
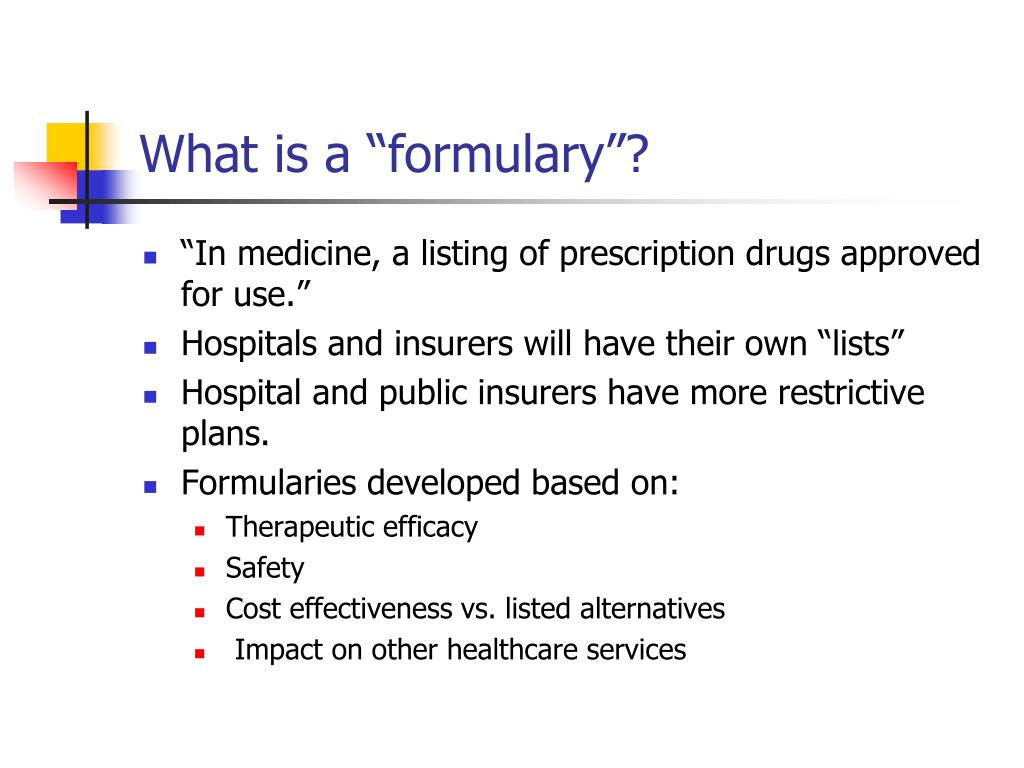
A drug formulary is a list of generic and brand-name prescription drugs covered by a health plan. The health plan generally creates this list by forming a pharmacy and therapeutics committee consisting of pharmacists and physicians from various medical specialties.
What are the rules of Medicare?
- You must have Medicare Part A and Part B.
- A Medigap policy is different from a Medicare Advantage Plan. ...
- You pay the private insurance company a monthly premium The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage. ...
- A Medigap policy only covers one person. ...
What is the Medicare Part D formulary?
- Tier 1: Preferred generic drugs
- Tier 2: Generic drugs
- Tier 3: Preferred brand drugs and select insulin drugs
- Tier 4: Non-preferred drugs
- Tier 5: Specialty drugs
What is formulary drug list?
A formulary drug or drug formulary is a list of prescription drugs that includes both generic and brand names. These are used by doctors or practitioners to identify drugs that have the greatest overall value. The formulary is maintained by an independent committee of practicing physicians and pharmacists.
What is a drug formulary and tier pricing?
This formulary outlines the most commonly prescribed medications covered under your plan’s prescription drug benefits. The formulary is also known as the Prescription Drug List (PDL). A formulary identifies the drugs available for certain conditions and organizes them into cost levels, also known as tiers.
How is a formulary defined in Medicare?
A Medicare formulary is a list of prescription drugs that are covered by a Medicare Part D plan. Coverage for a specific drug may vary from plan to plan. Each Medicare Part D plan has its own unique formulary, meaning that it has its own unique list of drugs the plan covers.
How is a formulary determined?
