LCSWs do not need to opt-in or opt-out of Medicare. If an LCSW wishes to be paid through Medicare, the LCSW must opt-in as a Medicare provider. All LCSWs are expected to accept assignment of any Medicare beneficiary who needs mental health treatment unless there is a reason that the beneficiary needs to be referred.
Full Answer
Do LCSWs get paid through Medicare?
If an LCSW wishes to be paid through Medicare, the LCSW must opt-in as a Medicare provider. All LCSWs are expected to accept assignment of any Medicare beneficiary who needs mental health treatment unless there is a reason that the beneficiary needs to be referred.
How do I Opt Out of Medicare as an LCSW?
CSWA has templates for private contracts with Medicare enrollees and to opt-out of Medicare in the Members Only section of the CSWA website ( www.clinicalsocialworkassociation.org) . If an LCSW decides to opt-in, the LCSW accepts “assignment” of all Medicare cases who seek treatment.
Can I assign Medicare beneficiaries to an LCSW?
All LCSWs are expected to accept assignment of any Medicare beneficiary who needs mental health treatment unless there is a reason that the beneficiary needs to be referred.
What is an LCSW and where do they work?
An LCSW may work in an office, or they might perform services out in the community. In addition to solo or group private practice, LCSWs may be employed in local government agencies, community and social services, schools, recovery programs, rehabilitation services, non-profits, jails, hospitals and other health care settings. 1
What does it mean to be paneled with insurance companies?
An insurance panel is a collection of healthcare providers to whom an insurance company will pay for services for their customers. It's also called credentialing, and each insurance provider selects its own panel. So, for each insurance company you're looking to work with, you'll need to submit another application.
How Much Does Medicare pay for 90837?
$132.69What is the difference between the “facility rate” and “nonfacility rate” for telehealth services?CodeService2021 Facility Rate90832Psychotherapy 30-minutes$68.7490837Psychotherapy 60-minutes$132.6996132Neuropsych Test Eval$106.0896158Hlth Bhvr Intrv Indvl$58.971 more row•Dec 10, 2021
How do I bill to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
How do I add a provider to a group in Pecos?
1:566:13Medicare Provider Enrollment Through PECOS - YouTubeYouTubeStart of suggested clipEnd of suggested clipAfter logging in click my enrollments. Next click new application to start the application processMoreAfter logging in click my enrollments. Next click new application to start the application process Pecos asks a series of questions to identify the enrollment.
Can social workers bill for Medicare?
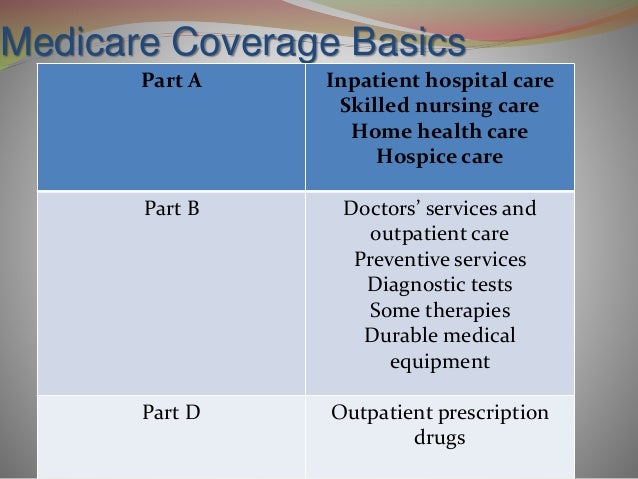
Clinical social workers (CSWs) are the largest group of mental health service providers in the United States and are among the professions that can bill Medicare Part B for mental health services.
Can a Lcsw bill 90837?
CPT code 90837 doesn't have to be billed by a licensed medical doctor. It's mainly used by licensed mental health professionals. Typically, Licensed Clinical Social Workers, Licensed Professional Clinical Counselors, Licensed Marriage and Family Therapists, and Clinical Psychologists will bill CPT code 90837.
Which is a combination Medicare and Medicaid option that combines medical social?
What are dual health plans? Dual health plans are designed just for people who have both Medicaid and Medicare. They're a special type of Medicare Part C (Medicare Advantage) plan. Dual health plans combine hospital, medical and prescription drug coverage.
How long does it take to get a Medicare provider number?
Most Medicare provider number applications are taking up to 12 calendar days to process from the date we get your application. Some applications may take longer if they need to be assessed by the Department of Health.
Can I submit a claim directly to Medicare?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
What is Pecos Medicare requirement?
