What is a Medicare drug plan coverage gap?
Most Medicare drug plans have a coverage gap (also called the "donut hole"). This means there's a temporary limit on what the drug plan will cover for drugs.
What is the coverage gap in Mrs Anderson's Medicare drug plan?
Mrs. Anderson reaches the coverage gap in her Medicare drug plan. She goes to her pharmacy to fill a prescription for a covered brand-name drug. The price for the drug is $60, and there's a $2 dispensing fee that gets added to the cost, making the total price $62.
When do I enter the coverage gap for Medicare Part D?
Once you and your plan have spent $4,020 on covered drugs in 2020, you're in the coverage gap. This amount may change each year. Also, people with Medicare who get Extra Help paying Part D costs won’t enter the coverage gap.
What counts as costs in the coverage gap?
Costs in the coverage gap 1 Brand-name prescription drugs. Once you reach the coverage gap in 2019,... 2 Generic drugs. In 2019, Medicare will pay 63% of the price for generic drugs during... 3 Items that count towards the coverage gap. 4 Items that don't count towards the coverage gap. 5 If you think you should get a discount.
Does the Medicare donut hole reset every year?
Your Medicare Part D prescription drug plan coverage starts again each year — and along with your new coverage, your Donut Hole or Coverage Gap begins again each plan year. For example, your 2021 Donut Hole or Coverage Gap ends on December 31, 2021 (at midnight) along with your 2021 Medicare Part D plan coverage.
What is the Medicare gap period?
The coverage gap begins after you and your drug plan have spent a certain amount for covered drugs. Once you and your plan have spent $4,430 on covered drugs in 2022, you're in the coverage gap. This amount may change each year.
What happens to the donut hole in 2021?
For 2021, the coverage gap begins when the total amount your plan has paid for your drugs reaches $4,130 (up from $4,020 in 2020). At that point, you're in the doughnut hole, where you'll now receive a 75% discount on both brand-name and generic drugs.
How long does the Medicare gap last?
When does the Medicare Donut Hole End? The donut hole ends when you reach the catastrophic coverage limit for the year. In 2022, the donut hole will end when you and your plan reach $7,050 out-of-pocket in one calendar year.
What is the Medicare donut hole 2022?
The Medicare Part D donut hole or coverage gap is the phase of Part D coverage after your initial coverage period. You enter the donut hole when your total drug costs—including what you and your plan have paid for your drugs—reaches a certain limit. In 2022, that limit is $4,430.
What is the coverage gap for 2022?
In 2022, the coverage gap ends once you have spent $7,050 in total out-of-pocket drug costs. Once you've reached that amount, you'll pay the greater of $3.95 or 5% coinsurance for generic drugs, and the greater of $9.85 or 5% coinsurance for all other drugs. There is no upper limit in this stage.
How do I get out of the donut hole?
In 2020, person can get out of the Medicare donut hole by meeting their $6,350 out-of-pocket expense requirement. However, there are ways to receive assistance for funding prescription drugs, especially if a person meets certain low income requirements.
Can you avoid the donut hole?
If you have limited income and resources, you may want to see if you qualify to receive Medicare's Extra Help/Part D Low-Income Subsidy. People with Extra Help see significant savings on their drug plans and medications at the pharmacy, and do not fall into the donut hole.
What is the best Medicare Part D plan for 2022?
The 5 Best Medicare Part D Providers for 2022Best in Ease of Use: Humana.Best in Broad Information: Blue Cross Blue Shield.Best for Simplicity: Aetna.Best in Number of Medications Covered: Cigna.Best in Education: AARP.
What year does Medicare donut hole end?
2020The Medicare donut hole is closed in 2020, but you still pay a share of your medication costs. Your coinsurance in the donut hole is lower today than in years past, but you still might pay more for prescription drugs than you do during the initial coverage stage.
How much is the donut hole in 2022?
Donut Hole: Who Pays What in Part D Medicare beneficiaries will see a Part D deductible up to $480 in 2022, followed by an Initial Coverage Period in which they will be responsible for 25% of costs up until they reach the threshold of $4,130 spent on prescription medications.
Is there still a donut hole in Medicare?
En español | The Medicare Part D doughnut hole will gradually narrow until it completely closes in 2020. Persons who receive Extra Help in paying for their Part D plan do not pay additional copays, even for prescriptions filled in the doughnut hole.
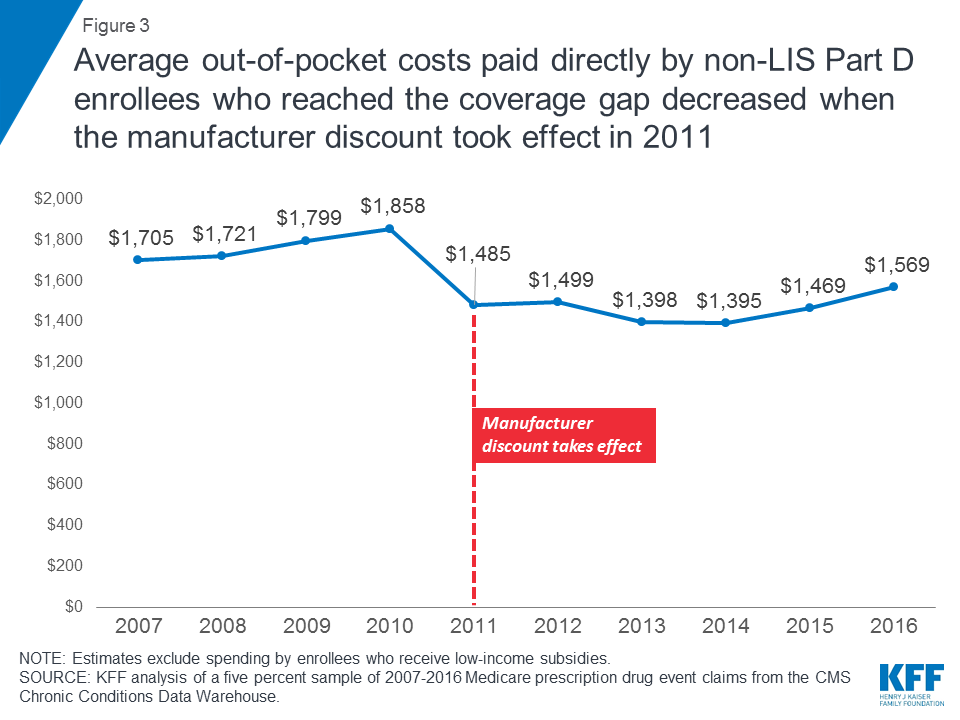
How much did Medicare increase in 2016?
