How do I get an EOB from Medicare?
claims:Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. ... Use Medicare's Blue Button by logging into your secure Medicare account to download and save your Part D claims information. ... For more up-to-date Part D claims information, contact your plan.
Can I get my Medicare Summary Notice Online?
Yes, Medicare summary notices are available online — but you must sign up to receive them electronically. If you opt for electronic notices, you'll stop receiving printed copies of your MSNs in the mail. Instead, you'll get an email every month from your online My Medicare Account.
How do I view my Medicare bills?
For questions about your Medicare bill or if your payment was processed:Log into (or create) your Medicare account. Select “My premiums,” then, “Payment history.”Call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048.
Can I view my Medicare bill online?
You can use your online MyMedicare account to view your Medicare premium bills, check your payment history and set up Medicare Easy Pay for auto payments.
What is Medicare Summary Notice?
It's a notice that people with Original Medicare get in the mail every 3 months for their Medicare Part A and Part B-covered services. The MSN shows: All your services or supplies that providers and suppliers billed to Medicare during the 3-month period. What Medicare paid. The maximum amount you may owe the provider.
How often do Medicare statements come out?
MSNs are usually mailed four times a year (quarterly) and contain information about charges billed to Medicare, the amount that Medicare paid, and the amount you are responsible for. Note that you may receive additional MSNs if you receive reimbursement for a bill you paid.
Is Medicare premium automatically deducted from Social Security?
Yes. In fact, if you are signed up for both Social Security and Medicare Part B — the portion of Medicare that provides standard health insurance — the Social Security Administration will automatically deduct the premium from your monthly benefit.
Why is my Medicare bill so high?
Medicare Part B covers doctor visits, and other outpatient services, such as lab tests and diagnostic screenings. CMS officials gave three reasons for the historically high premium increase: Rising prices to deliver health care to Medicare enrollees and increased use of the health care system.
How often does Medicare bill for Part B?
Part B premiums You pay a premium each month for Part B. Your Part B premium will be automatically deducted from your benefit payment if you get benefits from one of these: Social Security. Railroad Retirement Board.
Does Medicare send you a bill?
Most people don't get a bill from Medicare because they get these premiums deducted automatically from their Social Security (or Railroad Retirement Board) benefit.) Your bill pays for next month's coverage (and future months if you get the bill every 3 months). Your bill lists the dates you're paying for.
What is an Explanation of Benefits?
The first thing to know about an Explanation of Benefits is that it’s not a bill. Instead, it’s a summary of the claims and charges applied to your...
Who Receives an EOB?
Anyone enrolled in Medicare Advantage and Medicare Prescription Drug Plan (Part D) will receive an EOB when they use their policy. You don’t need t...
How Do I Read My EOB?
You can expect to see a few standard terms, no matter who sends your Explanation of Benefits. They are:
Can I Get Another Copy of my EOB?
If you misplaced your most recent EOB or didn’t receive it in the mail, contact your insurance company. A representative should be able to provide...
I’m on Original Medicare (Parts A and B) -- Do I get an EOB?
No, but you’ll receive a Medicare Summary Notice (MSN), the Medicare explanation of benefits. Like the EOB, the MSN is not a bill — it’s a monthly...
Does my EOB show specific prescription info?
If you have a Medicare Prescription Drug EOB, it can show which medicines you’re taking, how much they cost, and how much your insurance covers. [i]
Will I get an EOB each month if I don't see a doctor?
Your insurance company is only required to send you an EOB when you make a claim. This happens any time you see a healthcare provider through your...
What is EOB in Medicare?
Explanation of Benefits (EOB) go to enrollees in Medicare Advantage. Medicare Advantage ( Medicare Part C) is health insurance for Americans aged 65 and older that blends Medicare benefits with private health insurance. This typically includes a bundle of Original Medicare (Parts A and B) and Medicare Prescription Drug Plan (Part D).
What is coinsurance for medical bills?
