What are the requirements to qualify for Medicare Advantage?
There are 2 general eligibility requirements to qualify for a Medicare Advantage plan (Medicare Part C): 1. You must be enrolled in Original Medicare ( Medicare Part A and Part B). 2. You must live in the service area of a Medicare Advantage insurance provider that is accepting new users during your application period.
Who can sign up for Medicare Advantage?
Anyone who is enrolled in Original Medicare (Part A and Part B) may be eligible to sign up for a Medicare Advantage (Part C) plan. This includes people under the age of 65 who have qualified for Medicare because of a disability.
How much is Medicare Advantage 2021?
In 2021, the weighted average premium for a Medicare Advantage plan that includes prescription drug coverage is $33.57 per month. 1. 89 percent of Part C plans available throughout the country in 2021 cover prescription drugs, and 54 percent of those plans feature a $0 premium.
How long does Medicare enrollment last?
When you first become eligible for Medicare, you will be given an Initial Enrollment Period (IEP). Your IEP lasts for seven months. It begins three months before you turn 65 years old, includes the month of your birthday and continues on for three more months.
What is Medicare Part C?
Medicare Part C plans are sold by private insurance companies as an alternative to Original Medicare. Medicare Part C plans are required by law to offer at least the same benefits as Medicare Part A and Part B. There are several different types of Medicare Advantage plans, such as HMO plans and PPO plans. Each type of plan may feature its own ...
When is the Medicare open enrollment period?
The Medicare AEP lasts from October 15 to December 7 each year. During this time, you may be able to sign up for, change or disenroll from a Medicare Advantage plan.
Does Medicare Part A have an out-of-pocket limit?
Medicare Part A and Part B don't include an out-of-pocket spending limit. Medicare out-of-pocket costs can add up quickly if you're faced with a long-term inpatient hospital stay or undergo extensive medical care that requires high coinsurance or copay costs.
What is Medicare Advantage Plan?
Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are an “all in one” alternative to Original Medicare. They are offered by private companies approved by Medicare. If you join a Medicare Advantage Plan, you still have. Medicare.
Can't offer drug coverage?
Can’t offer drug coverage (like Medicare Medical Savings Account plans) Choose not to offer drug coverage (like some Private Fee-for-Service plans) You’ll be disenrolled from your Medicare Advantage Plan and returned to Original Medicare if both of these apply: You’re in a Medicare Advantage HMO or PPO.
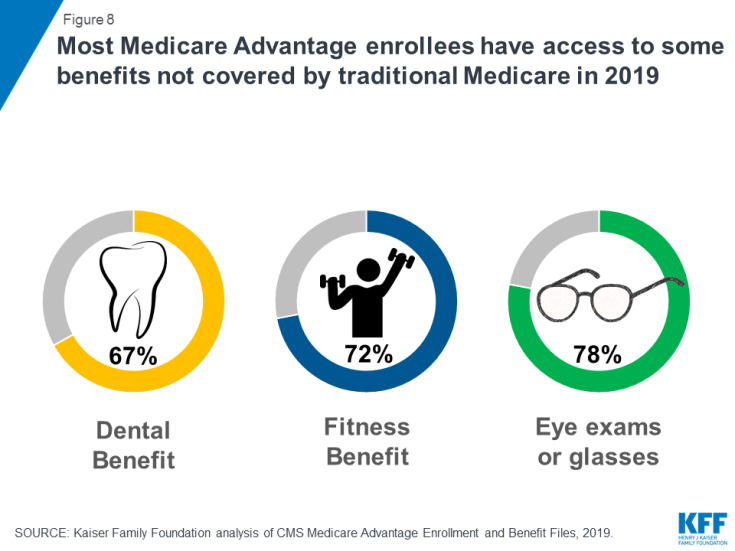
Does Medicare cover dental?
Covered services in Medicare Advantage Plans. Most Medicare Advantage Plans offer coverage for things Original Medicare doesn’t cover, like some vision, hearing, dental, and fitness programs (like gym memberships or discounts). Plans can also choose to cover even more benefits. For example, some plans may offer coverage for services like ...
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
Can a provider bill you for PFFS?
