However, safety net providers have limited resources and service capacity, and not all uninsured people have geographic access to a safety net provider. 28,29 The ACA has led to significant growth in the number of health centers and their service capacity through both new grant funds and new patient revenues due to expanded coverage. 30 However, this impact has been more limited in states not expanding Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Full Answer
How does the Affordable Care Act affect Medicare?
Sep 06, 2018 · Introduction. The primary components of the Affordable Care Act (ACA), including the individual mandate, subsidized Marketplace coverage, and state Medicaid expansions, were implemented in 2014. 1 A growing literature has emerged evaluating how state-specific insurance coverage, 2-10 access to care, 11-13 and self-assessed health 14-19 changed following the …
What happens to my ACA plan if I switch to Medicare?
May 08, 2017 · Getting coverage through the ACA is also associated with very substantial increases in the probability of having a usual place of care—by 47.1 percent according to the NHIS data and 86.5 percent in the BRFSS data. 9 These figures imply that people who gained coverage through the ACA’s expansions were just as likely to have a usual source of care as were those …
What is the impact of ACA on health care?
Oct 02, 2014 · Among other benefits, the Affordable Care Act (ACA) helps individuals on Medicare to save money with preventative care and brand-name drugs. Starting in January 2014, Medicare began covering many preventative services. with no out-of-pocket expense.. This coverage includes an annual wellness visit and screening tests as recommended, such as those for …
How did the Affordable Care Act (ACA) affect uninsurance disparities?
May 11, 2022 · Under the current regulations, an employer must offer employees self-only coverage that is affordable as defined by the ACA. For the 2022 tax year, affordability is set at 9.61%. There is no requirement for employers to also ensure coverage is affordable for dependents or spouses of the employee. The proposed rule would expand affordability to ...
Does the Affordable Care Act affect private insurance?
Can I stay on Obamacare instead of Medicare?
Does the Affordable Care Act apply to all insurance?
How will Affordable Care Act affect the uninsured?
Is Medicare more expensive than Obamacare?
Can I have both Medicare and Obamacare?
Which 3 populations do not have health care coverage even after the implementation of the Affordable Care Act ACA )?
What does the ACA cover?
When did the Affordable Care Act go into effect?
| Effective | March 23, 2010 Most major provisions phased in by January 2014; remaining provisions phased in by 2020; penalty enforcing individual mandate eliminated starting 2019 |
| Citations | |
|---|---|
| Public law | 111–148 |
| Statutes at Large | 124 Stat. 119 through 124 Stat. 1025 (906 pages) |
| Codification | |
What is the current impact of the ACA on health care in the US?
How does the ACA reduce healthcare costs?
How does the Affordable Care Act improved access to healthcare?
How does the ACA affect health care?
The Patient Protection and Affordable Care Act (ACA) expands access to health insurance in the United States , and, to date, an estimated 20 million previously uninsured individuals have gained coverage. Understanding the law’s impact on coverage, access, utilization, and health outcomes, especially among low-income populations, is critical to informing ongoing debates about its effectiveness and implementation. Early findings indicate that there have been significant reductions in the rate of uninsurance among the poor and among those who live in Medicaid expansion states. In addition, the law has been associated with increased health care access, affordability, and use of preventive and outpatient services among low-income populations, though impacts on inpatient utilization and health outcomes have been less conclusive. Although these early findings are generally consistent with past coverage expansions, continued monitoring of these domains is essential to understand the long-term impact of the law for underserved populations.
What are the effects of pre-ACA coverage?
