So, for example, if you completed 17 minutes of treatment, Medicare would be billed for 15 minutes, or one unit. However, if you completed 23 minutes of treatment, Medicare would be billed for two units of treatment. The bill would still be for two units regardless of whether you spent 23 or 30 minutes with the patient.
Full Answer
How does Medicare billing for physical therapy work?
Physical therapy billing guidelines for Medicare and Medicaid services include a section about how much time you must spend with a patient for it to be “bill-worthy.” Medicare physical therapy billing works in increments of 15. So what are you supposed to do when your treatment only takes 13 minutes to complete?
What is the 8-minute rule for Medicare physical therapy billing?
Medicare physical therapy billing works in increments of 15. So what are you supposed to do when your treatment only takes 13 minutes to complete? That’s where the eight-minute rule comes in. You only have to spend eight minutes with a patient to be able to bill for one “15-minute” unit.
Can I Bill for a re-evaluation?
To answer your question, this depends on the rules set forth by the payer. However, as we explain in this WebPT Blog post, per Medicare rules, you may bill for a re-evaluation if "you treat a patient with a chronic condition and you don’t see him or her for treatment very often."
Does your physical therapy practice need to Bill and collect payment?
But if you’re serious about helping people, your practice needs to be able to cover its costs (and yours), and that means billing and collecting payment for your services. Billing is an inevitable part of owning a physical therapy practice, but it doesn’t need to be complicated or overwhelming.
When should I charge a re eval for physical therapy?
Under Medicare guidelines, a re-evaluation is medically necessary (and therefore payable) only if the therapist determines that the patient has had a significant improvement, or decline, or other change in his or her condition or functional status that was not anticipated in the POC (emphasis added).
What is the KX modifier for Medicare?
The KX modifier, described in subsection D., is added to claim lines to indicate that the clinician attests that services at and above the therapy caps are medically necessary and justification is documented in the medical record.
How does Medicare reimburse physical therapy?
However, in 2018, the therapy cap was removed. Original Medicare covers outpatient therapy at 80% of the Medicare-approved amount. When you receive services from a participating provider, you pay a 20% coinsurance after you meet your Part B deductible ($233 in 2022).
Can physical therapists bill Medicare?
Physical therapy billing guidelines for Medicare and Medicaid services include a section about how much time you must spend with a patient for it to be “bill-worthy.” Medicare physical therapy billing works in increments of 15.
Is KX modifier for Medicare only?
Therapists should continue to affix the KX modifier to all medically necessary services above the designated limit ($2,010 in 2018), thus signaling Medicare to pay the claim. That means you must continue to track your patients' progress toward the threshold so you know when to affix the modifier.
What does the KX modifier indicate?
The KX modifier is a signal on a claim that though the patient services have met the capped amount allowed, the provider deems continued care medically necessary. As the description in the below table indicates, medical record documentation must be maintained to support the medical necessity of the continued services.
How many PT sessions will Medicare pay for?
There's no limit on how much Medicare pays for your medically necessary outpatient therapy services in one calendar year.
What are the CPT codes for physical therapy?
Common Physical Therapy CPT Codes29240, 29530, 29540: Strapping.97110: Therapeutic Exercise.97112: Neuromuscular Re-education.97116: Gait Training.97140: Manual Therapy.97150: Group Therapy.97530: Therapeutic Activities.97535: Self-Care/Home Management Training.More items...•
How do I find my Medicare fee schedule?
To start your search, go to the Medicare Physician Fee Schedule Look-up Tool. To read more about the MPFS search tool, go to the MLN® booklet, How to Use The Searchable Medicare Physician Fee Schedule Booklet (PDF) .
How does billing work in physical therapy?
How Does Therapy Billing Work?A bill is submitted to the patient, third-party payer directly, or a 'claims clearinghouse' that prepares the bill.The claims clearinghouse will submit the bill to the payer. ... Copayments are collected at the time of service.
Can a physical therapist Bill 97124?
Therapeutic Massage It's always important to check your state practice act, but in most cases, physical therapists can bill CPT code 97124 (massage therapy) when they provide therapeutic massage.
How many units can you bill for PT?
Per Medicare rules, you could bill one of two ways: three units of 97110 (therapeutic exercise) and one unit of 97112 (neuromuscular reeducation), or. two units of 97110 and two units of 97112.
How long does a physical therapist have to be on Medicare?
