Applying to become a Medicare provider
- Obtain an NPI Psychologists seeking to become Medicare providers must obtain a National Provider Identifier (NPI) before attempting to enroll in Medicare. ...
- Complete the Medicare Enrollment Application Once a psychologist has an NPI, the next step is to complete the Medicare Enrollment Application. ...
- Select a Specialty Designation
How do you become a Medicare provider?
- CMS-855A for Institutional Providers
- CMS-855B for Clinics, Group Practices, and Certain Other Suppliers
- CMS-855I for Physicians and Non-Physician Practitioners
- CMS-855R for Reassignment of Medicare Benefits
- CMS-855O for Ordering and Certifying Physicians and Non-Physician Practitioners
- CMS-855S for DMEPOS Suppliers
- CMS-20134 (PDF) for MDPP Suppliers
How to become Medicare Certified Provider?
- Public agency is an agency operated by a State or local government. Examples include State-operated HHAs and county hospitals. ...
- Nonprofit agency is a private (i.e., nongovernmental) agency exempt from Federal income taxation under §501 of the Internal Revenue Code of 1954. ...
- Proprietary agency is a private, profit-making agency or profit-making hospital.
How to credential a provider with Medicare?
- Obtain DMEPOS accreditation from a CMS-approved organization
- Enroll in the Medicare program as a DMEPOS Supplier
- Post a surety bond to the National Supplier Clearinghouse (NSC)
How to find Medicaid number for provider?
- Payment Limit Demonstrations
- Disproportionate Share Hospitals
- Medicaid Administrative Claiming
- State Budget & Expenditure Reporting for Medicaid and CHIP
- Provider Preventable Conditions
- Actuarial Report on the Financial Outlook for Medicaid
- Section 223 Demonstration Program to Improve Community Mental Health Services
Which of the following are steps to becoming a Medicare provider?
Applying to become a Medicare providerStep 1: Obtain an NPI. Psychologists seeking to become Medicare providers must obtain a National Provider Identifier (NPI) before attempting to enroll in Medicare. ... Step 2: Complete the Medicare Enrollment Application. ... Step 3: Select a Specialty Designation.
What does it mean to be credentialed with Medicare?
Credentialing is the process of approving a physician, agency or other medical provider as part of the Medicare supply chain.
What is a Pecos provider?
PECOS stands for Provider, Enrollment, Chain, and Ownership System. It is the online Medicare enrollment management system that allows individuals and entities to enroll as Medicare providers or suppliers.
What types of providers can bill Medicare?
Medicare also covers services you get from other health care providers, like:Physician assistants.Nurse practitioners.Clinical social workers.Physical therapists.Occupational therapists.Speech language pathologists.Clinical psychologists.
How long is the credentialing process?
90 to 120 daysA standard credentialing process takes from 90 to 120 days based on the guidelines. In some cases, the process may be completed within 90 days and sometimes, it can take more than 120 days. Keeping in mind, the complexities in medical credentialing, it is best to hire experts in the field.
How often does a provider need to be credentialed?
every three yearsHealthcare providers need to be re-credentialed at least every three years. Some healthcare facilities or insurance companies perform recredentialing even more often.
How do I apply for a NPI number online?
Visit the NPPES website In the national plan and provider enumeration system website, navigate to the NPI webpage, and look under how to apply for an NPI for individual providers. Create a login through the identity and access management system.
Who should enroll in Pecos?
CMS developed PECOS as a result of the Patient Protection and Affordable Care Act. The regulation requires all physicians who order or refer home healthcare services or supplies to be enrolled in Medicare.
How do I enroll in Pecos?
0:146:13Number if you do not already have an active NPI number you can register for one through the nationalMoreNumber if you do not already have an active NPI number you can register for one through the national plan and provider enumeration system or n Pez.
How are Medicare providers paid?
In general, Medicare pays each of these providers separately, using payment rates and systems that are specific to each type of provider. The remaining share of Medicare benefit payments (37%) went to private plans under Part C (the Medicare Advantage program; 26%) and Part D (the Medicare drug benefit; 11%).