Pre-ACA insurance expansions have largely demonstrated improved access to care for low-income populations. For example, the Massachusetts health reform was associated with significant reductions in forgone or delayed care and improvements in access to a personal doctor and usual source of care among adults overall (46, 54, 56, 58, 72, 88) and, in particular, for subgroups targeted by the ACA, such as low-income and childless adults (54, 56, 58). With regard to affordability, the Medicaid expansion in Oregon diminished financial hardship from medical costs, markedly reducing catastrophic OOP expenditures (5, 35, 98). In addition, other states that expanded public insurance prior to the ACA demonstrated improvements in access and affordability among low-income adults (62, 82) and children (33, 44) across comparable measures. More recently, the California LIHP waiver project found large reductions in the likelihood of any family OOP health care spending but did not detect significant differences in access to care, which may be explained by a well-established safety net in the state prior to program implementation (38). One ongoing concern about expanding coverage is that increased demand for services by newly insured individuals may limit access to care, but evidence from prior expansions does not appear to sufficiently support this hypothesis (67).
How does the reliance on the ACA affect health insurance?
Despite the availability of subsidies and cost-sharing reductions, the reliance of the ACA on health insurance exchanges may both increase access to health insurance and simultaneously pose unintended barriers to access, particularly for low-income populations. These barriers can arise in two ways. The most publicized method is through the creation of narrow networks, where insurers offer plans and policies with fewer doctors and hospitals in an effort to keep premiums as competitive as possible. Whether narrow networks create actual, rather than perceived, barriers to care has not been well established yet through research. Nevertheless, the existence of narrow networks has created the perception that exchange-based QHPs are limiting access to a greater extent than did pre-ACA policies, despite the absence of adequate baseline data from pre-ACA years.
What is the coverage gap?
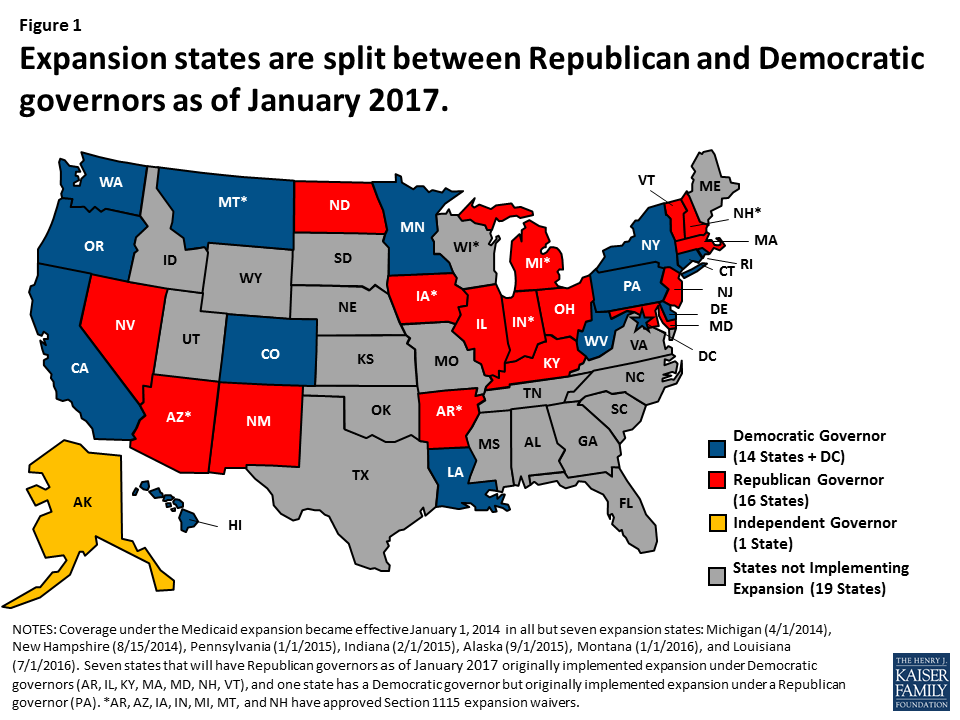
Approximately 9% of the remaining uninsured (almost 3 million Americans) fall into what is known as the “coverage gap.” This group represents poor, uninsured adults who reside in the 19 non–Medicaid expansion states whose income is above the state’s threshold for Medicaid eligibility but less than the 100% threshold for Marketplace subsidy eligibility. Also included are childless adults who were not previously eligible for Medicaid. Almost 90% of all adults in the coverage gap live in the South, half in either Texas or Florida, which aligns with this region’s high uninsurance rates, limited Medicaid eligibility, and low uptake of Medicaid expansion (37). Consistent with demographic characteristics and policies excluding nondisabled adults in states that did not expand Medicaid, African Americans and childless adults also account for a disproportionate share of individuals in the coverage gap (37). If all current nonexpansion states opted to expand Medicaid, 5.2 million currently uninsured adults would gain coverage: 2.9 million who are in the coverage gap, 0.5 million who are already eligible for Medicaid though alternate pathways, and an additional 1.8 million who are presently eligible for Marketplace subsidies with incomes from 100% FPL to 138% FPL yet did not enroll (37). Because a substantial portion of the remaining uninsured are either eligible for coverage or fall in the coverage gap, the law’s potential impact on the poor has not yet been fully realized.