Coinsurance is the percentage of your medical costs that you pay after you meet your deductible. Your insurance company pays the remaining amount. For example: If you have a $1,000 medical bill and your coinsurance is 20%, you'll pay $200. Your insurance company will cover the final $800.
Does Medicare Advantage have an EOB?
Each plan has its own EOB form; private insurance companies provide Medicare Advantage and Part D, and your EOB will come directly from them. If your MA plan and Part D plan are from different companies, you’ll receive an EOB for each.
What is deductible in insurance?
A deductible is an amount you pay out of pocket before your insurance company covers its portion of your medical bills. For example: If your deductible is $1,000, your insurance company will not cover any costs until you pay the first $1,000 yourself. An EOB is NOT a bill.
What is copayment in insurance?
Copayment: the fixed amount you pay directly to your provider for medical services or prescription drugs covered in your plan. Coinsurance: the percentage of your medical costs that you pay after you meet your deductible; your insurance company pays the remaining amount. Deductible: the amount you pay out of pocket before your insurance company ...
What happens if you don't see your doctor?
This happens any time you see a healthcare provider through your insurance. If you didn’t see your doctor, you probably won’t get an EOB. If you do receive one but haven’t seen a doctor (or filled a prescription) lately, make sure to check it for errors — this can be a helpful tool in spotting fraud on your account.
What is a 20% coinsurance?
For example: If you have a $1,000 medical bill and your coinsurance is 20%, you'll pay $200. Your insurance company will cover the final $800. payments you’ve made and how much you pay toward your deductibles. A deductible is an amount you pay out of pocket before your insurance company covers its portion of your medical bills.
What to do if your Medicare records don't match?
Whenever you see something that does not match up with your records, reach out to your doctor or medical office for clarification. There could have been a misunderstanding or a true billing error. In the worst-case scenario, it could be a sign of Medicare fraud and abuse.
How often do you get a Medicare summary notice?
The Medicare Summary Notice. If you are on Original Medicare (Part A and Part B), you will receive a Medicare Summary Notice (MSN) quarterly, i.e., every 3 months. You will receive separate MSNs for Part A and Part B coverage.
What is an EOB for Medicare?
The document you receive is called an Explanation of Benefits (EOB). Your commercial Medicare plan will mail you an EOB monthly. Similar information will be presented to you as on the Medicare Summary Notice. Like an MSN, an EOB is not a bill.
What is MSN bill?
An MSN is a detailed statement about services that have been charged to Medicare during that time frame but is not a bill in and of itself. THIS IS NOT A BILL will be printed in bold capitalized letters at the top of the statement.
When does a benefit period end?
It ends when you have not received inpatient hospital or skilled nursing facility care for 60 days in a row. You will pay a deductible for each benefit period and multiple deductibles may be listed here.
Who is Ashley Hall?
Ashley Hall is a writer and fact checker who has been published in multiple medical journals in the field of surgery. Learn about our editorial process. Ashley Hall. on December 14, 2020. You do not want to pay more than necessary, but if you don't read your Medicare bill, you could do just that.
What is EOB in medical billing?
Your EOB is a window into your medical billing history. Review it carefully to make sure you actually received the service being billed, that the amount your doctor received and your share are correct, and that your diagnosis and procedure are correctly listed and coded.