What Does Medicare pay for doctors visits?
If you see a GP Medicare will pay 100% of the cost if the GP bulk bills. If they don't bulk bill, Medicare will pay 100% of the public rate and you will have to pay any extra if the doctor charges more.
How do providers get reimbursed by Medicare?
Traditional Medicare reimbursements When an individual has traditional Medicare, they will generally never see a bill from a healthcare provider. Instead, the law states that providers must send the claim directly to Medicare. Medicare then reimburses the medical costs directly to the service provider.
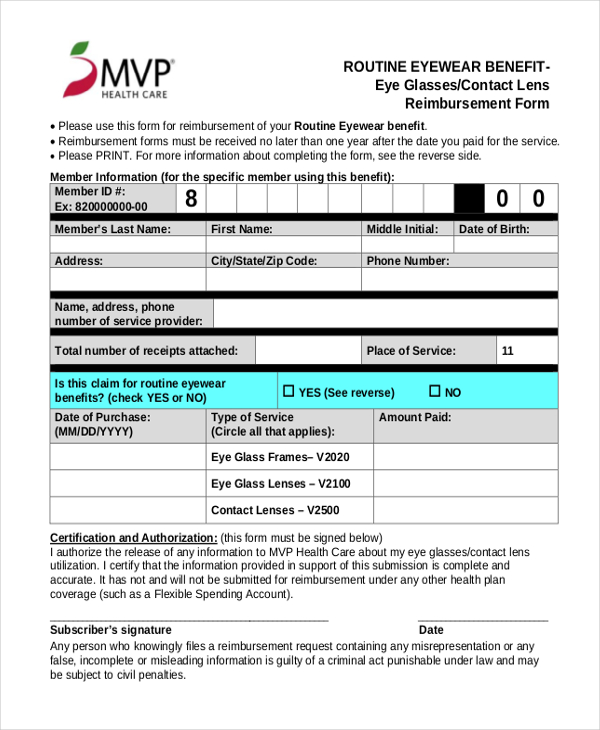
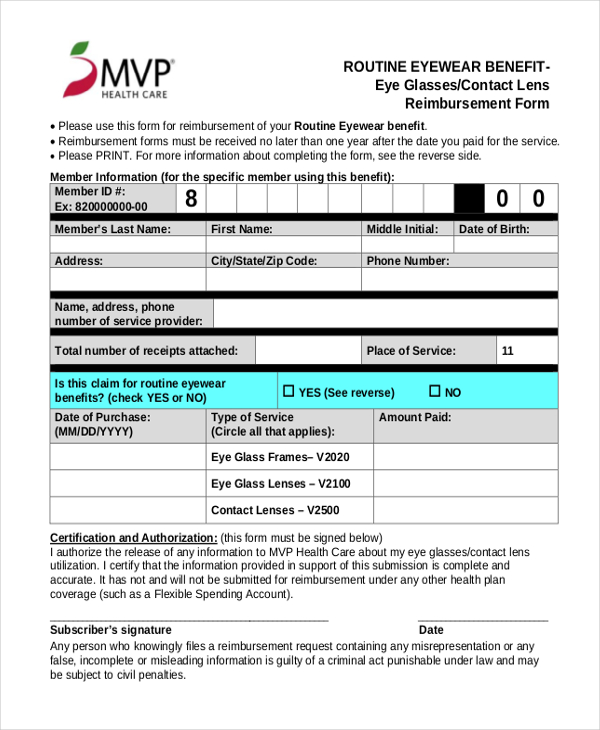
Submit The Following To The Fiscal Intermediary
The Provider/Supplier Enrollment Application Form is a requirement of the application process. To obtain this form, click on the CMS-855 link above or call the fiscal intermediary at 696-0705 or visit their website at www.palmettogba.com/medicare.
Become A Medicare Provider Or Supplier
Ready to become a Medicare provider or supplier? This guide will help you enroll in three steps.
Determine Eligibility As Medicare Provider
Determining your eligibility as a Medicare provider is the next step. To be eligible, you may need to be certified with the Conditions of Participation. The Centers for Medicare and Medicaid Services relies on state agencies to determine the eligibility of most providers.
