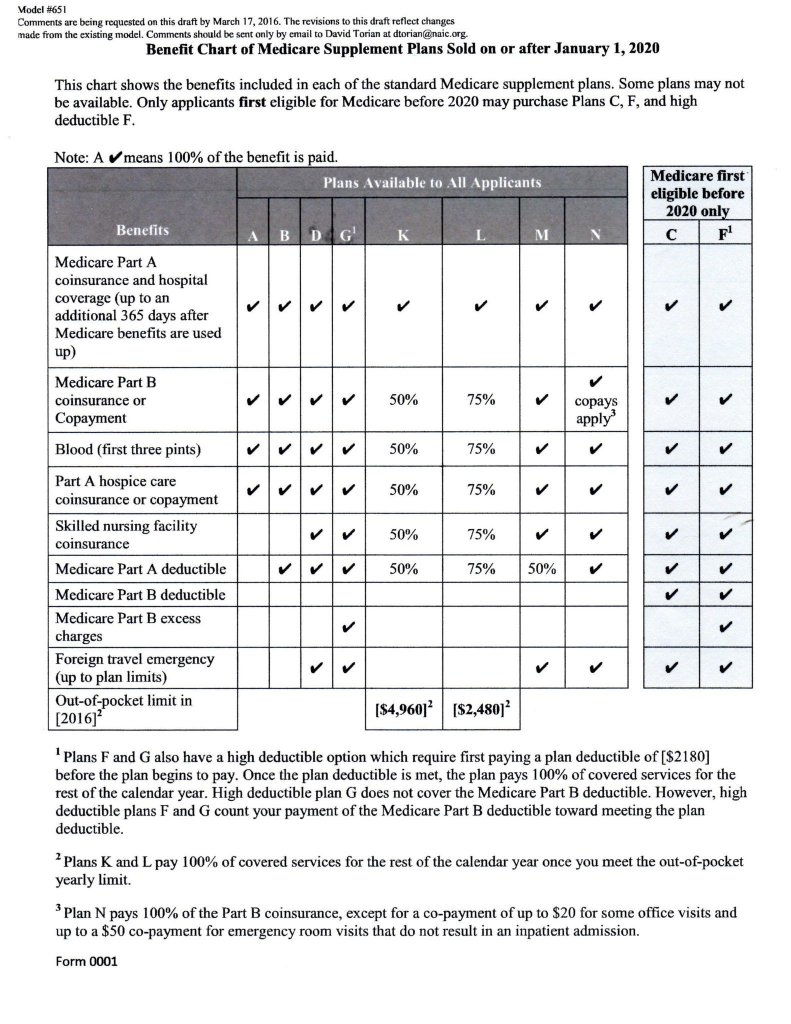
However, if you were eligible for Medicare before January 1, 2020, but not yet enrolled, you may be able to buy one of these plans that cover the Part B deductible (Plan C or F). If you already have or were covered by Plan C or F (or the Plan F high deductible version) before January 1, 2020, you can keep your plan.
When does Medicare Part A or Part B start?
Days 91 and beyond: $658 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime) Beyond lifetime reserve days: all costs. Part A skilled nursing facility stay. You pay: Days 1-20: $0 for each benefit period. Days 21-100: $164.50 per day of each benefit period.

What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
Can you cancel a Medigap policy?
This means the insurance company can't cancel your Medigap policy as long as you pay the premium. Some Medigap policies sold in the past cover prescription drugs. But, Medigap policies sold after January 1, 2006 aren't allowed to include prescription drug coverage.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible.
Why Us?
The Medicare Network exists to ensure that the Medicare program works smoothly for seniors nationwide.
Is the Medicare Network right for you?
For those who are unsure if our services and information are what they want, read through the questions below. If you answer yes to any of them, then chances are, you could use our help;
2018 Costs at a Glance
Most people don't pay a monthly premium for Part A (sometimes called "premium-free Part A"). If you buy Part A, you'll pay up to $413 each month.
What is Medicare for people 65 and older?
Medicare. Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD) and. group health plan.
What is a group health plan?
group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families. (retiree) coverage from a former employer, generally Medicare pays first for your health care bills, and your. group health plan. In general, a health plan offered by an employer ...