will increase from $4,700 in 2015 to $4,850 in 2016. begins once you reach your Medicare Part D plan’s initial coverage limit ($3,310 in 2016) and ends when you spend a total of $4,850 in 2016.
What is the increase in the cost of a generic drug in 2016?
will increase to greater of 5% or $2.95 for generic or preferred drug that is a multi-source drug and the greater of 5% or $7.40 for all other drugs in 2016. will increase to $2.95 for generic or preferred drug that is a multi-source drug and $7.40 for all other drugs in 2016.
When will Medicare Part D enrollment start in 2022?
If you would like for us to send you an email as additional 2022 Medicare Part D plan information comes online and when enrollment begins (October 15th), please complete the form below. We will NOT share your information with any third-parties.
What is the Medicare budget for 2016?
The FY 2016 Budget includes a package of Medicare legislative proposals that will save a net $423.1 billion over 10 years. The proposals are scored off the President’s Budget adjusted baseline, which assumes a zero percent update to Medicare physician payments. These reforms will strengthen Medicare by more closely aligning payments with the costs of providing care, encouraging health care providers to deliver better care and better outcomes for their patients, and improving access to care for beneficiaries. The Budget includes investments to reform Medicare physician payments and accelerate physician participation in high-quality and efficient healthcare delivery systems. Finally, it makes structural changes in program financing that will reduce Federal subsidies to high income beneficiaries and create incentives for beneficiaries to seek high value services. Together, these measures will extend the Hospital Insurance Trust Fund solvency by approximately five years.
How much money did Medicare spend in 2016?
In FY 2016, the Office of the Actuary has estimated that gross current law spending on Medicare benefits will total $672.6 billion. Medicare will provide health insurance to 57 million individuals who are 65 or older, disabled, or have end-stage renal disease.
What is the 190 day limit for psychiatric services?
Eliminate the 190-day Lifetime Limit on Inpatient Psychiatric Facility Services: The 190-day lifetime limit on inpatient services delivered in specialized psychiatric hospitals is one of the last obstacles to behavioral health parity in the Medicare benefit. Beginning in FY 2016, this proposal would eliminate the 190-day limit and more closely align the Medicare mental health care benefit with the current inpatient physical health care benefit. Many beneficiaries who utilize psychiatric services are eligible for Medicare due to a disability, which means they are often younger beneficiaries who can easily reach the 190-day limit over their lifetimes. Therefore, this proposal would expand the psychiatric benefit and bring parity to the sites of service, while also containing the additional costs of removing the 190-day limit.
5.0 billion in costs over 10 years]
What is the authority for a program to prevent prescription drug abuse in Medicare Part D?
Establish Authority for a Program to Prevent Prescription Drug Abuse in Medicare Part D: HHS requires Part D sponsors to conduct drug utilization review, which assesses the prescriptions filled by a particular enrollee.
How many people are in Medicare Part D in 2016?
In 2016, the number of beneficiaries enrolled in Medicare Part D is expected to increase by about 3.5 percent to 43.7 million , including about 12.6 million beneficiaries who receive the low‑income subsidy.
How much has Medicare saved?
Cumulatively since enactment of the Affordable Care Act, 9.4 million beneficiaries have saved a total of $15 billion on prescription drugs. The FY 2016 Budget includes a package of Medicare legislative proposals that will save a net $423.1 billion over 10 years.
What are the goals of CMS for FY 2016?
Clinical Quality Improvement: The key goals for FY 2016 are improving the health status of communities; delivering patient-centered, reliable, accessible, and safe care; and better care at lower costs. Through improving cardiac health, reducing disparities in diabetic care, using immunization information systems and meaningful use of health IT to improve prevention coordination, CMS aims to improve the health status ofbeneficiaries. These goals will also be achieved by efforts to reduce healthcare‑associated infections, healthcare‑associated conditions in nursing homes, and hospital readmissions and adverse drug events.
Medicare Coverage Gap 1 – Part A Hospital Insurance
Medicare will pay when you go into the hospital. But you will also pay. You will pay, by benefit period:
Medicare Coverage Gap 2 – Skilled Nursing Facility
If you are in a skilled nursing facility for a Medicare covered event, you will pay:
Medicare Coverage Gap 5 – Benefit Periods
Medicare tracks your hospital or skilled nursing facility with benefit periods. A benefit period begins with your admission to the in-patient facility. The benefit period continues until 60 days past discharge. After you stay out of the facility for 60 days, a new benefit period begins. For each new benefit period, you pay for another deductible.
What to do about the Medicare Coverage Gap
The Medicare coverage gap can strain personal finances. MediGap insurance or a Medicare Advantage plan help to defray these costs. Check out the sponsored links or the government website to understand more about the Medicare coverage gap.