Determining Your Eligibility As A Medicare Provider
1 Learn the types of Medicare. Any physician or non-physician medical care or supply provider who offers services or goods necessary for the physical and mental health of those who receive Medicare coverage are eligible to apply as providers.
Applying As A National Medicare Provider
1 Register with the National Plan & Provider Enumeration System . Youll need to create a user ID that will be used to obtain your National Provider Identifier, and this same log in information will be used to log into the Provider Enrollment, Chain, and Ownership Systems website where you will apply to become a Medicare provider.
Medicare Application Process And Forms
The Centers for Medicare and Medicaid Services determines whether a provider can participate in the Medicare program with the help of its regional home health intermediary.
How Do I Become Medicare Accredited
Step 1: Obtain an NPI. Psychologists seeking to become Medicare providers must obtain a National Provider Identifier before attempting to enroll in Medicare.
Section 2A, 2B: Identifying Information and Correspondence Address
The correspondence address cannot be the address of a billing company or other third party, it must be a direct connection to the provider.
Section 4
Practice Location Information begins collecting the details about the business entity, service locations, and payment address.
Section 6: Individuals having managing control
This section must list the name and identifying information of Dr. James. Dr. James would also need to make an additional copy of this page for an office manager or any other person who is responsible for managing the business of the practice.
Things to remember
Review your application and supporting documents to ensure the following items won’t cause a delay in your application:
Summary
Enrolling in the Medicare program can be time consuming and frustrating. Using the PECOS online enrollment system is often more efficient than a paper application. However, some of the MACs have proven problematic at accurately transferring application information to and from PECOS.
What is a Medicare provider number?
The article states that “A Medicare provider number is known as a “national provider identifier,” a ten-digit identification number for covered health care providers”. Obviously whoever wrote the article doesn’t understand the US Healthcare industry. Click here for an accurate description of how to obtain a Medicare Provider Number.
Do I need an NPI to enroll in Medicare?
Different provider types have varying enrollment requirements so become familiar with what your carrier needs to properly enroll you and/or your group. Yes, you must have an NPI to do business with any health insurance company including Medicare. But, your NPI is NOT your Medicare provider number.
What information do you need to release a private health insurance beneficiary?
Prior to releasing any Private Health Information about a beneficiary, you will need the beneficiary's last name and first initial, date of birth, Medicare Number, and gender. If you are unable to provide the correct information, the BCRC cannot release any beneficiary specific information.
When does Medicare use the term "secondary payer"?
Medicare generally uses the term Medicare Secondary Payer or "MSP" when the Medicare program is not responsible for paying a claim first. The BCRC uses a variety of methods and programs to identify situations in which Medicare beneficiaries have other health insurance that is primary to Medicare.
What is BCRC in Medicare?
The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries. The purpose of the COB program is to identify the health benefits available to a Medicare beneficiary and to coordinate the payment process to prevent mistaken Medicare payment. The BCRC does not process claims or claim-specific inquiries. The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
What is MLN CMS?
The Medicare Learning Network (MLN) is a CMS initiative to ensure Medicare physicians, providers and supplies have immediate access to Medicare coverage and reimbursement rules in a brief, accurate, and easy to understand format. To access MLN Matters articles, click on the MLN Matters link.
Can a Medicare claim be terminated?
Medicare claims paying offices can terminate records on the CWF when the provider has received information that MSP no longer applies (e.g., cessation of employment, exhaustion of benefits). Termination requests should be directed to your Medicare claims payment office.
How long does it take to change your Medicare billing information?
It’s important to keep your enrollment information up to date. To avoid having your Medicare billing privileges revoked, be sure to report any change within 30 days. Changes include, but are not limited to: a change in ownership. an adverse legal action. a change in practice location.
What is DMEPOS in Medicare?
Suppliers who receive Medicare reimbursement for durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) are required to: If your business doesn’t dispense or furnish DMEPOS, you should use the Medicare Enrollment Guide for Providers & Suppliers.