How effective is Medicaid expansion?
The expansion of Medicaid has been particularly effective in states that took advantage of the opportunity for early Medicaid expansion allowed under the ACA. Between 2010 and 2014, six states (California, Colorado, Connecticut, Minnesota, New Jersey, Washington) and the District of Columbia extended Medicaid eligibility for low-income adults through the early Medicaid expansion option or the Section 1115 waiver process (18). In California, the LIHP significantly increased coverage by 7.3 percentage points for poor adults (up to 138% FPL) within the first two years (38). Similarly, one year after early expansion, Medicaid coverage increased significantly in Connecticut (4.9 percentage points) and modestly in Washington, DC (3.7 percentage points) among low-income childless adults—a key subpopulation targeted by Medicaid expansion (86). Trends in coverage gains in these early expansions echoed those of the Massachusetts health reform, which was associated with an estimated 18.4-percentage-point increase in coverage among low-income adults and even larger gains among low-income childless adults (54). Though these expansions were implemented prior to the ACA, their positive findings inform potential coverage gains for the poor under the ACA.
What is the goal of increased coverage eligibility and affordability?
An important goal of increased coverage eligibility and affordability is to increase access to adequate health care services for the poor. As a result, the ACA’s impact on access to high-quality health care has been evaluated across multiple dimensions, including access to a doctor, having a usual source of care, timeliness of care, affordability, and access to medications and preventive, primary, and specialty care.
Does the ACA expand Medicaid?
In summary, early evidence following ACA implementation has demonstrated significant progress toward its goal of expanding coverage for millions of low-income individuals who would have otherwise remained uninsured. Not all individuals equally experience the potential benefits of the law, however, and disparities have developed on the basis of state decisions regarding whether to expand Medicaid.
How does ACA affect health care?
On an individual basis, gaining insurance coverage through the ACA decreases the probability that a person will report not receiving medical care because of costs by 20.9 percent (Exhibit 3), according to the NHIS data. In the BRFSS data, insurance coverage is associated with a 25 percent decrease in the probability of not receiving medical care because of cost. To put this figure in context, prior to implementation of the insurance expansions, about 47 percent of uninsured people reported that they were unable to access care because of cost. Gaining coverage cut that figure by half. Getting coverage through the ACA is also associated with very substantial increases in the probability of having a usual place of care—by 47.1 percent according to the NHIS data and 86.5 percent in the BRFSS data. 9 These figures imply that people who gained coverage through the ACA’s expansions were just as likely to have a usual source of care as were those who had held insurance prior to the coverage expansions.
Why was the ACA not needed?
When the ACA was first introduced and debated, some opponents of the law argued that it was not needed because uninsured people already had adequate access to care. 10 Since its passage, others have argued that the insurance coverage provided to people under the ACA provides insufficient protection against high costs or offers such limited networks that the newly insured cannot find care. 11,12 These arguments imply that the ACA would not generate improvements in access to care.
How has the ACA improved access to care?