The rule stipulates that you need to provide direct treatment for a minimum of 8 minutes to be reimbursed by Medicare for a time-based code.
What happens if you are not credentialed by Medicare?
If you are not credentialed, you will not be allowed to treat or collect payment from Medicare patients, even if Medicare offers cover for those services.
What is an ABN for Medicare?
An Advance Beneficiary Notice of Noncoverage (ABN) is a signed declaration that the client will accept financial responsibility if Medicare (and it’s likely they will) denies the claim.
When did the therapy cap start?
Introduced in 1997 , the Therapy Cap caps physical therapy and speech therapy services at a yearly amount, which does not reset for each diagnosis. You need to monitor your clients’ cap and apply for an exemption if the client needs medical necessary care despite exceeding their cap.
Is physical therapy a profitable business?
Physical therapy practice owners in America have a lot going on from scheduling and treating clients, to running a profitable small business covering marketing, accounting, and much more. If you have to add keeping track of PT Medicare billing nuances to the list, it’s more than most therapists can handle.
Why do you need to bill for physical therapy?
But in order to stay in business long enough to actually make a difference in your patients’ lives, you absolutely must bill—and collect payment— for your services.
When will rehab therapist assistants be paid?
In the 2019 final rule, CMS announced that, beginning in 2022, it will only pay 85% of services performed either in full or in part by a rehab therapist assistant. Thus, beginning in 2020, if a PTA performs at least 10% of a given service, then you must affix the CQ modifier to the claim line for that service, notifying Medicare about the assistant’s participation in the service. That said, payment reductions won’t occur until two years later.
What software do providers use to submit claims?
Software. A lot of providers use a billing software to prepare and submit their claims. The really smart ones use an electronic medical record system that includes (or integrates with) a top-notch therapy billing software (hello, WebPT ).
When to use modifier 59?
Practices and facilities that offer their patients both physical and occupational therapy may need to affix modifier 59 or modifier XP to claims when patients receive same-day services that form NCCI edit pairs. According to Castin, modifier XP would be appropriate if, say, “an OT takes over treatment in the middle of a PT session” and modifier 59 would be appropriate if the payer doesn’t yet recognize X modifiers or there’s another reason to provide “otherwise linked services that should, given the circumstances, be reimbursed separately.” For example, you would use modifier 59 if, say, a PT provides gait training (97116) and an OT provides therapeutic activity (97530). As such, you’re notifying Medicare that the services—97116 and 97530—were performed separately and distinctly from one another and thus, should both be paid.
What is the most common claim form?
However, some payers—a dwindling few—do still accept paper ones. The most common form is the Universal Claim Form ( CMS 1500 ), although some payers may request that you use their own.
What is CPT medical?
Developed by the American Medical Association (AMA), the Current Procedural Terminology (CPT®) is “the most widely accepted medical nomenclature used to report medical procedures and services under public and private health insurance programs.”.
How long does it take for a physician to sign a plan of care?
Initial certification: Medicare requires ordering physicians to “approve or certify the plan of care via signature in a timely manner (within 30 days of the evaluation).”. The initial certification covers the first 90 days of treatment.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
Therapy evaluation and formal testing services involve clinical judgment and decision-making which is not within the scope of practice for therapy assistants.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
How long is Medicare billing?
When billing timed CPT codes, Medicare not only looks at the individual 15-minute units but also considers the total time when factoring the allowable payment. This is commonly known as the 8-23-minute rule.
What does Medicare expect from you?
Medicare expects you to evaluate the patient, determine their rehabilitation needs and address those needs. One of those inaccurate impressions is the belief the patient must be making objective progress in order to continue with rehabilitation.
What does the KX modifier mean for PT?
The KX modifier simply indicates to Medicare that specific treatment continues to be medically necessary and requires the skills of the PT/OT in order to continue towards meeting the patient’s goals. This serves as a mental check on whether the care continues to be reasonable and necessary.
How did Medicare come into existence?
Medicare came into being through legislation, signed into law by President Lyndon Johnson, as part of the Social Security Amendments of 1965. It’s funded by payroll deductions as an addition to your Social Security deductions (FICA) as well as premiums paid for those receiving Part B benefits.
What is important about Medicare?
One of the more valuable things about Medicare is they tell you exactly what they are looking for in their documentation requirements. For starters, documentation must support the medical necessity of the care provided. This means your notes must be comprehensive enough and contain sufficient detail so anyone reviewing the medical record may easily see what you are treating and why you are providing that specific treatment. They should also be able to easily see if there is progress towards achieving the patient’s functional goals.