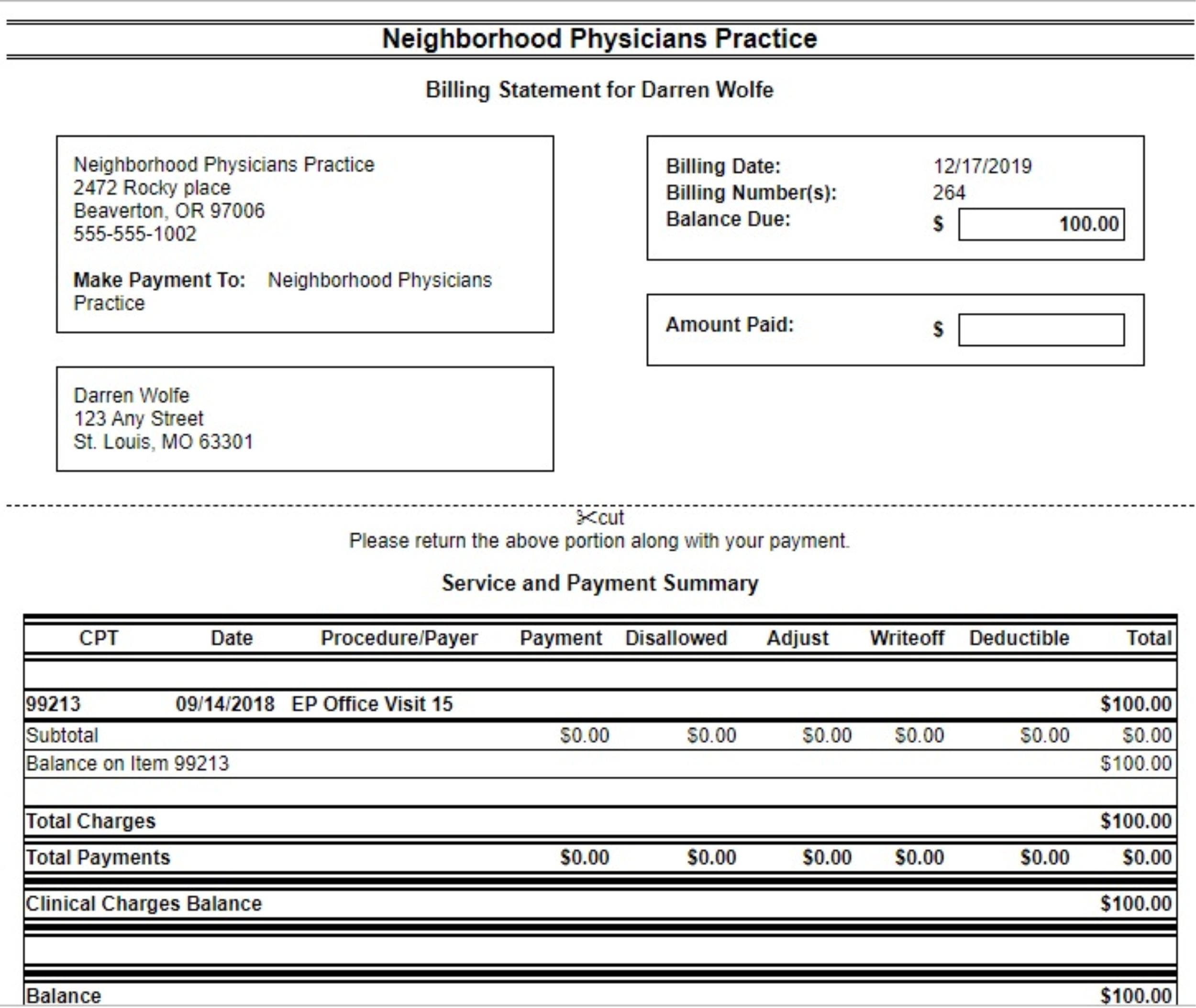
What is billed charge?
Charge (Also Known as Billed Charges): The amount your provider billed your insurance company for the service. Not Covered Amount: The amount of money that your insurance company did not pay your provider. Next to this amount you may see a code that gives the reason the doctor was not paid a certain amount.
What is EOB in healthcare?
Updated on July 19, 2020. An explanation of benefits (EOB) is a form or document provided to you by your insurance company after you had a healthcare service for which a claim was submitted to your insurance plan. Your EOB gives you information about how an insurance claim from a health provider (such as a doctor or hospital) ...
What is EOB in insurance?
An explanation of benefits (EOB) is a form or document provided to you by your insurance company after you had a healthcare service for which a claim was submitted to your insurance plan. Your EOB gives you information about how an insurance claim from a health provider (such as a doctor or hospital) was paid on your behalf—if applicable—and how ...