A few studies have examined how access to care at the population level has improved since ACA implementation. 3,4 One study, using the Gallup-Healthways Well-Being Index, found that by the end of the second enrollment period in 2015, the proportion of Americans without a personal doctor decreased by 3.5 percentage points and the proportion reporting an inability to afford care decreased by 5.5 percentage points. 5 These improvements were more pronounced in states that expanded Medicaid. Another study, using data from the Health Reform Monitoring Survey (HRMS), examined how various measures of access and affordability changed between the first and second open enrollment periods. 6 Among all income groups, there were significant improvements, including increases in the proportion reporting a regular source of care and in those reporting decreases in unmet needs because of cost of care. A recent Commonwealth Fund survey found that 72 percent of those enrolled in a marketplace plan or in Medicaid had used their insurance to visit a doctor, hospital, or other health care provider. More than half said they would not have been able to access or afford care before getting coverage through the ACA. 7 There is also evidence to suggest that the ACA has significantly reduced health disparities between racial and ethnic groups. 8
What is the goal of the Affordable Care Act?
One of the main goals of health reform like the Affordable Care Act (ACA) is to expand insurance coverage and, ultimately, to increase access to care. Among its reforms, the ACA expanded Medicaid coverage in participating states to all nonelderly adults with incomes below 133 percent of the federal poverty level (FPL), about $16,000 for an individual or $33,500 for a family of four, and provided subsidized insurance through the health care marketplaces for small businesses and individuals without access to employment-based insurance. Since the ACA’s first open enrollment period in the fall of 2013, the number of uninsured Americans has fallen from 41 million to 27 million. 1
Why did people go without care before the ACA?
A substantial share of the nonelderly population—from 9 percent to 19 percent, depending on the question asked—went without care because of cost in the period before the ACA expansions were implemented. The percentage was somewhat higher among those in the income range that is eligible for marketplace subsidies and much higher among those with incomes in the Medicaid-eligible range (Exhibit 1). Many adults reported that they had no usual place of care.
Does health insurance have better access to services?
Many prior studies have examined the relationship between insurance coverage and access to care. Virtually all have found that people with health insurance, whether Medicaid or private coverage, have better access to services.
Who said the emergency room is the health care option for the uninsured?
10 A. Terkel and S. Stein, “ Mitt Romney, on 60 Minutes, Cites Emergency Room as Health Care Option for Uninsured ,” Huffington Post, Sept. 24, 2012.
What is the impact of the Affordable Care Act on Medicare?
Among other benefits, the Affordable Care Act (ACA) helps individuals on Medicare to save money with preventative care and brand-name drugs. Starting in January 2014, Medicare began covering many preventative services with no out-of-pocket expense. This coverage includes an annual wellness visit ...
When will Medicare Part D donut hole close?
Medicare recipients will see some changes in their out-of-pocket expenses as the Medicare Part D donut hole is incrementally lowered to finally “close” in the year 2020. At that time, Medicare recipients will pay 25 percent of the drug cost.
What is the Medicare donut hole?
This refers to a temporary limit on prescription drug coverage, where the policy holder needs to pay a higher percentage of his or her medications after reaching this limit.
What happens if you are not dual eligible?
If you do not qualify as “Dual Eligible,” you may be determined “ Partial Dual Eligible .” This would qualify you for some financial assistance programs in your state based on income.
Is Medicare considered a dual insurance?
If you are “Dual Eligible,” generally Medicare would be billed first or considered your primary insurance, and then Medicaid would be billed for the balance acting as a secondary insurance. Please contact your local Department of Human Resources to determine if you qualify.
How did the Affordable Care Act affect Medicare?
The Affordable Care Act also affected Medicare by adding coverage for a "Wellness Visit" and a “Welcome to Medicare” preventative visit. It also eliminated cost-sharing for almost all of the preventive services covered by Medicare.
What is the Affordable Care Act?
The Affordable Care Act provides ways for hospitals, doctors and other health care providers to coordinate their care for Medicare beneficiaries. As a result, health care quality is improved and unnecessary spending is reduced.
What are the initiatives under the Affordable Care Act?
