How long does it take Medicare claims to process?
approximately 30 daysMedicare takes approximately 30 days to process each claim. Medicare pays Part A claims (inpatient hospital care, inpatient skilled nursing facility care, skilled home health care and hospice care) directly to the facility or agency that provides the care.
How does billing work with Medicare?
After a health care provider treats a Medicare patient, the provider sends a bill to Medicare that itemizes the services received by the beneficiary. Medicare then sends payment to the provider equal to the Medicare-approved amount for each of those services.Mar 31, 2021
What document notifies Medicare beneficiaries of claims processing?
The MSN is used to notify Medicare beneficiaries of action taken on their processed claims. The MSN provides the beneficiary with a record of services received and the status of any deductibles.
What is the most common method of claim transmission?
Paper claims (manual) are the most common types of claims submission. The HIPAA regulations require electronic transmission claims. The electronic transmission claim number is 12 837.Nov 24, 2021
Who processes traditional Medicare claims?
Medicare Administrative Contractor (MAC)When a claim is sent to Medicare, it's processed by a Medicare Administrative Contractor (MAC). The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim. This process usually takes around 30 days.
Why is Medicare not paying on claims?
If the claim is denied because the medical service/procedure was “not medically necessary,” there were “too many or too frequent” services or treatments, or due to a local coverage determination, the beneficiary/caregiver may want to file an appeal of the denial decision. Appeal the denial of payment.
What happens after Medicare processes a claim?
After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). A request for payment that you submit to Medicare or other health insurance when you get items and services that you think are covered. s for covered services and supplies you get.
Can a patient bill Medicare directly?
If you're on Medicare, your doctors will usually bill Medicare for any care you obtain. Medicare will then pay its rate directly to your doctor. Your doctor will only charge you for any copay, deductible, or coinsurance you owe.Sep 27, 2021
Can a doctor charge more than Medicare allows?
A doctor is allowed to charge up to 15% more than the allowed Medicare rate and STILL remain "in-network" with Medicare. Some doctors accept the Medicare rate while others choose to charge up to the 15% additional amount.
What are the 5 steps to the medical claim process?
These steps include: Registration, establishment of financial responsibility for the visit, patient check-in and check-out, checking for coding and billing compliance, preparing and transmitting claims, monitoring payer adjudication, generating patient statements or bills, and assigning patient payments and arranging ...
What are the 3 most important aspects to a medical claim?
Three important aspects of medical billing are claims validation, the migration of crucial software from local servers to cloud computing service providers and staying current on codes.Claims Validation. ... Cloud Computing. ... Codes and Compliance.Jan 13, 2016
In what format are healthcare claims sent?
The 837P (Professional) is the standard format health care professionals and suppliers use to send health care claims electronically. The ANSI ASC X12N 837P (Professional) Version 5010A1 is the current electronic claim version.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
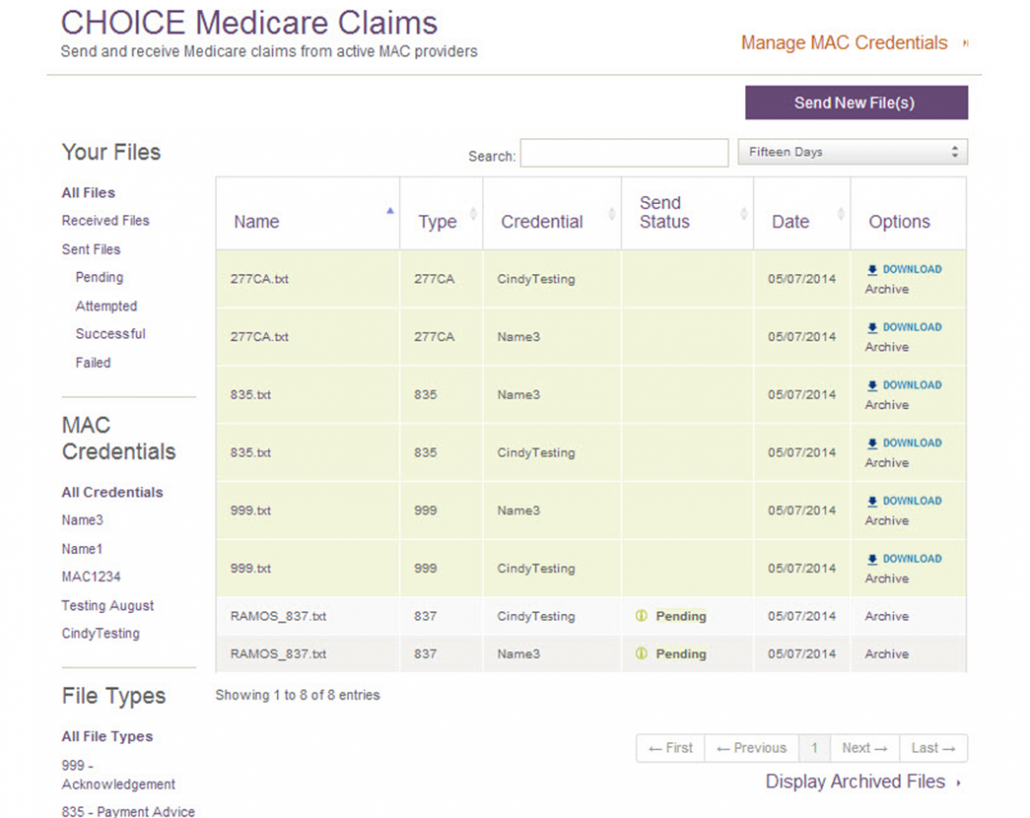
How does Medicare receive claims?