The provider shouldn’t provide services to you except in emergencies, and you’ll need to find another provider that will accept the PFFS plan .However, if the provider chooses to treat you, then they can only bill you for plan-allowed cost sharing. They must bill the plan for your covered services. You’re only required to pay the copayment or coinsurance the plan allows for the types of services you get at the time of the service. You may have to pay an additional amount (up to 15% more) if the plan allows providers to “balance bill” (when a provider bills you for the difference between the provider’s charge and the allowed amount).
What is Medicare Advantage?
According to Medicare.gov, Medicare Advantage (also known as Medicare Part C) plans are a type of Medicare health plan. They are offered by a private company that contracts with Medicare to provide all your Part A and Part B benefits. In addition, most Medicare services are covered through Medicare Advantage.
Who Qualifies for Medicare Advantage?
Finding the right doctor who accepts Medicare Advantage can be difficult. However, there are plenty of ways to find the one who is right for you. If you are unhappy with your current plan or doctor, take advantage of the annual Medicare open enrollment period from October 15 to December 7.
Can I Switch From a Medicare Advantage Plan back to Original Medicare?
You can switch plans by joining the plan of your choice during enrollment periods. You will be automatically disenrolled from your old plan when your new plan begins. Enrollment periods for switching back to Original Medicare are October 15 through December 7 and January 1-March 31.
What to do if you don't qualify for Medigap?
If you don’t qualify for Medigap or it’s too far out of your budget, please consider a Medicare Advantage plan. Whether you choose Medigap or Advantage, it’s always better to have some coverage. You don’t want to find yourself in a situation where you owe tens of thousands of dollars in healthcare costs.
Is it 100% your responsibility to see a doctor in Florida?
The thing is, you HAVE to use the network of doctors they allow. So, if you’re visiting family in Florida, a doctor’s visit could be 100% your responsibility. Or, if you have a specialist that isn’t in the network, if you see that doctor, the cost is all on you.
Is Medigap better than Advantage?
With Medigap, a referral is a thing of the past. While there are many reasons to say Medigap is more comprehensive than Advantage, some coverage is always better than no coverage.
Can you leave Medicare if you have a new plan?
Medicare, by itself, can be costly. Never leave your policy until you have a new plan in place. You never want to have a lapse in coverage. If you rely on an Advantage plan to give you Part D benefits, don’t forget to enroll in a stand-alone policy.
Can low income people get Medicare?
Low-income or Medicaid eligible beneficiaries may qualify for extra help paying for premiums, de ductibles, and copa yments. Those with End-Stage Renal Disease may qualify for a Medicare Advantage plan. Also, there are Special Needs Plans for those with chronic issues.
How old do you have to be to get Medicare Advantage?
How Does Medicare Advantage Reimbursement Work? In the United States, you are eligible to enroll in a Medicare Advantage plan if you are either 65 years of age or older, are under 65 with certain disabilities.
Where does Medicare Advantage money come from?
The money that the government pays to Medicare Advantage providers for capitation comes from two U.S. Treasury funds.
What is Medicare Advantage Reimbursement?
Understanding Medicare Advantage Reimbursement. The amount the insurance company receives from the government for you as a beneficiary is dependent upon your individual circumstances. As a beneficiary of a Medicare Advantage plan, if your monthly health care costs are less than what your insurance carrier receives as your capitation amount, ...
What is the second fund in Medicare?
The second fund is the Supplementary Medical Insurance Trust which pays for what is covered in Part B, Part D, and more. As a beneficiary enrolled in a Medicare Advantage plan, you will also be responsible for some of the costs of your healthcare.
Does Medicare Advantage cover dental?
Medicare Advantage plans must provide the same coverage as Parts A and B, but many offer additional benefits, such as vision and dental care, hearing exams, wellness programs, and Part D, prescription drug coverage.
Is Medicare Part C required?
Having a Medicare Part C plan is not a requirement for Medicare coverage, it is strictly an option many beneficiaries choose. If you decide to enroll in a Medicare Advantage plan, you are still enrolled in Medicare and have the same rights and protection that all Medicare beneficiaries have.