How old do you have to be to get Medicare Supplement?
In order to be eligible for a Medicare Supplement plan, you either need to be 65 years old or have a disability or end stage renal disease. Those medical conditions allow you to qualify for Medicare before you turn 65, and if you think you may qualify, but you are not sure, then you can always contact a Medicare insurance agent to find out.
How to add more overage to Medicare?
You can add more overage onto your existing basic Medicare plan by signing up for supplemental insurance for Medicare. This is insurance that is meant to extend your current coverage and take care of medical expenses not covered under the original plan.
What is Medicare Supplement Insurance?
Medicare supplement insurance is private insurance that fills in the gaps left by Medicare. For instance, when you have a hospital or doctor bill, Medicare pays its approved amount first, then the supplemental insurance pays other costs, such as deductibles and copays.
What is the age limit for Medicare Supplement?
Medicare Supplement Coverage. If you are 65 , you are eligible for Medicare. As you approach your 65 th birthday, you should consider applying for Medicare. Opens In A New Window. . There are two types of Medicare: original Medicare and Medicare Advantage.
Does Medicare Advantage require you to use a doctor?
Medicare Advantage might require you to use certain doctors and hospitals. Prescription drug coverage is available under Medicare Part D. Prescription drug benefits are included in some Medicare Advantage plans but otherwise must be purchased separately.
Who runs Medicare approved health plans?
These Medicare-approved health plans are run by private insurance companies and provide benefits for hospital, doctor, and other health care provider services covered under Original Medicare Parts A and B as well as supplemental benefits that vary by plan. The insurer receives money from Medicare and may also charge you a premium in some cases, ...
Does Medicare cover my spouse?
Your policy will not cover your spouse. Choosing the right Medicare supplement plan can be complicated. There are a number of questions to ask.
Does Medicare Supplement Plan A have the same benefits?
All insurance companies must offer the same benefits under a given plan. In other words, Medicare Supplement Plan A will have the same benefits regardless of which company sells it. However, the premium you pay for that plan may differ from one company to another.
When does Medicare change coverage?
You can’t use this Special Enrollment Period from October–December. However, all people with Medicare can make changes to their coverage from October 15–December 7, and the changes will take effect on January 1.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles).
What is a special enrollment period?
Special circumstances (Special Enrollment Periods) You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).
What can I do with my Medicare Advantage Plan?
What can I do? Join a Medicare Advantage Plan with drug coverage or a Medicare Prescription Drug Plan. Switch from your current plan to another Medicare Advantage Plan with drug coverage or a Medicare Prescription Drug Plan. Drop your Medicare Advantage Plan with drug coverage and return to Original Medicare .
How long does it take to switch plans after moving?
If you tell your plan before you move, your chance to switch plans begins the month before the month you move and continues for 2 full months after you move. If you tell your plan after you move, your chance to switch plans begins the month you tell your plan, plus 2 more full months.
What to do if you made wrong choice on Medicare?
Call center representatives can help you throughout the year with options for making changes.
What happens after you pay a deductible?
After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). . Drop your Medicare prescription drug coverage.
How long does Medicare coverage last?
This special period lasts for eight months after the first month you go without your employer’s health insurance. Many people avoid having a coverage gap by signing up for Medicare the month before your employer’s health insurance coverage ends.
What is a small group health plan?
Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage a small group health plan. If your employer’s insurance covers more than 20 employees, Medicare will pay secondary and call your work-related coverage a Group Health Plan (GHP).
Does Medicare pay second to employer?
Your health insurance through your employer will pay second and cover either some or all of the costs left over. If Medicare pays secondary to your insurance through your employer, your employer’s insurance pays first. Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance ...
Does Medicare cover health insurance?
Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance coverage in different ways. If your company has 20 employees or less and you’re over 65, Medicare will pay primary. Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage ...
Can an employer refuse to pay Medicare?
The first problem is that your employer can legally refuse to make any health-related medical payments until Medicare pays first. If you delay coverage and your employer’s health insurance pays primary when it was supposed to be secondary and pick up any leftover costs, it could recoup payments.