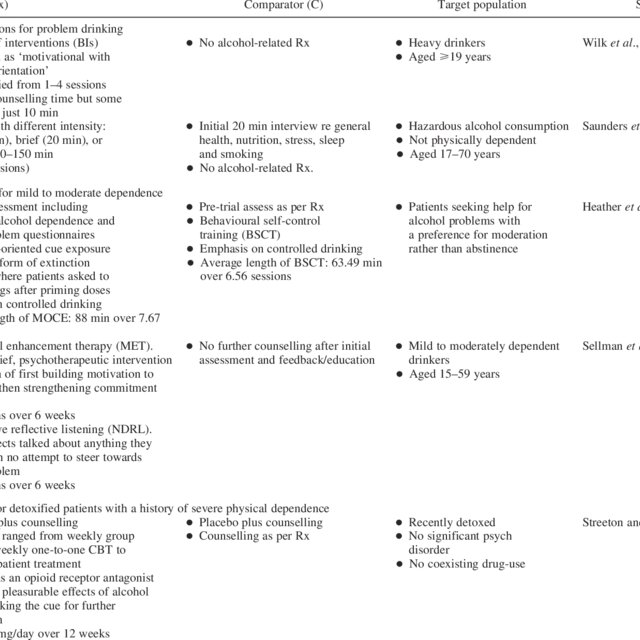
Formulary Development. The medications and related products listed on a formulary are determined by a pharmacy and therapeutics (P&T) committee or an equivalent entity. P&T committees are comprised of primary care and specialty physicians, pharmacists and other professionals in the health care field.
Are formularies based on CMS guidelines?
The MMA requires CMS to review Part D formularies to ensure that beneficiaries have access to a broad range of medically appropriate drugs to treat all disease states and to ensure that the formulary design does not discriminate or substantially discourage enrollment by certain groups.
How often are formularies updated?
There are also some instances where the same product can be made by two or more manufacturers, but greatly vary in cost. In these instances, only the lower cost product may be covered. How often is the Formulary updated? Formulary changes typically occur twice per year.
What are the three types of formulary systems?
An open formulary has no limitation to access to a medication. Open formularies are generally large. A closed formulary is a limited list of medications. A closed formulary may limit drugs to specific physicians, patient care areas, or disease states via formulary restrictions.
Does Medicare determine drug tiers?
Each plan can divide its tiers in different ways. Each tier costs a different amount. Generally, a drug in a lower tier will cost you less than a drug in a higher tier. A type of Medicare prescription drug coverage determination.
What is formulary classification?
A formulary is a list of drugs (both generic and brand name) that are selected by your health plan as the drugs they prefer to treat certain health conditions.
Are all Part D formularies the same?
Each Medicare Part D plan has its own unique formulary, meaning that it has its own unique list of drugs the plan covers. Medicare formularies are used to help provide Medicare beneficiaries with affordable and effective medications.
What if my drug is not on the formulary?
If a medication is “non-formulary,” it means it is not included on the insurance company's “formulary” or list of covered medications. A medication may not be on the formulary because an alternative is proven to be just as effective and safe but less costly.
Why do formularies change?
Formulary changes happen from time to time if drugs are: Recalled from the market; Replaced by a new generic drug; or, Clinical restrictions are added, including, but not limited to, prior authorization, quantity limits or step therapy.
What are the two types of formularies?
Other Types of Formularies. While “open” and “closed” formularies typically are used to denote the spectrum of evaluation, from a passive to active process, other permutations of formularies are known to exist.
What information is included in a formulary?
A list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list.
What drugs are included in Medicare formulary?
All Medicare formularies generally must include coverage for at least two different drugs within most drug categories, and they must include all available drugs for the following categories: HIV/AIDS treatments. Antidepressants.
What is a drug formulary?
A drug formulary is a list of medications covered by a Medicare drug plan. Here are 7 facts about Medicare drug formularies that every beneficiary should know. A Medicare formulary is the list of prescription drugs that are covered by a particular Medicare Part D or Medicare Advantage plan. Each plan includes its own formulary ...
What is tier 1 drug?
Drugs on a Medicare formulary are divided into tiers that determine the cost paid by beneficiaries. For example, a tier 1 drug might consist of low-cost, generic drugs and require only a small copayment in order to fill a prescription.
Does Medicare cover prescription drugs?