Under these initiatives, your doctor may get additional resources that will help ensure that your treatment is consistent. The Affordable Care Act provides ways for hospitals, doctors and other health care providers to coordinate their care for Medicare beneficiaries. As a result, health care quality is improved and unnecessary spending is reduced.
How much does Medicare pay for generic drugs?
In 2016, people with Medicare paid 45% for brand-name drugs and 58% for generic drugs while in the coverage gap. These percentages have shrunk over the last few years. Starting in 2020, however, you’ll pay only 25% for covered brand-name and generic drugs during the coverage gap.
How long does Medicare cover preventive visits?
This is a one-time visit. During the visit, your health care provider will review your health, as well as provide education and counseling about preventive services and other care.
How long does it take to sign up for Medicare?
You will get an initial enrollment period to sign up for Medicare. In most cases, the initial enrollment period begins three months before your 65th birthday and ends three months afterward. For most people, it’s beneficial to sign up for Medicare during this time. This is because those who sign up for Medicare after the initial enrollment period ends, face some negative consequences. For example, you might be required to pay a Part B (medical insurance) late enrollment penalty for as long as you have Medicare. Also, you are only permitted to enroll in Medicare Part B (and Part A in some cases) during the Medicare general enrollment period that runs from January 1 to March 31 each year. However, coverage will not begin until July of that year. This could create a gap in your insurance coverage.
When will Medicare be extended?
Under the Affordable Care Act, the Medicare Trust fund will be extended to at least the year 2029. This is a 12-year extension that is primarily the result of a reduction in waste, fraud, and abuse, as well as Medicare costs.
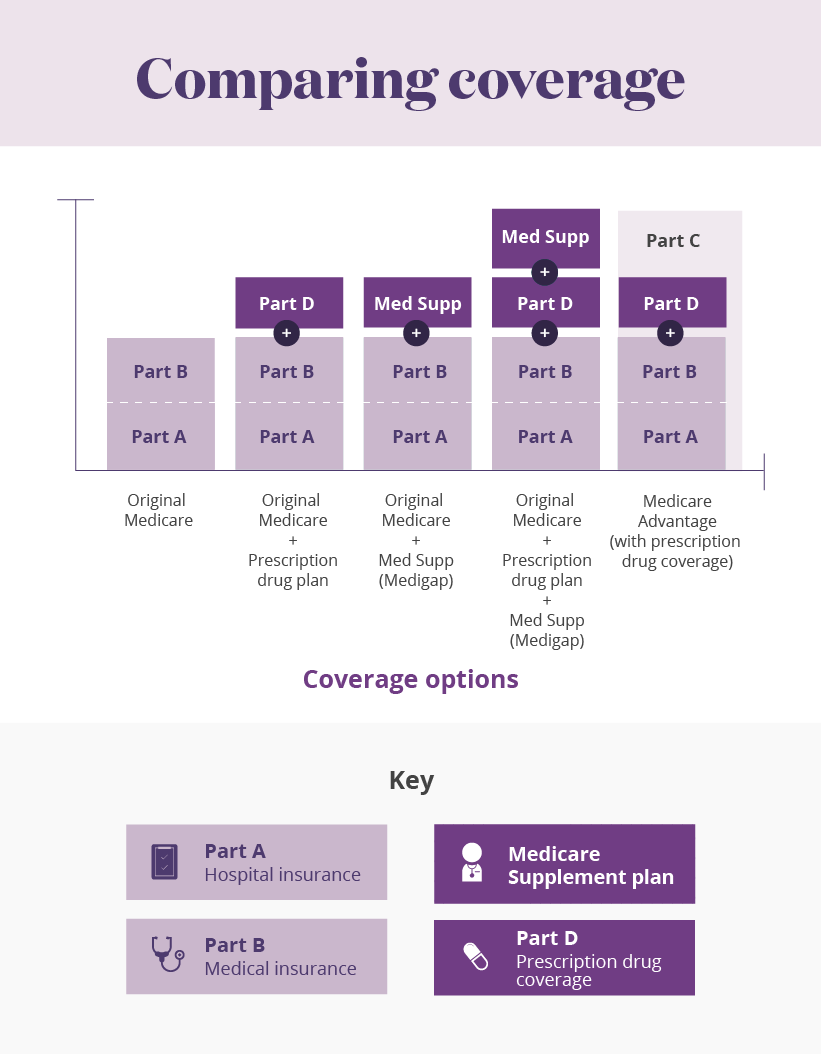
How did the ACA reduce Medicare costs?
