Medicare has set up a formal opt-out procedure that your doctor seems to have followed. This includes having you sign a contract acknowledging Medicare won’t pay for his services, and that you won’t submit a claim on your own to either Medicare or Medigap. If you do so, your claim will be denied.
Full Answer
How do I find Medicare providers who have opted out?
Search this database by first name, last name, National Provider Identifier (NPI), specialty, or ZIP code to find providers who've opted out of Medicare. Enter at least one field to start your search. You can also download a national list of providers who’ve opted out of Medicare.
What happens when you opt out of Medicare?
Once you opt out of Medicare, you cannot see any patients under Medicare during each two-year period you have opted out for. If you have been seeing Medicare patients, once you have opted out, they will only be able to continue seeing you under a private contract.
How do I Opt Out of Medicare as a par physician?
( Medicare Participating (PAR) Physicians Scroll down for instructions. Participating physicians’ opt out status only becomes effective at the beginning of a calendar quarter, when the affidavit is sent in at least 30 days before the first day of the quarter.) Step One: Notify your patients that you are opting out of Medicare.
How do I know if my Medicare claim has been approved?
Visit MyMedicare.gov, and log into your account. You’ll usually be able to see a claim within 24 hours after Medicare processes it. Check your Medicare Summary Notice (MSN) . The MSN is a notice that people with Original Medicare get in the mail every 3 months.

How do you know if you're enrolled in Medicare?
How Do I Check the Status of My Medicare Enrollment? The status of your medical enrollment can be checked online through your My Social Security or MyMedicare.gov accounts. You can also call the Social Security Administration at 1-800-772-1213 or go to your local Social Security office.
What does it mean to be opted out of Medicare?
Opt out is a contract between a provider, beneficiary and Medicare where the provider or beneficiary does not file a claim to Medicare. The physician or practitioner bills the beneficiary directly and is not required to follow the fee-for-service charges determined by Medicare.
Can I see Medicare patients if I opt out?
Once you opt out of Medicare, you cannot see any patients under Medicare during each two-year period you have opted out for. If you have been seeing Medicare patients, once you have opted out, they will only be able to continue seeing you under a private contract.
Can I opt back into Medicare?
No. After the initial 90-day period when physicians can change their minds, there is no ability to rejoin the Medicare program until after the two-year period has elapsed.
How often do you have to opt out of Medicare?
two yearsEach opt-out period lasts two years. However, after receiving the initial affidavit, the Centers for Medicare & Medicaid Services (CMS) will automatically renew it every two years unless the physician requests to terminate the opt out at least 30 days before the start of the next two-year period.
Can you opt out of Medicare and Social Security?
So, if you are still working or don't plan on applying for your earned Social Security benefits, you do not have to enroll in Medicare Part A. The problem is that you can't opt out of Medicare Part A and continue to receive Social Security retirement benefits.
What happens if I opt out of Medicare Part B?
Opting out ensures that you don't have to pay Part B premiums or, if you're receiving retirement benefits, have them deducted each month from your Social Security retirement check.
How do I cancel my Medicare opt?
To opt out, you will need to: Submit an opt-out affidavit to Medicare. Enter into a private contract with each of your Medicare patients.
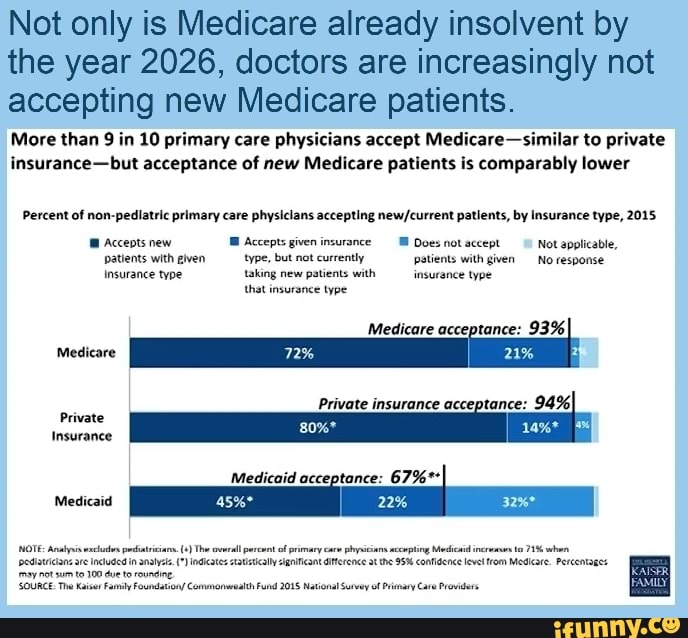
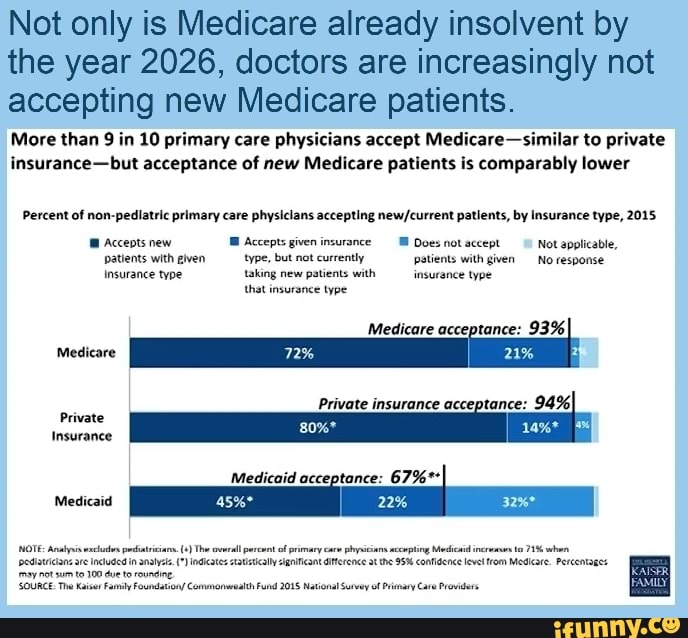
Why do doctors not like Medicare?
