What if I disagree with a Medicare decision?
Mar 07, 2022 · If your first-level appeal is denied, you may appeal to the next level and the next. The fifth-level appeal, if you reach it, is decided by a judicial review in a federal district court. Filing an Appeal with Medicare . You can file a first-level appeal for coverage or payment denied by Medicare by completing a Redetermination Request Form. You must file your appeal within …
How to appeal when someone with Medicare is being discharged?
Filing an initial appeal for Medicare Part A or B: File your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that lists the denied claim. Circle the item on your MSN that you are appealing and clearly explain why you think Medicare’s decision is …
How do I file an appeal to a Medicare claim?
Original Medicare? The appeals process has 5 levels: Level 1: Redetermination by the Medicare Administrative Contractor (MAC) Level 2: Reconsideration by a Qualified Independent Contractor (QIC) Level 3: Decision by the Office of Medicare Hearings and Appeals (OMHA) Level 4: Review by the Medicare Appeals Council (Appeals Council) Level 5: Judicial Review by a Federal …
How to appeal a Medicaid Managed Care Plan Decision?
Aug 05, 2021 · Always writing your Medicare number on all documents submitted with an appeal request. Keeping a copy of everything you send to Medicare, a Medicare Administrative Contractor, or your Medicare health plan. The most important tip is to file a claim. Medicare appeals can only have success if they are filed.

What are the chances of winning a Medicare appeal?
People have a strong chance of winning their Medicare appeal. According to Center, 80 percent of Medicare Part A appeals and 92 percent of Part B appeals turn out in favor of the person appealing.Jun 20, 2013
What should I say in a Medicare appeal?
What are the steps for filing an appeal for original Medicare?your name and address.your Medicare number (as shown on your Medicare card)the items you want Medicare to pay for and the date you received the service or item.the name of your representative if someone is helping you manage your claim.More items...•Nov 12, 2020
How do I write a Medicare appeal letter?
Include this information in your written request:Your name, address, and the Medicare Number on your Medicare card [JPG]The items or services for which you're requesting a reconsideration, the dates of service, and the reason(s) why you're appealing.More items...
What are the 5 levels of appeal for Medicare?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court.
Can you be denied Medicare?
In all but four states, insurance companies can deny private Medigap insurance policies to seniors after their initial enrollment in Medicare because of a pre-existing medical condition, such as diabetes or heart disease, except under limited, qualifying circumstances, a Kaiser Family Foundation analysis finds.Jul 11, 2018
How do I appeal Medicare underpayment?
You can appeal an underpayment by timely submitting a request for a redetermination appeal to your regional contractor (e.g. Palmetto-GBA for California).
How do you write an appeal letter template?
Dear [Recipient's name], [Recipient's title, if sending an email without the above information], I am writing to appeal [decision] on [date of action]. I was informed that [reason for action]. I am appealing this decision because I feel that [reason for appealing].Sep 20, 2021
How do you fight Medicare?
Visit Medicare.gov/appeals. Call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048. Visit Medicare.gov/forms-help-resources/medicare-forms for appeals forms.
What is a Medicare reconsideration?
If you disagree with the initial decision from your plan (also known as the organization determination), you or your representative can ask for a reconsideration (a second look or review). You must ask for a reconsideration within 60 days of the date of the organization determination.
How long does Medicare have to respond to an appeal?
The Council generally decides within 90 days of the OMHA disposition or dismissal review request receipt date. If the Council review comes from an escalated appeal, the Council has 180 days from the escalation request receipt date to issue a decision.
How long does it take to appeal a Medicare claim?
You can file a first-level appeal for coverage or payment denied by Medicare by completing a Redetermination Request Form. You must file your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that first reported the service or item.
How to appeal a Medicare denial?
You may file an appeal if you disagree with a coverage or payment decision made by Medicare or by your Medicare health or prescription drug plan. You may appeal if you receive a denial any of the following: 1 A health care service, supply, item or prescription drug that you think you should be able to get or continue to get 2 Payment for a health care service, supply, item or a prescription drug you already got 3 Request to change the amount you must pay for a health care service, supply, item, or prescription drug
What is a Medicare redetermination notice?
It may come as a separate notice or it may be included in a future MSN. The notice will explain the decision and what you can do to appeal to the next level.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
What is an appeal for a denial of a health care service?
You may appeal if you receive a denial any of the following: A health care service, supply, item or prescription drug that you think you should be able to get or continue to get. Request to change the amount you must pay for a health care service, supply, item, or prescription drug. The appeals process has five levels.
What to include in Medicare appeal?
In general, the request should include: Your name, address, and the Medicare number shown on your Medicare card. Description of the items or services for which you’re requesting a reconsideration, including the dates of service and the reason for your appeal. ...
How many levels of appeals are there?