It is a database where physicians register with the Centers for Medicare and Medicare Services (CMS). CMS developed PECOS as a result of the Patient Protection and Affordable Care Act. The regulation requires all physicians who order or refer home healthcare services or supplies to be enrolled in Medicare.
How do I add a new provider to Medicare?
Enrollment ApplicationsEnroll as a Medicare provider or supplier.Review information currently on file.Upload your supporting documents.Electronically sign and submit your information online.
Is Pecos ID same as Medicare number?
The following walk-thru explains how a user can find their Medicare ID number in PECOS. Medicare numbers are also known as the CCN, P-Tan, Oscar, Provider number, or Medicare ID.
How to get a panel?
Getting paneled requires a lot of information and documentation, which may include your: 1 Licensure information 2 Practice address 3 NPI number 4 Resume 5 Proof of malpractice insurance 6 Taxonomy code (if you plan to bill Medicare/Medicaid) 7 Proof of liability insurance from your landlord (if you rent) 8 Advanced training or credentialing paperwork (if you have any)
What to do when an insurance company says they are full?
The best thing you can do when an insurance company tells you they’re full or not accepting applications from people with your specialty is build a relationship with the provider until they have openings for your preferred services. This means calling them to reiterate your differentiating skills.
What happens if you apply for unemployment insurance and it expires?
After applying, you’ll need to follow up regularly. If your application gets stuck in limbo with no action for too long, it may expire and you’ll have to start all over. To avoid any issues, make sure to call the insurance company every time you submit documentation to make sure they received it.
What do you need to get paneled?
Getting paneled requires a lot of information and documentation, which may include your: Taxonomy code ( if you plan to bill Medicare/Medicaid) Proof of liability insurance from your landlord (if you rent) Advanced training or credentialing paperwork (if you have any)
How many times do you have to re-attest to a claim?
After applying, make sure you don’t lose any of your application information, since you’ll be asked to “re-attest” to it 2–4 times per year. Make sure to respond to such requests quickly. Insurance companies will know if you don’t and may refuse to pay claims.
Can therapy notes be submitted electronically?
Once you've done this, TherapyNotes™ can help you submit your insurance claims electronically. This will save you time and paper, speed up payments, and reduce the likelihood of errors on claims. You can even submit claims electronically if you're not in-network.
What services are covered by Medicare?
Services you perform as a clinical social worker are eligible for coverage under Part B of Medicare if they are services that would be covered if performed by a physician or if the services are incident to the services of a physician, nurse practitioner or other medical practitioner.
Why do you need to document your Medicare claim?
Documentation is also used to ensure that care is provided by a qualified social worker and to monitor the patient's progress. If you fail to provide complete documentation, Medicare claims may be denied. Document each appointment with your patients, as well as any phone calls, referrals and consultations.
Do social workers have to be on Medicare?
Medicare Billing Requirements for Social Workers. Not all social workers are approved to provide services under Medicare. Direct-service social workers help people cope with problems in their everyday lives.
Does Medicare cover social work?
Medicare Part B does not cover social work services to inpatients at hospitals or skilled nursing facilities. In addition, if state law prohibits a social worker from providing a certain treatment or service, Medicare will not cover this service, even if it is normally covered for other social workers. Get the Best Mortgage Rate for You | ...
What is the Medicare reimbursement rate for CSWs?
The Improving Access to Mental Health Act also increases the Medicare reimbursement rate for CSWs from 75% to 85% of the physician fee schedule, thereby mitigating reimbursement inequity.
How does the Mental Health Act affect Medicare?
The legislation enhances Medicare beneficiaries’ access to the valuable services of independent CSWs in two scenarios: The Improving Access to Mental Health Act also increases the Medicare reimbursement rate for CSWs from 75% to 85% of the physician fee schedule, thereby mitigating reimbursement inequity .
Can Medicare beneficiaries receive mental health services?
However, beneficiaries who receive SNF services under Medicare Part A cannot simultaneously receive services from an independent CSW under Part B. This limits the pool of practitioners who can serve SNF residents, which is problematic given the high incidence of mental health conditions among SNF residents, and the high ratio of 120 residents to every medical social worker (who may not actually have received a social work degree). This access barrier exists because when SNF consolidated billing was implemented, psychiatrists’ and psychologists’ services were excluded from the Prospective Payment System, but CSW services were not. Medicare beneficiaries who transfer from a setting in which they receive mental health services from an independent CSW under Medicare Part B to a SNF, where they cannot receive such services, experience a disruption in care. Such care transitions can occur even if the beneficiary is moved within the same building or remains in the same bed. The reimbursement restriction also limits the pool of Medicare providers available to meet newly identified mental health needs of beneficiaries during a SNF stay. Correcting this will enhance beneficiaries’ access to mental health services in SNFs.