All Medicare plans with prescription drug coverage must make sure that members have access to all medically necessary drugs listed on their formulary.
Does Medicare cover all drugs?
All Medicare formularies generally must include coverage for at least two different drugs within most drug categories, and they must include all available drugs for the following categories:
Can Medicare have generic drugs?
The drug formulary of one Medicare plan may differ from another plan’s formulary. Medicare drug formularies can feature both generic and name brand drugs.
Can Medicare formulary change?
A Medicare formulary can change throughout the year. Drugs may be added or removed from the market at any time, and therefore drugs may be added or removed from a plan’s formulary. Drugs may also remain for sale on the market but be removed from a plan’s formulary for a variety of reasons.
What is a formulary?
A formulary is a list of generic and brand name drugs that are covered by a health plan. Pharmacy Benefit Dimensions (PBD) offers several formulary options for both our self-funded and Medicare Part D Prescription Drug Plan (PDP) Employer Group Waiver Plan (EGWP) clients.
What is a tier?
A formulary is divided into various categories, or tiers. Drugs are placed in tiers based on the drug type. Drug types include generic, preferred brand, non-preferred brand and specialty. At PBD, we offer a variety of formulary options based on a tiering structure including:
How does this benefit our clients?
Our clinical team utilizes a value-based approach when making formulary decisions which focuses on low-cost therapeutic alternatives such as generic medications, to help balance efficacy, safety and cost-effectiveness.
What do pharmacists do when filling prescriptions?
When you fill a prescription at the pharmacy, Medicare drug plans and pharmacists routinely check to make sure the prescription is correct, that there are no interactions, and that the medication is appropriate for you. They also conduct safety reviews to monitor the safe use of opioids and other frequently abused medications. These reviews are especially important if you have more than one doctor who prescribes these drugs. In some cases, the Medicare drug plan or pharmacist may need to first talk to your doctor before the prescription can be filled.
What to do if your prescription is not filled?
If your pharmacy can’t fill your prescription as written, the pharmacist will give you a notice explaining how you or your doctor can call or write to your plan to ask for a coverage decision. If your health requires it, you can ask the plan for a fast coverage decision. You may also ask your plan for an exception to its rules before you go to the pharmacy, so you’ll know if your plan will cover the medication. Visit Medicare.gov/medicare-prescription-drug-coverage-appeals to learn how to ask for an exception.
Does Medicare cover prescription drugs?
Medicare drug plans have contracts with pharmacies that are part of the plan’s “network.” If you go to a pharmacy that isn’t in your plan’s network, your plan might not cover your drugs. Along with retail pharmacies, your plan’s network might include preferred pharmacies, a mail-order program, or an option for retail pharmacies to supply a 2- or 3-month supply.
Does Medicare cover opioids?
Some Medicare drug plans will have a drug management program to help patients who are at risk for prescription drug abuse. If you get opioids from multiple doctors or pharmacies, your plan may talk with your doctors to make sure you need these medications and that you’re using them appropriately. If your Medicare drug plan decides your use of prescription opioids and benzodiazepines may not be safe, the plan will send you a letter in advance. This letter will tell you if the plan will limit coverage of these drugs for you, or if you’ll be required to get the prescriptions for these drugs only from a doctor or pharmacy that you select.
What Happens if a Drug is Not on the Formulary for a Medicare Part D Provider?
If your drug isn’t on the formulary, you’ll likely pay the full price. Of course, you can request a formulary exception or file an appeal.
How Can I Appeal a Drug on the Part D Formulary?
You can file an appeal when you disagree with the decision made by the insurance company. So, if the plan denies a drug claim but you believe it should have coverage, you can file an appeal. You may need supporting documents to show necessity, prior authorization, or step therapy requirements have been met.
Who Has the Best Part D Formulary?
Medicare Part D plans have a star-rating system similar to Medicare Advantage. Many locations don’t have 5-star plans, but some areas will have those options.
When Is A Formulary Exception Likely to Be Approved?
Exceptions are more likely to see approval when the requested medication is medically necessary for you. Your doctor must submit a statement to your plan supporting the exception request.
How to know what medications are in Medicare Part D?