Is it better to audit Medicare or defend?
Of course, the best defense is a good offense. Setting your practice up to comply with the Medicare rules is much better than having to address an audit. To audit proof yourself, be sure you know the rules and regulations on document/billing and fully comply.
Does Medicare cover OT care?
Medicare will cover maintenance care provided the level of care needed to maintain a certain level of function requires the skills (knowledge) of a physical or occupational therapist. In short, the complexity of the care must not be able to be completed by a family member, aide or anyone other than a PT/OT. Another misperception relates ...
How many minutes of therapy do you need for Medicare?
The 8-Minute Rule. The 8-Minute rule as known as “the eight rule” specifies how many support unit therapists will bill Medicare for the given service date. In order to obtain reimbursement from Medicare for a time-based code, you must have direct treatment for at least eight minutes, according to the law. However, although it sounds basic, there ...
When is a POC change required?
Change into the POC is required if the patient is unable to respond to the treatment given in the current POC. You discover additional clinical findings in the course of treatment, which are somehow similar to the original treating condition.
What is co-treatment in a therapist?
The American Occupational Therapy Association (AOTA), American Physical Therapy Association (APTA), and American Speech-Language-Hearing Association (ASHA), designed combined guidelines for Medicare Part A and Part B, which states that therapists should only co-treat a patient to have direct benefits to a patient.
What is an ABN in Medicare?
ABNs. Patients should sign an Advance Beneficiary Notice of Noncoverage (ABN) in order to offer Medicare patients services that they consider are not covered by Medicare or not required medically. This means that the patient will bear the financial cost of treatment if claims are declined by Medicare. Tags.
What is the therapy cap?
The Therapy Cap. The therapy cap was planned as a provisional solution to regulate Medicare costs and was announced as part of the Balanced Budget Act (BBA) of 1997. Despite a long-term force to cancel the cap, Congress lasted to renew the cap every year from its establishment.
What does the GA modifier mean on a claim?
If you declare an ABN because you think that specific services are not reasonable and medically required, then the GA modifier should be incorporated into the claim to indicate that you have an ABN on file.
Can you waive copays?
Copays. If he or she is expected to pay a copayment through your patient’s policy, you can receive the payment when you offer your services. In most cases, waiving copayments or deductibles isn’t a good idea. There are however other avenues in which you can offer support to patients in need.
What is a re-evaluation in Medicare?
The AOTA describes a re-evaluation as the “reappraisal of the patient’s performance and goals to determine the type and amount of change that has taken place. Medicare and other third-party payers may have particular rules about when a re-evaluation may be reimbursed.
Why are therapists uncertain about re-evaluation?
Therapists are understandably uncertain as to when a re-evaluation can be billed because of conflicting terminology and confusion with “reassessment” requirements in PT and OT Acts. To determine if and when a re-evaluation is billable, we need to look at all of the following rules:
What is the AMA CPT?
In sum, the AMA CPT descriptions provide the basics of when a re-evaluation may be billed and what must be included in a PT and OT re-eval. You should note that Medicare and other payers can and sometimes do impose additional conditions that must be met to be paid for a reevaluation.
What is the time required for a standardized patient assessment?
2. Revised plan of care using a standardized patient assessment instrument and/or measurable assessment of functional outcome. Typically, 20 minutes are spent face-to-face with the patient and/or family.
Does Tricare have a re-eval?
The major commercial payers and Tricare do not have any unique guidance regarding re-evals. Their PT/OT policies basically include the AMA’s CPT descriptions for 97164 and 97168 if they include anything at all. Medicare’s more restrictive re-evaluation rules do not necessarily apply to these payers.
Is a re-evaluation required by Medicare?
Under Medicare guidelines, a re-evaluation is medically necessary (and therefore payable) only if the therapist determines that the patient has had a significant improvement, or decline, or other change in his or her condition or functional status that was not anticipated in the POC (emphasis added).
How long do you have to bill Medicare for therapy?
According to the rule, you must provide direct treatment for at least eight minutes in order to receive reimbursement from Medicare for a time-based code. But, while it sounds simple, there are some tricky 8-Minute Rule scenarios that could trip you up.
What is billable time?