Can you get Medicare Part B reimbursement for a psychiatrist?
Although beneficiaries can access Medicare Part B–reimbursed HBAI services from psychologists and psychiatrists, they cannot access them from independent CSWs. This access barrier exists because Medicare Part B reimbursement for independent CSW services is restricted to the diagnosis and treatment of mental illness.
How much does Medicare cost for LCSW?
Though Medicare rates for LCSWs vary by region, they generally fall between $60-80 for 90806 provided by an LCSW.
How long does Medicare opt out last?
The opt-out period is generally for two years. Opt-outs may be renewed for subsequent two-year periods. The provider must opt out of Medicare for ALL beneficiaries and services with the exception of emergency or urgent care situations.
Does LCSW accept Medicare?
An LCSW is unwilling to accept Medicare reimbursement rates. An LCSW is concerned about the 40% co-pay currently in place for Medicare enrollees to access mental health services and the hardship this represents for those on limited incomes [which will gradually reach the 20% co-pay for medical benefits by 2014].
Can LCSWs reapply for Medicare?
LCSWs can reapply after being dropped from the Medicare provider list to become a provider again, if they so choose ( Medicare Reimbursement for LCSWs: Past, Present, and Future, access, 10/06). LCSWs are used to thinking about how to get onto insurance panels, not about how to stay off them.
Do LCSWs have to opt out of Medicare?
While it is true that the application process is lengthy and complicated, and the opt-out process also takes some work, the Social Security Law as of 1990 states that all LCSWs must “opt-out” of Medicare if they choose not to “opt-in”, i.e., become an official Medicare provider.
How to become a Medicare provider?
Become a Medicare Provider or Supplier 1 You’re a DMEPOS supplier. DMEPOS suppliers should follow the instructions on the Enroll as a DMEPOS Supplier page. 2 You’re an institutional provider. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should use the Medicare Enrollment Guide for Institutional Providers.
How to get an NPI?
If you already have an NPI, skip this step and proceed to Step 2. NPIs are issued through the National Plan & Provider Enumeration System (NPPES). You can apply for an NPI on the NPPES website.
How long does it take to change your Medicare billing?
To avoid having your Medicare billing privileges revoked, be sure to report the following changes within 30 days: a change in ownership. an adverse legal action. a change in practice location. You must report all other changes within 90 days. If you applied online, you can keep your information up to date in PECOS.
Can you bill Medicare for your services?
You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify. You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.
Do you need to be accredited to participate in CMS surveys?
ii If your institution has obtained accreditation from a CMS-approved accreditation organization, you will not need to participate in State Survey Agency surveys. You must inform the State Survey Agency that your institution is accredited. Accreditation is voluntary; CMS doesn’t require it for Medicare enrollment.
What is a licensed clinical social worker?
Licensed Clinical Social Workers specialize in providing mental health services in private practices, clinics, hospitals, agencies, and other settings. The primary function of clinical social workers is to provide mental health treatment, to include assessment, diagnosis, treatment, and prevention.
What is LCSW in psychology?
Where. An LCSW is a Licensed Clinical Social Worker. LCSWs are Master’s level Social Workers with extensive professional training and expertise in mental health. LCSWs are required to fulfill requirements in their State of practice to obtain licensure, and must also successfully pass a national examination.
How does the cost of therapy vary?
The cost of therapy can vary widely depending on geographical location, type of provider, and what type of psychotherapy or service is being performed. The cost of a provider can increase with their level of experience, amount of time in practice, or professional reputation, as well as demand for their services.
What is a LPC in counseling?
License d Practical Counselors (LPC) and Marriage and Family Therapists (MFT) are two other types of mental health professionals trained to perform counseling and psychotherapy. With multiple options available to consumers, it is important to research the qualifications and specializations of a provider.
What is direct practice social work?
Some types of social workers work directly with individuals, families, and groups performing services other than psychotherapy. These are called direct practice social workers. Direct practice refers to face-to-face work with clients.
How much does a psychotherapist cost?
A typical psychotherapy session with an LCSW can cost $80-$150 per hour. If insurance benefits are used, there may be a co-pay that a client is required to pay per session.
What is NPI in Medicare?
The National Provider Identifier (NPI) will replace health care provider identifiers in use today in standard health care transactions. Suppliers must obtain their NPI prior to enrolling in the Medicare program. Enrolling in Medicare authorizes you to bill and be paid for services furnished to Medicare beneficiaries.
What is Medicare application?
application is used to initiate a reassignment of a right to bill the Medicare program and receive Medicare payments (Note: only individual physicians and non-physician practitioners can reassign the right to bill the Medicare program).