How to Know What Medications are in a Medicare Part D Formulary. If you have a health insurance agent, they can assist in finding your plan’s formulary list. You can check insurance carrier websites to view the drug formularies they offer. Those with Medicare are eligible for a drug plan and should enroll as soon as possible.
What is formulary exception?
A Formulary Exception is a form of a request to determine coverage. By obtaining an exception, you may be able to get a drug that’s not on your plan’s formulary or ask your plan to bypass step therapy or prior authorizations.
What is Medicare Part D?
The Medicare Part D formulary is a list of drugs that have coverage under your policy. The formulary must include at least two drugs per category, and the insurance company can choose the options.
What is a formulary in Medicare?
The Medicare & You handbook defines a formulary as “a list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits.”. Most people simply refer to it as a drug list.
Why is formulary inclusive?
Cost savings is the reason a formulary inclusive of your medications is important. The drugs on these lists reflect those for which plans negotiate for the best price. The consequence of non-compliance with the list of covered drugs may result in your responsibility for full price versus a copayment or coinsurance.
What is Medicare Part D?
Medicare Part D is the prescription drug coverage for Medicare recipients. Part D plans are designed to defray the cost of your medications, but they do not kick in automatically when you enroll in Medicare Parts A and B. Once eligible, you would apply for the coverage through a private insurance company. Though all Part D plans are required ...
How long do you have to give a prescription drug plan to change the formulary?
Coverage rules and costs can change. Brand name drugs can be replaced by generic drugs. In these cases, the plan should give you at least 30 days of notice in writing before the effective date.
How long do you have to give a drug plan before the effective date?
Brand name drugs can be replaced by generic drugs. In these cases, the plan should give you at least 30 days of notice in writing before the effective date. Sometimes, the Food and Drug Administration (FDA) decides certain drugs are unsafe.
What to do if your insurance does not include your drug?
If the list of covered drugs does not include your specific drug, it will usually include one that is comparable. Consult with your physician in this case . If necessary, submit an exception request to your plan administrator.
Do all Part D plans have the same coverage?
Though all Part D plans are required to comply with the same standard federal government guidelines, there are differences in cost and coverage . Therefore, it is best to do some comparison shopping before making a decision. The first step is to look at each plan’s formulary.
What is a formulary in medicine?
formulary is more than a list of approved medications. A formulary must consist of drugs that will provide patients with a clinically appropriate medication for the course of treatment established by the physician. Consistent with industry standards/practices, the formulary is supported by a system of care management tools to consistently provide patients with access to medications that have been demonstrated to be safe, effective, and affordable, while maintaining and improving quality patient care. To ensure that Medicare prescription drug plans are following best practices, the CMS formulary review will follow four important principles.
What is the MMA in Medicare?
The addition of a prescription drug benefit to Medicare as a result of the MMA represents a landmark change to the Medicare program, a change that will significantly improve the healthcare coverage available to millions of Medicare beneficiaries. In the final regulation, we have included policies, such as formulary requirements and exceptions and appeals processes, to assure that beneficiaries have access to covered drugs that are medically necessary for their condition while enabling plans to design and manage their formularies to provide the most affordable benefit possible. We are also adjusting the payments to drug plans based on the expected costs of their enrollees, as well as implementing many other steps to limit the financial risk facing drug plans. Together, our goal is to provide a foundation for fair competition to offer high-quality coverage at the lowest cost to all types of Medicare beneficiaries, and to reward plans that focus on this critical policy goal.
Does CMS review drug lists?
Regardless of the classification system chosen, CMS will review and approve drug lists that are consistent with best practice formularies currently in widespread use today. The following paragraphs describe the multiple checks that will be utilized as part of the drug list review.
What Is a Formulary?
A drug formulary, or preferred drug list, is a continually updated list of medications and related products supported by current evidence-based medicine, judgment of physicians, pharmacists and other experts in the diagnosis and treatment of disease and preservation of health. The primary purpose of the formulary is to encourage the use of safe, effective and most affordable medications.
How does formulary system evolve?
Formulary systems evolve as new information becomes available or resources are developed . Since formulary decisions rely on published clinical information to make those decisions, it is important to have as much quality information as is available. It is estimated that in the coming years, comparative effectiveness research (CER) and genetic-based medicine, also referred to as personalized medicine, will impact formulary systems. The information gained through CER methodology and outcomes will provide P&T committees additional resources to evaluate the use of medication versus alternative treatment options. Through diagnostic tests and targeted therapies, personalized medicine may add complexity to the P&T committee decision making process. P&T committees will have to develop policies and procedures for making individual decisions in additional to the traditional population-based decisions.