Your Medigap (supplemental insurance) company or retiree plan receives claims for your services 1 of 3 ways: Directly from Medicare through electronic claims processing. This is done online. Directly from your provider, if he/she accepts Medicare assignment. This is done online, by fax or through the mail.
How much does Medicare pay for Part B?
If the provider accepts assignment (agrees to accept Medicare’s approved amount as full reimbursement), Medicare pays the Part B claim directly to him/her for 80% of the approved amount. You are responsible for the remaining 20% (this is your coinsurance ). If the provider does not accept assignment, he/she is required to submit your claim ...
How to file a claim with Medicare?
Follow these steps: Fill out the claim form provided by your insurance company (if required). Attach copies of the bills you are submitting for payment (if required). Attach copies of the MSN related to those bills.
What happens if a provider does not accept assignment?
If the provider does not accept assignment, he/she is required to submit your claim to Medicare, which then pays the Part B claim directly to you. You are responsible for paying the provider the full Medicare-approved amount, plus an excess charge . Note: A provider who treats Medicare patients but does not accept assignment cannot charge more ...
Does Medicare send a bill for MSN?
For more information, see Assignment for Original Fee-for-Service Medicare . Medicare will send you a Medicare Summary Notice (MSN) form each quarter. Previously known as the Explanation of Medicare Benefits, the MSN is not a bill. You should not send money to Medicare after receiving an MSN.
Is MSN a bill?
How much Medicare approved and paid. How much you owe. Previously known as the Explanation of Medicare Benefits, the MSN is not a bill. You should not send money to Medicare after receiving an MSN. Your provider will bill you separately.
What is the purpose of MSN?
The MSN is used to notify Medicare beneficiaries of action taken on A/B MAC (A)/(HHH) processed claims. MSNs are not used by A/B MACs (HHH) for RAPs, and RAP data are not included on the monthly MSN. The MSN provides the beneficiary with a record of services received and the status of any deductibles.
How big is a window on an envelope?
For all sizes of the envelope, the window measures 4.5 inches in width and 1.5 inches in height with rounded corners. On standard #10 and half-size envelopes, the window is located at (0.75˝, 2.06˝) from left top corner.
How long does a SNF benefit last?
A benefit period begins the day you first receive inpatient hospital services or, in certain circumstances, SNF services, and ends when you haven’t received any inpatient care in a hospital or inpatient skilled care in a SNF for 60 days in a row. Inpatient Hospital: You have {. #} out of 90 covered benefit days.
Do MACs use MSN?
To ensure that all messages are uniform throughout the Medicare program, A/B MACs (A), (B), (HHH), and DME MACs may not use locally developed MSN messages until approved by the regional office (RO). The MSNs are not sent to providers. Providers receive remittance advice records.
What is MSN in Medicare?
The MSN is a notice that people with Original Medicare get in the mail every 3 months. It shows: All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period. What Medicare paid. The maximum amount you may owe the provider. Learn more about the MSN, and view a sample.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
How long does it take to see a Medicare claim?
Log into (or create) your secure Medicare account. You’ll usually be able to see a claim within 24 hours after Medicare processes it. A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare.
What is Medicare Part A?
Check the status of a claim. To check the status of. Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. or.
What is a PACE plan?
PACE plans can be offered by public or private companies and provide Part D and other benefits in addition to Part A and Part B benefits. claims: Contact your plan.
Does Medicare Advantage offer prescription drug coverage?
Medicare Advantage Plans may also offer prescription drug coverage that follows the same rules as Medicare drug plans. Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs.
Is Medicare paid for by Original Medicare?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. or other. Medicare Health Plan. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan.
How does accepting assignment affect Medicare?
First, it affects the rates that the provider will charge for a given diagnostic code since accepting assignment also means accepting Medicare's schedule of reimbursements ( or up to 15% higher if a provider chooses). The other big impact is on the claims side.
What does it mean when a provider accepts an assignment?
The term for this is that a provider accepts "assignment" which essentially means that the provider is in Medicare's network. This has two major impacts.
Does Medigap pay for things that Medicare does not?
This is a very important concept to understand. Many people think that Medigap plans will offer "additional" benefits to traditional Medicare, meaning, it will pay for things that Medicare will not pay for. We have to be careful here.
Does Medicare supplement work with Medigap?
First, it's important to understand how Medicare itself deals with providers and secondly, how Medigap supplements coordinate with Medicare itself. The first point depends on the status of the particular provider (doctor or hospital) in question. If the provider participates with Medicare, the claims process can be pretty smooth and coordinated.
Does Medicare pay you up front?
If you paid up front, Medicare typically would reimburse you accordingly. A non-assignment provider might request the excess amount up front (up to 15% higher than what Medicare allows). These providers may file a claim on your behalf to Medicare in these situations.
Does Medicare Supplement Plan pay for a procedure?
We have to be careful here. For a given medical procedure, if Medicare deems that it is not covered, the Medicare supplement plan will also not pay. The supplement looks to Medicare to determine what is eligible and then pays accordingly.
Does Medicare pay part of a covered benefit?
Medicare will pay part of a covered benefit and the supplement will pay all or part of the remaining claim. You will then get an Explanation of Benefits or an EOB showing what the total amount was, what Medicare and supplement paid, and your responsibility if any for that particular claim.