The appeals process has five levels. The first level asks Medicare or your Medicare health or prescription drug plan for a “redetermination” on the original request. If your first-level appeal is denied, you may appeal to the next level and the next. The fifth-level appeal, if you reach it, is decided by a judicial review in a federal district ...
What happens if you disagree with a Medicare decision?
If you disagree with a decision about one of your Medicare claims, you have the right to challenge that decision and file an appeal. Situations in which you can appeal include: Denials for health care services, supplies or prescriptions that you have already received. For example: During a medical visit your doctor conducts a test.
How to report Medicare not paying?
If you still have questions about a claim you think Medicare should not have paid, report your concerns to the Medicare at 1-800-MEDICARE. Make copies for your records of everything you are submitting. Send the MSN and any additional information to the address listed at the bottom on the last page of your MSN.
How long does it take to appeal Medicare?
The final level of appeal is to the federal courts. You generally have 60 days to file appeals before an ALJ, the Medicare Appeals Council and to federal court.
What to do if Medicare Advantage decision is not in your favor?
In addition, Medicare Advantage companies must give patients a way to report grievances about the plan and the quality of care they receive from providers in the plan.
Why does Medicare reject my doctor's recommendation?
For example: Your Medicare Part D drug plan rejects your doctor’s recommendation that you receive a discount on an expensive medication because the available lower-cost drugs are not effective for your condition.
When a doctor submits a claim to be reimbursed for that test, what does Medicare determine?
When the doctor submits a claim to be reimbursed for that test, Medicare determines it was not medically necessary and denies payment of the claim. Denials of a request you or your doctor made for a health care service, supply or prescription. For example: Medicare determines that a wheelchair is not medically necessary for your condition.
How to request a plan exception?
Requests for plan exceptions can be made by phone or in writing if you are asking for a prescription drug you haven’t yet received. If you are asking to be reimbursed for the price of drugs you have already bought, you must make your request in writing.
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
What to do if you are not satisfied with QIC?
If you’re not satisfied with the QIC’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or , in certain circumstances, a review of the appeal record by an ALJ or attorney adjudicator.
What is a QIC?
QIC is an independent contractor that didn’t take part in the level 1 decision. The QIC will review your request for a reconsideration and will make a decision.
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
What happens if you disagree with a decision?
If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you’ll get instructions on how to move to the next level of appeal.
What is an organization determination?
You have the right to ask your plan to provide or pay for items or services you think it should cover, provide, or continue. The decision by the plan is called an “organization determination.” You, your representative, or your doctor can request an organization determination from your plan in advance to make sure that the services are covered. If the plan denies coverage or payment after you receive services, that denial is the organization determination that you can appeal.
What is a home health change of care notice?
The “Home Health Change of Care Notice” is a written notice that your home health agency should give you when your home health plan of care is changing because of one of these:
What to do if you decide to appeal a health care decision?
If you decide to file an appeal, ask your doctor, health care provider, or supplier for any information that may help your case. If you think your health could be seriously harmed by waiting for a decision about a service, ask the plan for a fast decision.
What happens if my Medicare plan doesn't decide in my favor?
Then, if your plan doesn't decide in your favor, the appeal is reviewed by an independent organization that works for Medicare, not for the plan.
What types of Medicare decisions can I appeal?
You have the right to dispute decisions from Medicare, a Medicare health plan, or a Medicare Part D prescription drug plan that involve:
How do I start the appeals process?
Where you begin in the appeals process depends on the nature of your Medicare problem and the urgency of the needed solution.
How do I appeal if I have original Medicare?
Original Medicare includes Part A (hospital insurance) and Part B (medical insurance).
How do I appeal if I have Medicare Advantage?
Medicare Advantage plans — also known as Part C — which bundle Medicare Parts A, B, and, usually, D together, are alternative ways to get Medicare benefits. Medicare Advantage plans are sold by private insurers that Medicare approves.
How do I appeal if I have a Medicare drug plan?
Prescription drug coverage is available as an add-on to original Medicare called Medicare Part D, or as a prescription drug benefit included with a Medicare Advantage plan or other Medicare plan.
How do I maximize my chances of winning an appeal?
There are several ways to increase your chances of winning an appeal, including:
Where can I find help for my Medicare appeal?
In addition to consulting your provider, the Centers for Medicare & Medicaid Services (CMS) offers many online Medicare resources for appeals. CMS also provides a Medicare telephone helpline at 1-800-MEDICARE ( 1-800-633-4227 ).
What is the TTY number for a prescription drug?
TTY users call 711. Monday through Friday, 8 a.m. to 8 p.m. Fill out a form. You can ask us to review a decision we made related to prescription drugs using the Request for Redetermination form (PDF). Mail or fax your appeal.
How long does it take to get a fast appeal?