Cost savings through Medicare Advantage. The ACA gradually reduced costs by restructuring payments to Medicare Advantage, based on the fact that the government was spending more money per enrollee for Medicare Advantage than for Original Medicare. But implementing the cuts has been a bit of an uphill battle.
Why did Medicare enrollment drop?
When the ACA was enacted, there were expectations that Medicare Advantage enrollment would drop because the payment cuts would trigger benefit reductions and premium increases that would drive enrollees away from Medicare Advantage plans.
What is Medicare D subsidy?
When Medicare D was created, it included a provision to provide a subsidy to employers who continued to offer prescription drug coverage to their retirees, as long as the drug covered was at least as good as Medicare D. The subsidy amounts to 28 percent of what the employer spends on retiree drug costs.
How much will Medicare Part B cost in 2021?
In 2021, most Medicare Part B enrollees pay $148.50/month in premiums. But beneficiaries with higher incomes pay additional amounts – up to $504.90 for those with the highest incomes (individuals with income above $500,000, and couples above $750,000). Medicare D premiums are also higher for enrollees with higher incomes.
What percentage of Medicare donut holes are paid?
The issue was addressed immediately by the ACA, which began phasing in coverage adjustments to ensure that enrollees will pay only 25 percent of “donut hole” expenses by 2020, compared to 100 percent in 2010 and before.
How many people will be on Medicare in 2021?
However, those concerns have turned out to be unfounded. In 2021, there were 26 million Medicare Advantage enrollees, and enrollment in Advantage plans had been steadily growing since 2004.; Medicare Advantage now accounts for 42% of all Medicare beneficiaries. That’s up from 24% in 2010, which is the year the ACA was enacted (overall Medicare enrollment has been growing sharply as the Baby Boomer population ages into Medicare, but Medicare Advantage enrollment is growing at an even faster pace).
What is the medical loss ratio for Medicare Advantage?
This is the same medical loss ratio that was imposed on the private large group health insurance market starting in 2011, and most Medicare Advantage plans were already conforming to this requirement; in 2011, the average medical loss ratio for Medicare Advantage plans was 86.3%. The medical loss ratio rules remain in effect, but starting in 2019, the federal government has reduced the reporting burden for Medicare Advantage insurers.
What happens if you miss your window to switch to Medicare?
If you miss your window to switch to Medicare, the federal government will catch up to you soon enough. When it finds that you should have moved to Medicare at age 65, it will assess you a fine to make you pay back any subsidy dollars that you have received toward your ACA coverage since you turn 65.
What happens if you don't enroll in Medicare at 65?
Even worse, if you fail to enroll in Medicare at age 65 because you choose to keep your Obamacare plan instead, you will later owe a Part B late enrollment penalty that will stay with you for as long as you remain enrolled in Medicare. It’s a 10% penalty per year for every year that you could have been enrolled in Medicare (at 65).
How long do you have to wait to cancel ACA?
Don’t be tempted to gamble with your health by cancelling your ACA plan early. If you have more than a 63-day window between when your ACA plan ends and your Medicare begins, then when you enroll in a Medigap plan, they can impose a waiting period for pre-existing conditions.
How much is the penalty for Medicare if you wait two years?
It’s a 10% penalty per year for every year that you could have been enrolled in Medicare (at 65). So if you waited two years, your would pay a 20% higher monthly premium for Part B for the rest of your life. This can be disappointing news if you’ve been getting your ACA plan very inexpensively due to a subsidy.