What is a tiered pharmacy?
Many managed care organizations use a “tiered” pharmacy benefit design. All medications and related products subject to clinical review are assigned to a formulary “tier.” The tier represents the level of coverage the health plan will provide. The most cost-effective agents (often generics) are usually assigned to the most preferred tier and have the lowest patient out-of-pocket costs. The least cost-effective agents are usually assigned to the least preferred tier and have the highest patient out-of-pocket costs or offer no coverage. The preferred tier (s) are commonly referred to as “formulary” and non-preferred tier (s) as “non-formulary.” In other cases, non-formulary drugs are not assigned a tier and are not listed on the formulary. A formulary may be published in a variety of ways including by tier status, by therapeutic class or alphabetically.
What is a formulary management system?
Formulary management systems are routinely used by health plans, pharmacy benefit management companies (PBMs), hospitals and government agencies, including the Veterans Health Administration, Department of Defense, and Medicare and Medicaid programs. Formularies have evolved into a tool for assuring the selection of medications demonstrated to be safe, effective and affordable while maintaining or improving quality patient care.
What is the role of a pharmacist in formulary management?
Pharmacists often lead formulary management initiatives, coordinate P&T committee tasks and make recommendations based on sound clinical evidence. To ensure the success of the formulary management process, pharmacists guide P&T committees through the drug product selection process. Pharmacists also develop benefit related policies, therapeutic guidelines and design utilization management strategies. Pharmacists and physicians also serve as voting members on P&T committees.
How do P&T committees compare medications?
P&T committees compare medications by therapeutic classifications or upon similarities in clinical use. When two or more medications produce similar effectiveness and safety results in patients, then business elements like cost, supplier services, ease of delivery or other unique properties of the agents are considered when determining which agent to include on the formulary. In many organizations the P&T committee only performs clinical analyses; if two or more medications are determined to be clinically equivalent, then business elements will determine formulary inclusion or exclusion. The overall goal is to develop a list of the safest, most effective medications that will produce the desired goals of therapy at the most reasonable cost to the health care system.
How does formulary management affect health care?
In the face of the escalating number and complexity of drug products, rising drug prices and direct-to-consumer advertising , the formulary management process provides the managed health care system with the ability to objectively discriminate between superior and marginal medications. Such efficient and effective use of health care resources minimizes overall medical costs, improves patient access to more affordable care and provides an improved quality of life.
What Is A Formulary?
- A formulary is a list of generic and brand name drugs that are covered by a health plan. Pharmacy Benefit Dimensions (PBD) offers several formulary options for both our self-funded and Medicare Part D Prescription Drug Plan (PDP) Employer Group Waiver Plan (EGWP) clients.
What Is A Tier?
- A formulary is divided into various categories, or tiers. Drugs are placed in tiers based on the drug type. Drug types include generic, preferred brand, non-preferred brand and specialty. At PBD, we offer a variety of formulary options based on a tiering structure including: 1. Self-Funded Clients The standard PBD formulary is structured in a 3-tier format. There are approximately 5,465 (71%…
How Are PBD’s Formularies developed?
- Our formularies are developed by a Pharmacy and Therapeutics (P&T) Committee. The P&T Committee consists of 14 practicing physicians and 4 pharmacists. The identity of the committee members remains confidential to avoid undue pressure and lobbying from interested parties. Committee membership is reviewed annually.
What Does The Pt Committee do?
- The P&T Committee meets on a quarterly basis to review new drugs that are available in addition to reviewing existing classes and categories on the formularies. Additions, deletions and modifications are based on sound clinical evidence to make quality care available while appropriately containing costs. After discussing the clinical data correlating to each formulary u…
How Does This Benefit Our Clients?
- Our clinical team utilizes a value-based approach when making formulary decisions which focuses on low-cost therapeutic alternatives such as generic medications, to help balance efficacy, safety and cost-effectiveness. This is in stark contrast to a revenue or rebate driven formulary that would aggressively market brand name medications to secure rebates. While thi…