Can Doctors Refuse Medicare? The short answer is "yes." Thanks to the federal program's low reimbursement rates, stringent rules, and grueling paperwork process, many doctors are refusing to accept Medicare's payment for services. Medicare typically pays doctors only 80% of what private health insurance pays.
How often do you have to renew a Medicare contract?
Step Six: Mark your calendar to have Medicare patients re-sign a new private contract every two year’s on the anniversary of your opt out effective date. While Physicians opting out on or after June 16, 2015 will no longer need to renew their opt out every two years, CMS currently still requires patients to renew the private contract every two years.
How often do you have to opt out of Medicare?
A silver lining in the Medicare Access and CHIP Reauthorization Act of 2015. which was signed into law in mid-April 2015 to repeal the sustainable growth rate (SGR), is a provision in the bill that also repeals the irritating requirement of having to renew an opt-out status every two years. Physicians opting out of Medicare after June 16, 2015 will need to file an affidavit to opt out of Medicare only once, and it will have permanent effect. The physician will no longer need to renew his opt-out every two years thereafter. However patients will still need to sign a private contract every two-years.
Why should doctors get out of Medicare?
Medicare endangers seniors, rations care and punishes the best doctors whose only aim is to give the best care. For the sake of patients and integrity of the profession , doctors should get out of Medicare. If playback doesn't begin shortly, try restarting your device.
When does opt out become effective?
Participating physicians’ opt out status only becomes effective at the beginning of a calendar quarter, when the affidavit is sent in at least 30 days before the first day of the quarter.) Step One: Notify your patients that you are opting out of Medicare.
How long does a physician have to provide private contracting services?
Subsequent Steps: Follow the above Steps One through Six for a non-participating physician, except that the physician may not provide private contracting services until the first date of the next quarter that is at least 30 days after receipt of the notice by the carrier. For example, the carrier must receive the notice from the physician by Sept. 1 if the physician seeks to provide private contracting services beginning on Oct. 1.
What to do if playback doesn't begin?
If playback doesn't begin shortly, try restarting your device.
Do contractors have to renew opt out?
CMS confirms that contractors must process opt-out renewals submitted prior to opt-out expiration date.
How long does Medicare opt out last?
Previous to June 16, 2015, a physician who opted out of Medicare agreed not to see any Medicare patients (barring emergencies or urgent services), except for those with whom she has entered into private contracts, for a period of two years. As of June 16, 2015, when you opt out, that status will automatically renew every two years unless you inform the Medicare Administrative Contractor for your geographical area within 30 days before the next two-year period begins that you wish to change your status.
How long does it take to opt out of Medicare?
Non-participating physicians may opt out of Medicare at any time. Their continuous two-year opt-out period begins the date the affidavit is signed, provided it is filed with the MAC or Carrier within ten-days after the physician signs his first private contract with a Medicare beneficiary.
What happens if you opt out of Medicare?
This means that if an opted out physician refers a patient to a lab to have blood work done, or to another specialist who has not opted out of Medicare, the services the patient receives as a result of the referral will be covered by Medicare (if they are services that Medicare ordinarily covers).
Can you continue seeing Medicare patients after opting out?
If you have been seeing Medicare patients, once you have opted out, they will only be able to continue seeing you under a private contract. This means any payments from them to you will be out of pocket. Not only will Medicare not reimburse for your services, neither will any supplemental Medigap policies your patients have.
Do you need an affidavit for Medicare?
Physicians who have never enrolled in Medicare, but want to be able to treat Medicare patients under private contracts, must also file an affidavit with the MAC or Carrier that serves their area. These physicians will be provided with a UPIN (Unique Physician Identification Number), based on the physician tax identification number that must be entered on the affidavit.
Can you opt out of Medicare?