What is Medicare Supplement Plan G?
Coverage from Medicare and a Medicare Supplement Plan G would give you comprehensive benefits where you will pay nothing but the Part B deductible for Medicare-approved services and your monthly premiums.
Does ACA cover Medicare?
Your ACA coverage was never meant to replace Medicare. If you do not sign up for Medicare during your Initial Enrollment Period, you will be subject to substantial penalties when you later enroll in Medicare.
Can you cancel ACA coverage once you join Medicare?
So if you are enrolled in either an ACA plan or a short term medical plan, you’ll likely want to cancel that coverage once you join Medicare. Many people use short-term health insurance plans to bridge the gap between when their employer coverage ends and when they turn 65 and become eligible for Medicare.
Why do people fall into the Medicaid coverage gap?
At a time when many need health care services due to the health care crisis or face loss of financial security due to the economic downturn, millions fall into the Medicaid coverage gap due to their state’s decision not to expand eligibility.
What is the ACA expansion?
The ACA Medicaid expansion was designed to address historically high uninsured rates among low-income adults, providing a coverage option for people with limited access to employer coverage and limited income to purchase coverage on their own. In states that expanded Medicaid, millions of people gained coverage, ...
What percentage of people in the Medicaid coverage gap are adults without dependent children?
Reflecting limits on Medicaid eligibility outside ACA pathways, most people in the coverage gap (77%) are adults without dependent children. 4. Adults left in the coverage gap are spread across the states not expanding their Medicaid programs but are concentrated in states with the largest uninsured populations.
What is the coverage gap?
Reflecting limits on Medicaid eligibility outside ACA pathways, most people in the coverage gap (77%) are adults without dependent children. 4
How many people would be eligible for Medicaid if they were not expanding?
If states that are currently not expanding their programs adopt the Medicaid expansion, all of the nearly 2.2 million adults in the coverage gap would gain Medicaid eligibility. In addition, 1.8 million uninsured adults with incomes between 100 and 138% of poverty 6 (most of whom are currently eligible for Marketplace coverage) ...
What is the gap in Medicaid coverage?
The Coverage Gap: Uninsured Poor Adults in States that Do Not Expand Medicaid. The economic downturn and change in Administration are likely to bring renewed attention to gaps in Medicaid coverage in states that have not expanded eligibility under the Affordable Care Act (ACA). In recent months, millions have gained health insurance coverage ...
Why are there no uninsured adults in Wisconsin?
There are no uninsured adults in the coverage gap in Wisconsin because the state is providing Medicaid eligibility to adults up to the poverty level under a Medicaid waiver. The geographic distribution of the population in the coverage gap reflects both population distribution and regional variation in state take-up of the ACA Medicaid expansion.
How does lack of health insurance affect access to care?
Lack of health coverage, even for short periods of time, results in decreased access to care. Research has shown that adults who experience gaps in their health insurance coverage are less likely to have a regular source of care or to be up to date with blood pressure or cholesterol checks than those with continuous coverage. 20 Research also indicates that children who are uninsured for part of the year have more access problems than those with full-year coverage. 21,22 Similarly, adults who lack insurance for an entire year have poorer access to care than those who have coverage for at least part of the year, suggesting that even a short period of coverage can improve access to care. 23
What happens if you don't have health insurance?
Compared to those who have health coverage, people without health insurance are more likely to skip preventive services and report that they do not have a regular source of health care .
Why are uninsured people more likely to have negative health consequences?
Because uninsured people are less likely than those with insurance to have regular outpatient care, they are more likely to have negative health consequences. Because uninsured patients are also less likely to receive necessary follow-up screenings than their insured counterparts, 8 they have an increased risk of being diagnosed at later stages ...
Does health insurance make a difference?
Health insurance makes a difference in whether and when people get necessary medical care, where they get their care, and ultimately, how healthy they are . Uninsured people are far more likely than those with insurance to postpone health care or forgo it altogether. The consequences can be severe, particularly when preventable conditions or chronic diseases go undetected.