If waiting could cause serious harm to your health or hurt your ability to function, you’ll hear from us within 72 hours. Your doctor should request a fast appeal.
What is BCMP in Medicare?
The Beneficiary Care Management Program (BCMP) is a CMS Person and Family Engagement initiative supporting Medicare Fee-for-Service beneficiaries undergoing a discharge appeal, who are experiencing chronic medical conditions requiring lifelong care management. It serves as an enhancement to the existing beneficiary appeals process. This program is not only a resource for Medicare beneficiaries, but extends support for their family members, caregivers and providers as active participants in the provision of health care delivery.
What is coinsurance in Medicare?
An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%). The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay.
How long before discharge do you have to sign a copy of your IM?
Information on your right to get a detailed notice about why your covered services are ending. If the hospital gives you the IM more than 2 days before your discharge day, it must give you a copy of your original, signed IM or provide you with a new one (that you must sign) before you're discharged.
What is a fast appeal?
A fast appeal only covers the decision to end services. You may need to start a separate appeals process for any items or services you may have received after the decision to end services. For more information, view the booklet Medicare Appeals . You may be able to stay in the hospital (. coinsurance.
What is your right to be involved in a hospital decision?
Your right to be involved in any decisions that the hospital, your doctor, or anyone else makes about your hospital services and to know who will pay for them. Your right to get the services you need after you leave the hospital. Your right to appeal a discharge decision and the steps for appealing the decision.
What is your right to get all?
Your right to get all. medically necessary. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine. hospital services.
Does Medicare cover hospital admissions?
Medicare will continue to cover your hospital stay as long as medically necessary (except for applicable coinsurance or deductibles) if your plan previously authorized coverage of the inpatient admission, or the inpatient admission was for emergency or urgently needed care.
What should a Medicare appeal letter include?
Finally the Medicare appeal letter itself should include all relevant details. Outline the facts and dates of service and any doctor’s orders that affect your claim. Keep it professional. When Medicare or an insurance company denies a claim, we become angry or emotional.
What happens if you miss a Medicare letter?
If they get no reply, they notify Medicare and Medicare assesses a late penalty. When Medicare does this, the Part D carrier MUST comply. They must charge you the penalty – they have no choice.
How long does Medicare cover SNF?
It will cover up to 100 days in a SNF, with the goal being that the beneficiary can then resume normal self-care. Medicare Advantage plans follow these same rules. It appeared Joe was refusing to try to get well, so the carrier actually did have grounds to deny the claim.
What happened to the man who fell on his back?
The fall had caused him to break his arm and bruise his back. Upon admittance to the hospital, he was diagnosed with low blood pressure, low oxygen and a severe and debilitating UTI. This infection, coupled with the pain medication he was given, had left him feeling weak, foggy and confused.
Does Medicare pay for skilled nursing facilities?
The Medicare Advantage carrier then denied payment for the Skilled Nursing Facility (SNF). Their denial stated that Joe had “refused to participate” in therapy that would begin his rehabilitation. Medicare generally does not provide skilled nursing facility care for beneficiaries who are not expected to recover.
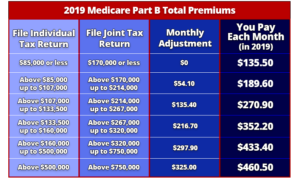
How is IRMAA calculated?
The IRMAA is based on information from the individual’s income tax return obtained from the Internal Revenue Service (IRS) and calculated according to a mathematical formula established by law. The IRMAA is then added to the standard premium amount to calculate the beneficiary’s total monthly Part B insurance premium.
How to request reconsideration of Social Security?
A request for reconsideration can be done orally by calling the SSA 1-800 number (800.772.1213) as well as by writing to SSA .
What are the circumstances that qualify a beneficiary for a new Part B determination?
Below are the situations which may qualify a beneficiary for a new Part B determination: Events that result in the loss of dividend income or affect a beneficiary's expenses, but do not affect the beneficiary's modified adjusted gross income are not considered qualifying life-changing events.
What is a work stoppage?
Work stoppage. Loss of income from income producing property. Loss or reduction of certain kinds of pension income. Events that result in the loss of dividend income or affect a beneficiary's expenses, but do not affect the beneficiary's modified adjusted gross income are not considered qualifying life-changing events.
What are the life changing events?
There are 7 qualifying life-changing events: 1 Death of spouse 2 Marriage 3 Divorce or annulment 4 Work reduction 5 Work stoppage 6 Loss of income from income producing property 7 Loss or reduction of certain kinds of pension income
Who is responsible for determining a beneficiary's Social Security benefits?
The Social Security Administration (SSA) notifies a beneficiary of his or her Part B insurance premium and any IRMAA with the beneficiary’s annual notice of Social Security benefits (referred to as an initial determination). SSA is responsible for issuing all initial and reconsideration determinations.