What is a claim number?
Claim Number: The number that identifies, or refers to the claim that either you or your health provider submitted to the insurance company. Along with your insurance ID number, you will need this claim number if you have any questions about your health plan. Provider: The name of the provider who performed the services for you or your dependent. ...
What is a provider?
Provider: The name of the provider who performed the services for you or your dependent. This may be the name of a doctor, a laboratory, a hospital, or other healthcare providers. Type of Service: A code and a brief description of the health-related service you received from the provider.
How old is Frank F.?
Frank F. is a 67-year-old man with type 2 diabetes and high blood pressure. He is enrolled in a Medicare Advantage Plan and sees his doctor every three months for a follow-up of his diabetes. Six weeks after his last visit, Frank received an EOB with the following information: 1 . Patient: Frank F.
What happens when you receive a medical bill?
Once you receive a medical bill from your healthcare provider, you will notice that it consists of multiple components that might not be clear to you. For most patients, the codes, descriptions, and prices listed in their bills can seem confusing.
How to correct a healthcare billing error?
Contact your healthcare provider’s billing office: Speak to your healthcare provider about bill inaccuracies. If they made an error during the claims process, they should be able to correct it. Take note of the billing representative, the date, and time of your phone call .
What happens if a claim is rejected?
If rejected, the claims processor provides the billing office with a detailed description of why the services are not covered. Your healthcare provider bills you for the remaining balance.
What does EOB mean in medical billing?
EOB stands for explanation of benefits. It is not the same as a medical bill, although it may look similar and show a balance due. When the EOB indicates that money is still owed to the doctor or dentist who provided care, patients can expect a separate bill to be sent from the doctor or dentist’s office.
What does EOB mean in insurance?
When the EOB indicates that money is still owed to the doctor or dentist who provided care, patients can expect a separate bill to be sent from the doctor or dentist’s office. In this instance, payment should be made directly to the practitioner, not to the insurance company who sent the EOB.
What does "not covered" mean in health insurance?
Not Covered: This is the amount your health insurance does not cover. You are responsible for this amount. Reason Code Description: This code provides the reason (s) why your insurer did not cover a charge. Covered by Plan: This is the total amount your health insurance provider has saved you.
What is an 837 file?
They then submit an 837 file to your insurance, the standard file format set by the Health Insurance Portability and Accountability Act ( HIPAA ), allowing your healthcare provider to communicate securely with your insurance.
How does Medicare billing work?
1. Medicare sets a value for everything it covers. Every product and service covered by Medicare is given a value based on what Medicare decides it’s worth.
What happens after a provider treats a Medicare patient?
After a health care provider treats a Medicare patient, the provider sends a bill to Medicare that itemizes the services received by the beneficiary. Medicare then sends payment to the provider equal to the Medicare-approved amount for each of those services.
What does it mean to accept Medicare assignment?
“Accepting assignment” means that a doctor or health care provider has agreed to accept the Medicare-approved amount as full payment for their services. The overwhelming majority of health care providers in the United States accept Medicare assignment.
What happens if a provider doesn't accept Medicare?
If a provider chooses not to accept assignment, they may still treat Medicare patients but will be allowed to charge up to 15 percent more for their product or service. These are known as “excess charges.”. 3.
What percentage of Medicare is coinsurance?
For example, the patient is responsible for 20 percent of the Medicare-approved amount while Medicare covers the remaining 80 percent of the cost. A copayment is typically a flat-fee that is charged to the patient.
Does Medicare cover out of pocket expenses?
Some of Medicare’s out-of-pocket expenses are covered partially or in full by Medicare Supplement Insurance. These are optional plans that may be purchased from private insurance companies to help cover some copayments, deductibles, coinsurance and other Medicare out-of-pocket costs.
What is excess charge?
These are known as “excess charges.”. 3. The provider sends a bill to Medicare that identifies the services rendered to the patient. After a health care provider treats a Medicare patient, the provider sends a bill to Medicare that itemizes the services received by the beneficiary.