1. Billable Time. To put it simply, billable time is time spent treating a patient. However, there are some nuances to keep in mind. For instance, you can’t bill for: unskilled prep time, multiple timed units due to multiple therapists, rest periods or other break times, supervision, or.
What is an ABN in Medicare?
In order to provide Medicare patients with services that you believe are either not covered by Medicare or not medically necessary (e.g., the services extend beyond the therapy cap ), you must have your patient sign an Advance Beneficiary Notice of Noncoverage (ABN), thereby indicating that he or she will accept financial responsibility if—but really more like when—Medicare denies the claim.
What is one on one therapy?
A one-on-one service is an individual therapy service—one that involves direct, one-on-one contact with a patient. While a group service still requires constant attendance, it does not involve one-on-one contact with each patient. Rather, according to CMS, it “consists of simultaneous treatment to two or more patients who may or may not be doing the same activities.”
Can you round up your billable time?
Additionally, when calculating your billable time, you shouldn’t ever round up . However, you can bill for evaluations and reevaluations—in some cases. Most payers, including Medicare, allow therapists to bill for the initial evaluations necessary to establish plans of care.
Can you waive copays?
If your patient’s insurance requires him or her to pay a copay, you can collect that payment when you provide your services. In most cases, it is not a good idea to waive copayments or deductibles. However, there are other ways you can provide financial assistance to patients who need it. To learn more about what your payers consider acceptable when it comes to helping patients cover the cost of your services, thoroughly read your insurance contracts. If you still come up empty-handed, contact your payers directly.
Can a therapist bill Medicare Part A?
However, therapists who bill under Medicare Part A may bill separate, full treatment sessions with a patient —as long as each therapist is of a different discipline and provides different treatments to the same patient at the same time. For clarity on billing for co-treatment—and a few examples—check out this resource. 4.
How long does Medicare bill for physical therapy?
Understanding the Medicare 8-Minute Rule for Physical Therapy Billing. Medicare has certain rules and regulations in place to prevent fraud, waste, and abuse. Here’s one you may not have heard of – the 8-minute rule. Providers must treat patients for at least eight minutes to receive Medicare reimbursement.
How many units of Medicare would you be billed for if you completed 23 minutes of treatment?
However, if you completed 23 minutes of treatment, Medicare would be billed for two units of treatment. The bill would still be for two units regardless of whether you spent 23 or 30 minutes with the patient.
What is CPT code?
As you may know, CPT codes are medical codes that describe the procedures and services you are performing to billing agencies and insurance companies. They were created by the American Medical Association in 1966 to simplify and standardize procedural reporting.
How long do you have to be on Medicare for treatment?
The 8-minute rule states that to receive Medicare reimbursement, you must provide treatment for at least eight minutes. Using the “rule of eights,” billing units that are normally based on 15-minute increments spent with a patient can be standardized.
How many minutes of manual therapy are there on Medicare?
However, you have two “remaining” minutes from the physical exercise and six “remaining” minutes from the manual therapy. Together, you have eight minutes, which would push you into the next billing unit. Medicare guidelines would allow you to bill for three units in that circumstance.
How many billing units can you bill for 45 minutes?
Technically, you’ve just spent 45 minutes with the patient, which would equate to three billing units. However, those first 25 minutes only counted for one unit because you were not in the room for the whole time, and you were not performing one undivided task. Therefore, you can only bill for two units.
How long do you have to bill for a 15 minute unit?
You only have to spend eight minutes with a patient to be able to bill for one “15-minute” unit. However, if you spend 16 minutes with a patient, you’ll still only be able to bill for one unit. You’d have to spend 23 minutes (15 + 8) with a patient to be able to fall into the two-unit bracket.
A Current Patient Develops A Newly Diagnosed, Related Condition.
A Current Patient Develops A Newly Diagnosed, Unrelated Condition.
- Use: Initial Evaluation (97161–97163) Conversely, when a patient with an active plan of care presents with a second condition that is totally unrelated to the primary issue, you should select the appropriate initial evaluation code. The nuance for therapists to remember is that a re-evaluation is triggered by a significant clinical change in the condition for which the original pla…
A Patient Undergoes Surgery Mid-Plan of Care.
- Use: Re-evaluation (97164) Re-evaluations also may be appropriate for patients who received therapy treatment prior to surgery and then returned for additional rehabilitation after surgery. The catch in this situation is that some commercial payers may consider the post-op treatment period a new episode of care, in which case you’d need to use an evaluation code. Example: You treat …
Introduction
What Are The Codes?