Since January 1, 1998, physicians have been permitted to opt out of Medicare and enter into private contracts with Medicare beneficiaries that allow them to set their own fees. If you don’t officially opt out, it is illegal to have Medicare patients pay for your services outside of Medicare. Once you’ve opted out successfully, Medicare will not pay for the care you provide in any setting, for as long as you’re opted out, but you will be able to see Medicare patients and have them pay you based on your private contracts with them.
When do you file affidavits with MAC?
Participating physicians must file their affidavits with their MAC or Carrier at least thirty days before the first date of the next calendar quarter, with the affidavit showing an effective date of the first day of that quarter (i.e., 1/1, 4/1, 7/1, 10/1).
What is PECOS system?
PECOS is the online Medicare enrollment management system which allows you to review information currently on file and withdraw electronically. The PECOS system has print and video tutorials to walk you through different scenarios of withdrawing from Medicare:
What happens if you don't withdraw from Medicare?
Failing to withdraw could result in fraudulent billing or having your Medicare billing privileges revoked.
What is PECOS online?
PECOS is the online Medicare enrollment management system which allows you to:
How long does it take to withdraw from Medicare?
Withdraw from Medicare. If you retire, surrender your license, or no longer want to participate in the Medicare program, you must officially withdraw within 90 days. DMEPOS suppliers must withdraw within 30 days.
What is a private contract with Medicare?
This contract will reflect the agreement between you and your patients that they will pay out of pocket for services, and that nobody will submit the bill to Medicare for reimbursement.
How often does an opt out affidavit renew?
If you’re currently opted out, your opt-out status will automatically renew every two years. If you submitted an opt-out affidavit before June 16, 2015 and never renewed it, you’ll need to submit a new opt-out affidavit.
How to cancel opt out on Mac?
To cancel your opt-out status, you’ll need to mail a cancellation request to your MAC at least 30 days before your opt-out period is set to expire. If you don’t submit your cancellation request before the 30-day period, your opt-out status will automatically renew for another two-year cycle.
What is MSN in Medicare?
The MSN is a notice that people with Original Medicare get in the mail every 3 months. It shows: All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period. What Medicare paid. The maximum amount you may owe the provider. Learn more about the MSN, and view a sample.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
How long does it take to see a Medicare claim?
Log into (or create) your secure Medicare account. You’ll usually be able to see a claim within 24 hours after Medicare processes it. A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare.
What is Medicare Part A?
Check the status of a claim. To check the status of. Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. or.
What is a PACE plan?
PACE plans can be offered by public or private companies and provide Part D and other benefits in addition to Part A and Part B benefits. claims: Contact your plan.
Does Medicare Advantage offer prescription drug coverage?
Medicare Advantage Plans may also offer prescription drug coverage that follows the same rules as Medicare drug plans. Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs.
Is Medicare paid for by Original Medicare?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. or other. Medicare Health Plan. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan.
Should you disenroll from Medicare Part B?
Disenrolling in Medicare Part B isn’t an easy process because it requires an in-person or phone interview. But this is intentional. Canceling Part B could have negative consequences for your wallet (in the form of late-enrollment penalties) and your health (in the form of a gap in coverage).
What to do if you drop Part B?
If you’re dropping Part B because you can’t afford the premiums, remember that you could save money on your health care costs in other ways. Consider adding a Medicare Advantage or Medigap plan instead of dropping Part B. Call us to learn more about these alternatives to disenrolling in Part B.
What is primary payer health plan?
A primary payer health plan pays before Medicare. That means your employer-provided health plan will cover its share of your health care costs first, and if there’s anything left over that Medicare covers, Medicare will pay what remains.
How to schedule an interview with the SSA?
You can schedule an in-person or over-the-phone interview by contacting the SSA. If you prefer an in-person interview, use the Social Security Office Locator to find your nearest location. During your interview, fill out Form CMS 1763 as directed by the representative. If you’ve already received your Medicare card, you’ll need to return it during your in-person interview or mail it back after your phone interview.
What happens if you opt out of Part B?
But beware: if you opt out of Part B without having creditable coverage—that is, employer-sponsored health insurance from your current job that’s as good or better than Medicare—you could face late-enrollment penalties (LEPs) down the line.
Is Medicare a secondary payer?
Conversely, a secondary payer health plan covers only costs left over after Medicare covers its share. If your health plan at work is a primary payer, that’s great. Feel free to drop your Part B coverage if you wish. The Part B premiums might not be worth any additional coverage you receive. But if you have secondary-payer insurance ...
Can Medicare tack late enrollment penalties?
If you have a gap in coverage, the Medicare program could tack late-enroll ment penalties onto your Part B premiums if you re-enroll in coverage again later. Avoid this pitfall by working with your human resources department to ensure that your company's insurance is indeed creditable (meaning that it’s as good or better than Medicare Part B). You may need to provide documentation of creditable coverage during your Part B cancellation interview.