- The International Classification of Diseases
In order to successfully bill for your services, you’ll need to diagnose your patients’ conditions in a manner that demonstrates the medical necessity of those services—and you’ll need to do so using the latest version of the International Classification of Diseases (ICD), which, as of October 2015… - The Current Procedural Terminology
Developed by the American Medical Association (AMA), the Current Procedural Terminology (CPT®) is “the most widely accepted medical nomenclature used to report medical procedures and services under public and private health insurance programs.” According to the …
What’s The Terminology?
- Looking for a refresher on your billing terminology? Here are some definitions we’ve adapted from this APTA resource and this WebPT oneto bring you back up to speed: 1. Treatment:Includes all therapeutic services. 2. Time-based (constant attendance) CPT codes:These codes allow for variable billing in 15-minute increments when a practitioner provides a patient with one-on-one s…
What Are The Forms?
- Today, most payers—and providers—prefer electronic claim forms. However, some payers—a dwindling few—do still accept paper ones. The most common form is the Universal Claim Form (CMS 1500), although some payers may request that you use their own. Once you provide your services, you’ll submit a bill to either your patientor a third-party payer. Occasionally, you may act…
What’s The Process?
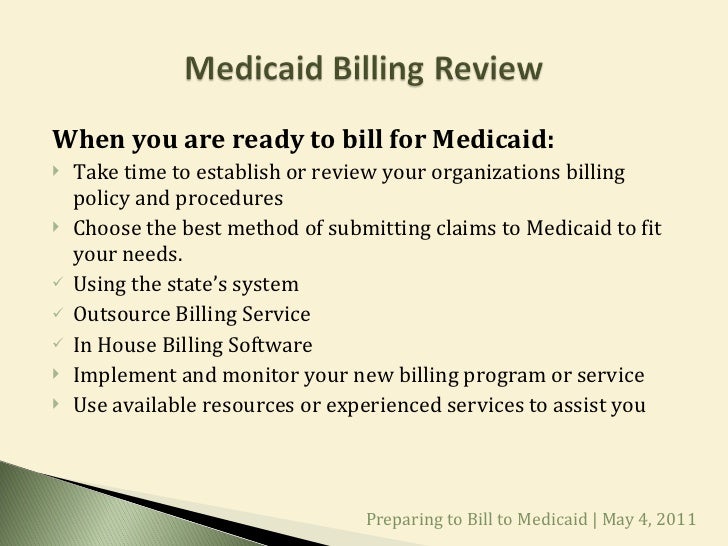
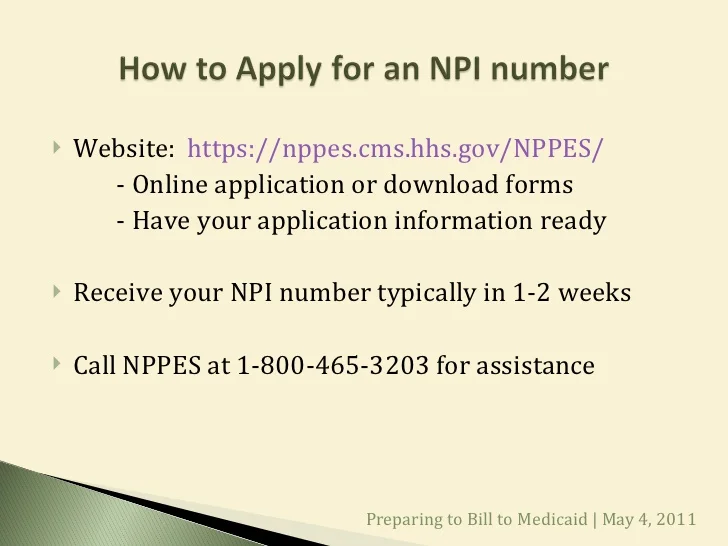
- Get credentialed.
If you haven’t already received credentialing, you may want to consider changing that. Being credentialed by an insurance company allows you to become an in-network provider, which may help you reach—and serve—a larger pool of potential patients. Some payers—like Medicare—do … - Negotiate payer contracts.
Just as rules are (sometimes) meant to be broken, contracts are (always) meant to be negotiated. This especially holds true when it comes to your private payer contracts. After all, these rates establish what you’re able to earn—and that number should be an accurate reflection of the valu…